Abstract
Aims/hypothesis
Insulin resistance and insulin deficiency are proposed as risk factors for IGT and type 2 diabetes. We assessed the predictive value of initial parameters for the outcome of an OGTT performed 24.3±2.9 years later in an unselected healthy non-obese population.
Methods
The K-value of an IVGTT was determined in 267 healthy subjects (mean±SD: age 31.0±12.0 years, BMI 21.8±2.8 kg/m2). First-phase insulin response to a glucose infusion test was estimated as an incremental 5- or 10-min (ΔI5 or ΔI10) value, and as insulinogenic indices (ΔI5/ΔG5 or ΔI10/ΔG10) adjusted for insulin sensitivity determined by homeostasis model assessment for insulin resistance ([ΔI5/ΔG5]/HOMA-IR).
Results
At follow-up, six subjects had type 2 diabetes and 47 had IGT; 214 retained normal glucose tolerance. Insulin sensitivity and early (30 min) insulin response decreased with decreasing outcome OGTT. Blood glucose (2 h) at OGTT correlated positively with initial age and BMI, and negatively with ΔI5/ΔG5, (ΔI5/ΔG5)/HOMA-IR and K-value. In multiple linear regression analysis, (ΔI5/ΔG5)/HOMA-IR, ΔI10, K-value, age, HOMA estimate of insulin secretion, and fasting plasma glucose were significantly associated with 2-h OGTT blood glucose. Similar results were obtained on comparing differences between subjects with normal and decreased (IGT+diabetes) glucose tolerance.
Conclusions/interpretation
In 267 non-obese healthy subjects, initial K-value and first-phase insulin response to glucose adjusted for insulin sensitivity, but not insulin sensitivity itself, were strong predictors of the outcome of an OGTT performed 25 years later. Thus, in contrast to obese or other high-risk populations, in lean subjects, decreased beta cell function, but not insulin resistance itself, determines future glucose tolerance.
Similar content being viewed by others
Introduction
Type 2 diabetes develops through interaction between heredity and environment [1]. The disease evolves from a hypothetical prediabetic phase through IGT. IGT and type 2 diabetes are characterised by decreased insulin release and insulin resistance [2–4]. As regards prediabetes, contradictory data have been presented indicating that impaired insulin response to glucose [4–6], decreased peripheral insulin sensitivity [7], or a combination of both [8–10], is the primary marker.
The objective of this study was to characterise the initial parameters that predicted the outcome of an OGTT at long-term follow-up in a normal, healthy population. Emphasis was placed on clarifying the predictive role of glucose tolerance and insulin responsiveness in this regard. At the initiation of the study, glucose tolerance was assessed by calculating the glucose disappearance rate (K-value) after i. v. administration of glucose (IVGTT). Insulin responsiveness was measured using a glucose infusion test, which was designed to evaluate both first-and second-phase insulin responses to glucose [11]. Fasting plasma glucose and insulin during the glucose infusion test were used to assess insulin resistance and beta cell function by homeostasis model assessment (HOMA).
Subjects and methods
Subjects
Subjects (n=319) were recruited between 1963 and 1981. They were mainly healthy Swedish blood donors with a normal IVGTT, defined as K-value ≥1.0%/min. Forty-one subjects were lost to follow-up. Nine had developed diabetes during the follow-up (two had developed type 1 diabetes) and did not participate in the final OGTT. Thus, 269 subjects underwent an OGTT at the end of the study. However, two subjects showed signs of autoimmune diabetes and were excluded from further analyses. The protocol was approved by the ethics committee of Karolinska Hospital.
The sample consisted of 152 male and 115 female subjects, who were aged 6–64 years (mean±SD 31.0±12.0) at the start of study and had a BMI of 13.0–30.0 kg/m2 (mean±SD 21.8±2.8). Age at OGTT was 55.6±10.7 years (mean±SD) and duration of follow-up was 24.3±2.9 years (mean±SD). None of the subjects were receiving medication.
The IVGTT
Glucose (25 g) was injected rapidly as a 25% solution. Capillary blood glucose was measured every 5 min for 70 min, and values plotted semi-logarithmically against time. The near-straight line obtained after a 25-min equilibration period was used to calculate the K-value (%/min), i.e. the disappearance rate of glucose [12].
The glucose infusion test
A 25% glucose solution (500 mg/kg body weight) was injected rapidly; this was followed by infusion of a 15% glucose solution at a rate of 20 mg kg−1 min−1 for 60 min [11]. Venous blood samples were drawn at 5–20-min intervals over 120 min for determination of blood glucose and plasma insulin.
Estimates obtained during the glucose infusion test
The HOMA for beta cell function (HOMA-β) and insulin resistance (HOMA-IR) were calculated from fasting plasma glucose and insulin concentrations [13]. Incremental plasma insulin (ΔI5) and blood glucose (ΔG5) responses were calculated as the difference between the value baseline and the value at 5 min after initiation of glucose injection. The ratio of incremental insulin to glucose responses (ΔI5/ΔG5; insulinogenic index) was used as a measure of beta cell function. Insulin sensitivity is a critical modulator of the insulin response [14]; we therefore adjusted ΔI5/ΔG5 for insulin sensitivity by dividing it by HOMA-IR ([ΔI5/ΔG5]/HOMA-IR). Other estimates used were incremental insulin concentration (ΔI10) and insulinogenic index at 10 min (ΔI10/ΔG10).
The OGTT
Glucose (75 g) was dissolved in 250 ml water. Results were interpreted according to World Health Organization criteria [15] for venous blood glucose.
Estimates obtained during OGTT
Incremental plasma insulin (ΔI30) and blood glucose (ΔG30) responses were calculated as difference between baseline and values at 30 min after glucose intake. The ratio of the incremental insulin to glucose response (ΔI30/ΔG30) was adjusted for insulin sensitivity by dividing with the HOMA-IR ([ΔI30/ΔG30]/HOMA-IR).
Assays
Glucose was measured in whole blood and plasma with glucose oxidase. In samples from the glucose infusion test, plasma insulin was determined by radioimmunoassay, using charcoal to separate antibody-bound and free insulin. A double-antibody radioimmunoassay was used to determine plasma insulin in venous samples from the OGTT. All diabetic subjects were tested for GAD antibodies.
Statistical analysis
Statistical analysis was performed using STATISTICA, version 6.0 (StatSoft, Tulsa, OK, USA). Data are presented as means±SEM unless stated otherwise. Analyses were performed after logarithmical transformation of skewed variables. Correlations between 2-h blood glucose at OGTT and other variables were assessed using Spearman’s rank correlation coefficient, while simple linear regression analysis was performed after logarithmic transformation of the data. The χ 2 test was used to test for sex differences between the groups with NGT and decreased glucose tolerance (DGT; this group includes those with IGT and those with diabetes). The Mann–Whitney U-test was performed to compare the NGT and DGT groups. The Kruskal–Wallis test was used to compare the NGT, IGT and diabetic groups. Multiple linear regression analysis was performed with variables assessed at the start of the study used as covariates and 2-h blood glucose during the OGTT used as the dependent variable. A similar analysis was performed with glucose tolerance (DGT vs NGT) used as the dependent variable in multiple logistic regression. The models were checked by inspection of residuals. Several variables in the univariate analyses were derived variables and most were excluded from the multivariate analyses due to multicollinearity. A p value less than 0.05 was regarded as statistically significant.
Results
Cross-sectional study: results of OGTT at follow-up
According to the OGTT at follow-up, of the 269 subjects with no previously known diabetes, eight had developed diabetes (3%), 47 had developed IGT (17.5%) and 214 showed NGT. Two diabetic patients tested positive for GAD antibodies and were excluded from analyses. The groups with diabetes and IGT were combined into a common group, DGT (19.9%).
The characteristics of the subjects at the end of follow-up are shown in Table 1. Sex did not correlate with glucose tolerance. Age, BMI, WHR and systolic and diastolic blood pressure were higher in groups with decreased glucose tolerance.
Current insulin responsiveness and sensitivity were estimated as previously described [4]. Insulin sensitivity (Fig. 1a) and early insulin response (Fig. 1b) decreased with decreasing glucose tolerance. The deteriorating insulin secretion capacity was more pronounced when beta cell function was adjusted according to insulin sensitivity (Fig. 1c).
Insulin resistance determined by HOMA-IR (a) and beta cell function, quantified as ΔI30/ΔG30 (b) and (ΔI30/ΔG30)/HOMA-IR (c), from an OGTT in subjects with NGT (n=214), IGT (n=47) or diabetes (n=6). Definitions of the estimates are provided in the main text. Thepvalues are for Mann–Whitney U-tests of differences between the different glucose tolerance groups
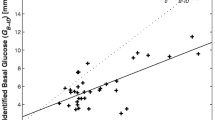
Longitudinal study: correlation of 2-h blood glucose at outcome OGTT with variables measured at inclusion
There were significant positive correlations with age and BMI, and a negative correlation with K-value. Importantly, first-phase insulin response during the glucose infusion test (ΔI5/ΔG5 and [ΔI5/ΔG5]/HOMA-IR) correlated negatively with OGTT (Table 2). The strength of the correlation was similar for the significantly associated variables. Similar results were obtained when analysing correlations for the logarithmically transformed variables (data not shown). The 2-h blood glucose value did not differ between sexes.
Multiple linear regression analysis was performed with OGTT 2-h blood glucose as the dependent variable. The best subset variable selection method was used, with all variables from Table 2, together with sex, as possible predictor variables in the model. The associated variables were, in descending order of significance: (ΔI5/ΔG5)/HOMA-IR, ΔI10, K-value, age, HOMA-β and fasting plasma glucose (Table 3). Adjusted R 2 for the best subset model was 0.123, p<0.001. There was no multicollinearity problem in this model.
Differences in inclusion variables between outcome NGT and DGT groups
The same initial variables that correlated significantly to 2-h blood glucose (Table 2) also differed significantly between the NGT and DGT groups, except ΔI5/ΔG5 (Table 4). Thus, at the beginning of the study, subjects who developed DGT were older and had a higher BMI. They also had a lower K-value and (ΔI5/ΔG5)/HOMA-IR. Logarithmically transformed variables gave similar results (data not shown). There were no sex differences related to outcome glucose tolerance.
In multiple logistic regression analysis with glucose tolerance as the dichotomous outcome variable (DGT vs NGT), we used predictor variables established with the best subset variable selection method in multiple linear regression analysis. Starting with all possible predictor variables did not work efficiently in the logistic regression analysis due to multicollinearity. The associated variables were, in descending order of significance: ΔI10, (ΔI5/ΔG5)/HOMA-IR, K-value, HOMA-β, fasting plasma glucose and age (Table 5). The p value for the log likelihood ratio test of goodness-of-fit was <0.001 for the ‘best subset’ model, and R 2 logit was 0.125. Importantly, similar results were obtained in logistic regression analysis when the seven subjects who developed type 2 diabetes during follow-up were included.
Discussion
The 30-year controversy on whether type 2 diabetes is a disorder of reduced insulin action or diminished insulin secretion is abating, with most investigators accepting that diminished insulin secretion is a necessary condition for the development of impaired glucose homeostasis [3, 16–18]. The main reason for underestimating the deficit in insulin secretion is failure to recognise the modulating effect of insulin sensitivity on beta cell function [14]. When this was taken into consideration it became evident that subjects at high risk of subsequently developing type 2 diabetes have a diminished insulin-releasing capacity. Thus, reduced first-phase insulin response to i.v. glucose was demonstrated in first-degree relatives of type 2 diabetes [5], women with a history of present or previous gestational diabetes [19, 20], women with polycystic ovary syndrome [21], subjects with cystic fibrosis [22], older subjects [23] and subjects with IGT [24]. These more recent findings provide strong support for our suggestion from four decades ago that subjects with a decreased insulin response to glucose (especially those with a low first-phase response, then labelled prediabetics) are at risk of developing type 2 diabetes when additional factors later in life, such as insulin resistance, demand a major increase in insulin output [25, 26]. The present investigation was initiated to verify this hypothesis in subjects belonging to a population in which these early observations were made.
Twenty-five years of follow-up enabled us to compare insulin responsiveness and sensitivity in subjects who maintained NGT with those who developed IGT or type 2 diabetes. We used simple measures of beta cell function during OGTT, such as incremental plasma insulin at 30 min (ΔI30), alone or related to the corresponding glucose increment (ΔI30/ΔG30, known as the insulinogenic index), which is a better parameter of beta cell sensitivity to glucose [27]. However, normalising the insulinogenic index to the insulin sensitivity of the subject ([ΔI30/ΔG30]/HOMA-IR) provides the best physiological parameter for characterising beta cell responsiveness to glucose [4]. The use of an early time point (30 min) is important, since it is well correlated to first-phase insulin secretion and is probably regulated by similar beta cell mechanisms. For example, the acute insulin response to i.v. glucose correlated with the insulinogenic index of OGTT at 30 min in Pima Indians [28]. We found similar correlations in lean subjects with normal vs reduced first-phase insulin response to the glucose infusion test [29].
The present cross-sectional study confirms the results of Jensen et al. [4] that both insulin secretion and insulin sensitivity decrease with decreasing glucose tolerance. Since neither the insulinogenic index nor the HOMA-IR were normally distributed, it was not possible to evaluate the relative importance of these parameters for deterioration of glucose tolerance from NGT to IGT to type 2 diabetes.
The main interest of this investigation lies in the analysis of predictive factors for glucose intolerance assessed 25 years earlier in a non-obese and non-high-risk population. The subjects were young at recruitment and were only about 55 years old at final OGTT. This may explain why age was not strongly correlated with outcome in the longitudinal study. Furthermore, initial body weight was normal, with very few overweight persons (none with a BMI>30.0 kg/m2 and only 14 of 267 with a BMI>26.0 kg/m2); therefore, BMI was not strongly correlated with outcome in this study. Another explanation, corroborated in the multivariate analyses, is that age and BMI have little or no independent effect on glucose tolerance, but act mainly by decreasing insulin secretion and insulin sensitivity. The heredity of diabetes could be assessed in only 181 subjects. It appeared that about 30% of the subjects had at least one first- or second-degree relative with diabetes. This is the expected prevalence in a Swedish population of similar age [30].
The predictive power of fasting plasma glucose for future diabetes has recently been summarised in a consensus statement published by the International Diabetes Federation [31]: in six studies from different populations without diabetes, the group with IFG accounted for 9–64% of future diabetes cases. Of our subjects, only six had initial fasting plasma glucose in the IFG range (6.1–6.9 mmol/l); only one developed IGT 25 years later. Thus, in our population, fasting glucose was not a strong predictor. In contrast, in all analyses, the K-value was constantly a predictor of final glucose tolerance. To our knowledge there is only one earlier long-term study of the predictive power of the K-value: Warram et al. showed that decreased glucose removal rate was an independent risk factor for developing diabetes among the offspring of diabetic parents [7]. Our study shows that this is also true in subjects recruited from the general population, even when they are overwhelmingly non-obese and lack other diabetes risk factors. The K-value has been described as an integral measure of simultaneous changes in hepatic glucose output and peripheral glucose removal, both of which are modified by insulin release [32]. Indeed, it has been shown by Thorell [33], as well as by us [34], that the K-value is closely correlated with glucose-induced first-phase insulin secretion, while the correlation with insulin sensitivity is weaker [34]. It is therefore not surprising that, in the univariate analyses of the 2-h blood glucose concentrations at the final OGTT, the only significantly associated estimates besides the K-value were ΔI5/ΔG5 and, especially, (ΔI5/ΔG5)/HOMA-IR, both of which are estimates of first-phase insulin response to glucose. Irrespective of whether this was assessed as ΔI5/ΔG5 or corrected for insulin sensitivity ([ΔI5/ΔG5]/HOMA-IR), there was a consistent tendency for lower insulin responses in the group of subjects who developed DGT 25 years later (Table 4). We conclude from these results that the first-phase insulin response is an important predictor of future glucose tolerance, and suggest that in subjects at risk of developing IGT and diabetes, the beta cells have a reduced ability to respond rapidly to acute challenges.
A finding that seems surprising at first glance and in contradiction to the above discussion, is the positive correlation between the 10-min glucose infusion test insulin response (ΔI10) and future glucose intolerance (Tables 3 and 5). What differs between 5 and 10 min during the ‘square-wave’ glucose stimulation of the pancreas during the glucose infusion test? While insulin values at 5 min correspond to first-phase insulin release, the 10 min sample reflects the beginning of second-phase secretion. We have previously demonstrated that second-phase insulin release is a function of so-called time-dependent potentiation (TDP) or glucose priming, which works via a mechanism different from the insulin secretion-initiating effect of the sugar [35, 36]. Of greater relevance to this study, previous work demonstrated that healthy subjects with a low insulin response to glucose or IGT exhibit enhanced TDP [37]. By this mechanism, beta cells try to compensate for the impaired initiatory effect of glucose on insulin secretion and maintain substantial late (second-phase) insulin responses until the advanced stages of type 2 diabetes.
Insulin sensitivity in itself had no predictive value for IGT and type 2 diabetes in the present follow-up, in contrast to several studies in the literature: in Pima Indians [38] and Hispanics [9], not only insulin responsiveness, but also insulin sensitivity was of major significance for development of IGT and type 2 diabetes. Why this difference? Both Pima Indians and Hispanics are populations with a very high prevalence of obesity. The subjects included in our study were of Swedish origin, non-obese and mostly physically fit; thus, in such a ‘low-risk’ population the confounding effect of obesity-related insulin resistance seems to be eliminated, permitting the unravelling of the importance of the underlying beta cell deficiency for the development of IGT. It could be claimed that HOMA-IR is not sensitive enough to disclose subtle alterations in insulin sensitivity. However, comparison of HOMA with the hyperinsulinaemic–euglycaemic clamp, which is the gold standard for measuring insulin sensitivity, revealed high and significant correlation, r≈0.80 [39]. Furthermore, in a previous study in type 2 diabetes patients with similar phenotype, insulin sensitivity determined with hyperinsulinaemic–euglycaemic clamps was normal [40]. Finally, while in vitro insulin sensitivity in muscle biopsies from patients with type 2 diabetes was decreased, it was normalised after long-term preincubation in a medium of normal glucose concentration [41]. Hence, rather than being a primary defect, it seems that the insulin resistance of these patients is secondary to hyperglycaemia, probably as a result of glucose-induced downregulation of glucose transport in muscle [42].
In conclusion, 20% of 267 healthy subjects with normal intravenous glucose tolerance developed decreased oral glucose tolerance 25 years later. Both initial K-value and first-phase insulin response to glucose, corrected for insulin sensitivity ([ΔI5/ΔG5]/HOMA-IR), were consistent strong predictors of glucose tolerance at the end of follow-up. K-value is mainly controlled by first-phase insulin secretion. We therefore believe that a first-phase insulin response that is inadequate for the insulin sensitivity of the subject is an important risk factor for developing IGT and type 2 diabetes. Thus, this study supports the hypothesis that subjects with low insulin response are at risk of developing diabetes [26].
Abbreviations
- DGT:
-
decreased glucose tolerance
- HOMA-β:
-
homeostatic model assessment of insulin secretion
- HOMA-IR:
-
homeostasis model assessment of insulin resistance
- TDP:
-
time-dependent potentiation
References
Kahn CR (1994) Insulin action, diabetogenes, and the cause of type II diabetes. Diabetes 43:1066–1084
Efendic S, Luft R, Wajngot A (1984) Aspects of pathogenesis of type 2 diabetes. Endocr Rev 5:395–410
DeFronzo RA, Bonadonna RC, Ferrannini E (1992) Pathogenesis of NIDDM: a balanced overview. Diabetes Care 15:318–368
Jensen CC, Cnop M, Hull RL, Fujimoto WY, Kahn SE, American Diabetes Association GENNID Study Group (2002) β-Cell function is a major contributor to oral glucose tolerance in high-risk relatives of four ethnic groups in the US. Diabetes 51:2170–2178
Pimenta W, Korytkowski M, Mitrakou A et al (1995) Pancreatic beta-cell dysfunction as the primary genetic lesion in NIDDM. Evidence from studies in normal glucose-tolerant individuals with a first-degree NIDDM relative. J Am Med Assoc 273:1855–1861
Kadowaki T, Miyake Y, Hagura R et al (1984) Risk factor for worsening to diabetes in subjects with impaired glucose tolerance. Diabetologia 26:44–49
Warram J, Martin B, Krolewski A, Soeldner S, Kahn RC (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic patients. Ann Intern Med 113:909–915
Lillioja S, Mott DM, Spraul M et al (1993) Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. Prospective studies of Pima Indians. N Engl J Med 329:1988–1992
Haffner SM, Miettinen H, Gaskill SP, Stern MP (1995) Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican–Americans. Diabetes 44:1386–1391
Eriksson J, Franssila-Kallunki A, Ekstrand A et al (1989) Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus. N Engl J Med 321:337–343
Cerasi E, Luft R (1967) The plasma insulin response to glucose infusion in healthy subjects and in diabetes mellitus. Acta Endocrinol (Copenh) 55:287–304
Ikkos D, Luft R (1957) On the intravenous glucose tolerance test. Acta Endocrinol (Copenh) 25:312–334
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Kahn SE, Prigeon RL, McCulloch DK et al (1993) Quantification of the relationship between insulin sensitivity and β-cell function in human subjects: evidence for a hyperbolic function. Diabetes 42:1663–1673
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (1997) Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20:1183–1197
Cerasi E (1995) Insulin deficiency and insulin resistance in the pathogenesis of type 2 diabetes: is a divorce possible? Diabetologia 38:992–997
Cavaghan MK, Ehrman DA, Polonsky KS (2000) Interactions between insulin resistance and insulin secretion in the development of glucose intolerance. J Clin Invest 106:329–333
Kahn SE (2001) The importance of β-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab 86:4047–4058
Catalano PM, Tyzbir ED, Wolfe RR et al (1993) Carbohydrate metabolism during pregnancy in control subjects and women with gestational diabetes. Am J Physiol 264:E60–E67
Efendic S, Hanson U, Persson B, Wajngot A, Luft R (1987) Glucose tolerance, insulin release, and insulin sensitivity in normal-weight women with previous gestational diabetes mellitus. Diabetes 36:413–419
Dunaif A, Finegood DT (1996) β-Cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome. J Clin Endocrinol Metab 81:942–947
Austin A, Kalhan SC, Orenstein D, Nixon P, Arslanian S (1994) Roles of insulin resistance and β-cell dysfunction in the pathogenesis of glucose intolerance in cystic fibrosis. J Clin Endocrinol Metab 79:80–85
Kahn SE, Larson VG, Schwartz RS et al (1992) Exercise training delineates the importance of beta-cell dysfunction to the glucose intolerance of human aging. J Clin Endocrinol Metab 74:1336–1342
Larsson H, Ahrén B (1996) Failure to adequately adapt reduced insulin sensitivity with increased insulin secretion in women with impaired glucose tolerance. Diabetologia 39:1099–1107
Cerasi E, Luft R (1963) Plasma-insulin response to sustained hyperglycaemia induced by glucose infusion in human subjects. Lancet ii:1359–1361
Cerasi E, Luft R (1967) “What is inherited–what is added?” hypothesis for the pathogenesis of diabetes mellitus. Diabetes 16:615–627
Phillips DIW, Clark PM, Hales CN, Osmond C (1994) Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med 11:286–292
Pratley RE, Weyer C (2001) The role of impaired early insulin secretion in the pathogenesis of type II diabetes mellitus. Diabetologia 44:929–945
Cerasi E, Luft R (1967) Further studies on healthy subjects with low and high insulin response to glucose infusion. Acta Endocrinol (Copenh) 55:305–329
Grill V, Persson G, Carlsson S et al (1999) Family history of diabetes in middle-aged Swedish men is a gender unrelated factor which associates with insulinopenia in newly diagnosed diabetic subjects. Diabetologia 42:15–23
Unwin N, Shaw J, Zimmet P, Alberti KGMM (2002) Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 19:708–723
Moorhouse JA, Grahame GR, Rosen NJ (1964) Relationship between intravenous glucose tolerance and the fasting blood glucose levels in healthy and in diabetic subjects. J Clin Endocrinol Metab 24:145–159
Thorell JI (1973) Effect of transient elevation of plasma insulin within physiological levels (simulated early insulin response) on blood glucose. J Clin Endocrinol Metab 37:423–430
Efendic S, Cerasi E, Elander I et al (1979) Studies on low insulin responders. Glucose tolerance and insulin response to intravenous and oral glucose challenges in 226 normal subjects and 25 subjects with mild or chemical diabetes. Acta Endocrinol Suppl (Copenh) 224:5–32
Grill V, Adamson U, Cerasi E (1978) Immediate and time-dependent effects of glucose on insulin release from rat pancreatic tissue; evidence for different mechanisms of action. J Clin Invest 61:1034–1043
Nesher R, Cerasi E (2002) Modeling phasic insulin release: immediate and time-dependent effects of glucose. Diabetes 51:S53–S59
Cerasi E (1975) Potentiation of insulin release by glucose in man. III. Normal recognition of glucose as a potentiator in subjects with low insulin response and in mild diabetes. Acta Endocrinol (Copenh) 79:511–534
Weyer C, Tataranni PA, Bogardus C, Pratley RE (2000) Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care 24:89–94
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27:1487–1495
Arner P, Pollare T, Lithell H (1991) Different aetiologies of type 2 (non-insulin-dependent) diabetes mellitus in obese and non-obese subjects. Diabetologia 34:483–487
Zierath JR, Krook A, Wallberg-Henriksson H (1998) Insulin action in skeletal muscle from patients with NIDDM. Mol Cell Biochem 182:153–160
Sasson S, Edelson D, Cerasi E (1987) In vitro autoregulation of glucose utilization in the rat soleus muscle. Diabetes 36:1041–1046
Acknowledgements
The authors are grateful to the nurses and technicians of the Endocrine Laboratory at the Karolinska Hospital. These studies were supported by grants from The Swedish Research Council (K2003-72B1-14624-01A) and Novo Nordisk Foundation Consortium on Vascular Complications in Diabetes.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is dedicated to Rolf Luft, our mentor and collaborator over several decades, on the occasion of his 90th birthday.
Rights and permissions
About this article
Cite this article
Alvarsson, M., Wajngot, A., Cerasi, E. et al. K-value and low insulin secretion in a non-obese white population: predicted glucose tolerance after 25 years. Diabetologia 48, 2262–2268 (2005). https://doi.org/10.1007/s00125-005-1929-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1929-6