Abstract
Objective:To assess the relationship of specific patient chief physical complaints to underlying depressive symptoms in primary care practice.
Design:A cross-sectional study that was part of a larger prevalence study of depression in primary care.
Setting:A general medical primary care practice in a teaching medical center in rural New England.
Patients:1,042 consecutive outpatients screened for depression with the Hopkins Symptom Checklist 49-item depression scale and for whom physicians filled out a form recording both specific chief complaints and two aspects of complaint presentation style, clarity and amplification.
Interventions:None.
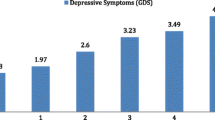
Results:Complaints that discriminated between depressed and non-depressed patients (at the p=0.05 level) were sleep disturbance (PPV 61%), fatigue (PPV 60%), multiple (3+) complaints (PPV 56%), nonspecific musculoskeletal complaints (PPV 43%), back pain (PPV 39%), shortness of breath (PPV 39%), amplified complaints (PPV 39%), and vaguely stated complaints (PPV 37%).
Conclusions:Depressed patients are common in primary care practice and important to recognize. Certain specific complaints and complaint presentation styles are associated with underlying depressive symptoms.
Similar content being viewed by others
References
Klerman GL, Weissman MM. Increasing rates of depression. JAMA. 1989;261:2229–334.
Barrett JE, Barrett JA, Oxman TE, Gerber PD. The prevalence of psychiatric disorders in a primary care practice. Arch Gen Psychiatry 1988;45:1100–6.
Regier DA, Goldberg ID, Taube CA. The de factor U.S. mental health service septem: a public health perspective. Arch Gen Psychiatry. 1978:35:685–93.
Nielsen A, Williams T. Depression in ambulatory medical patients. Arch Gen Psychiatry 1980;37:999–1004.
Zung W, Magill M, Moore J, Georges D. Recognition and treatment of depression in a family practice. J Clin Psychiatry. 1983;44:3–6.
Parker G, Holmes S, Manicevasagar V. Depression in general practice attenders: casiness, natural history, and predictors of outcome. J Affective Disord. 1986;10:27–8.
Myers JK, Weisman MM, Tischler GL, et al. The prevalence of psychiatric disorders in three communities, 1980–1982. Arch Gen Psychiatry. 1984;41:959–67.
Goldberg ID, Bahigian HM, Locke BA, Rosen EM. Role of nonpsychiatrist physicians in the delivery of mental health services: implications from three studies. Public Health Rep. 1978;92(3):240.
Jones L, Badger L, Ficken R, Leeper J, Anderson R. Inside the modern mental health network. Examining mental health care delivery of primary care physicians. Gen Hosp Psychiatry. 1987;9:287–93.
Gerber PD, Barrett J, Barrett J, Manheimer E, Whiting R, Smith R. Recognition of depression by internists in primary care: a comparison of internist and “gold standard” psychiatric assessments. J Gen Intern Med 1989;4:7–13.
Mark SJ, Goldberg D, Hillier V. Determinants of the ability of general practitioners to detect psychiatric illness. Psychol Med. 1979;9:337–53.
Goldberg D, Steele J, Johnson A, Smith C. Ability of primary care physicians to make accurate ratings of psychiatric symptoms. Arch Gen Psychiatry. 1982;39:829–33.
PR Jencks SF. Recognition of mental distress and diagnosis of mental disorder in primary care. JAMA. 1985;253:1903–7.
German PS, Shapiro S, Skinner EA, et al. Detection and management of mental health problems of older patients by primary care providers. JAMA. 1987;257:489–93.
Prestidge BR, Lake CR. Prevalence and recognition of depression among primary care outpatients. J Fam Pract. 1987;25:67–72.
Schulberg HC, McClelland M. A conceptual model for educating primary care providers in the diagnosis and treatment of depression. Gen Hosp Psychiatry. 1987;9:1–10.
Widmer RB, Cadoret RJ, North CS. Changes in pattern of patient visits and complaints during a developing depression. J Fam Pract. 1978;7:293–302.
Wilson DR, Widmer RB, Cadoret RJ, Judiesch K. Somatic symptoms, a major feature of depression in a family practice. J Affective Disord. 1983;5:199–207.
Stoeckle JD, Zola IK, Davidson GE. The quantity and quality of psychological distress in medical patients. J Chron Dis. 1964;17:959–70.
Lipman RS, Covi L, Shapiro AK. The Hopkins Symptoms Checklist (HSCL): factors derived from HSCL-90. J Affective Disord. 1979;1:9–24.
Spitzer RS, Endicott J, Robins E. Research diagnostic criteria for a selected group of functional disorders. New York: Biometrics Research, New York State Psychiatric Institute, 1975.
Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. JAMA. 1989;262:1479–84.
Kroenke K, Wood DR, Maugelsdorff AD, Meier NJ, Powell JB. Chronic fatigue in primary care. JAMA. 1988;260:929–34.
Manu P, Mathews DA, Lane TJ. The mental health of patients with a chief complaint of chronic fatigue. Arch Intern Med. 1988;148:2213–7.
Katon W, Kleinman A, Rosen G. Depression and somatization: A review. Part I. Am J Med. 1982;72:127–35.
Katon W, Kleinman A, Rosen G. Depression and somatization: a review. Part II. Am J Med. 1982;82:214–7.
Barsky AJ. Patients who amplify bodily sensations. Ann Intern Med. 1979;91:63–70.
Katon W, Ries RK, Kleinman A. The prevalence of somatization in primary care. Compr Psychiatry. 1984;25:208–15.
Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145(11):1358–66.
Kirmayer LJ. Culture, affect and somatization. Transcultural Psychiatr Res Rev. 1984;21:159–88.
Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA. 1989;262:914–9.
Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. HAMA. 1990;264:2524–8.
Anda RF, Williamson DE, Escobero LG, et al. Depression and the dynamics of smoking. JAMA. 1990;264:1541–5.
Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation and major depression. JAMA. 1990;264:1546–9.
Author information
Authors and Affiliations
Additional information
Received from the Section of General Internal Medicine, Department of Medicine, and the Department of Community and Family Medicine, Dartmouth Medical School, Hanover, New Hampshire.
Supported by NIMH Grant No. MH-3752.
Rights and permissions
About this article
Cite this article
Gerber, P.D., Barrett, J.E., Barrett, J.A. et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med 7, 170–173 (1992). https://doi.org/10.1007/BF02598007
Issue Date:
DOI: https://doi.org/10.1007/BF02598007