Abstract
Aims/hypothesis
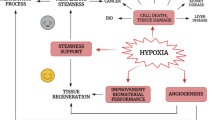
A reduction in the number of endothelial progenitor cells (EPCs) is considered a plausible cause of increased cardiovascular risk in diabetes mellitus. The aim of this study was to test the hypothesis that weak bone marrow mobilisation is responsible for the decrease in circulating EPCs in diabetes.
Materials and methods
We employed a model of hindlimb ischaemia–reperfusion (I/R) injury to study mobilisation of EPCs in control and streptozotocin diabetic rats. EPCs were defined by flow cytometry as Sca-1+ and Sca-1+c-kit+ peripheral blood cells and further characterised by the expression of CD31, von Willebrand factor and fetal liver kinase-1. Capillary density was evaluated by immunofluorescent staining of vWF. We also determined plasma levels of stromal cell-derived factor (SDF-1) and vascular endothelial growth factor (VEGF) by ELISA and muscle expression of hypoxia-induced factor (HIF-1α) by Western blotting.
Results
In control rats, EPCs showed a mobilisation curve within 7 days, while diabetic rats were completely unable to mobilise EPCs after I/R injury. As a consequence, diabetic rats showed no compensatory increase in muscle capillary density. Defective EPC mobilisation in diabetes was associated with altered release of SDF-1 and VEGF and inability to upregulate muscle HIF-1α. Both insulin administration and premedication with granulocyte-colony stimulating factor and stem cell factor led to partial recovery in post-ischaemic mobilisation of EPCs in diabetic rats.
Conclusions/interpretation
Defective ischaemia-induced bone marrow mobilisation of EPCs impedes compensatory angiogenesis in ischaemic tissues of diabetic animals. Growth factor administration together with blood glucose control may offer a rational therapeutic strategy for diabetic ischaemic syndromes.
Similar content being viewed by others
Introduction
Diabetes mellitus is characterised by an excess of cardiovascular disease and mechanisms involved in the pathogenesis of macrovascular complications include an impaired angiogenic response to ischaemia [1]. Endothelial progenitor cells (EPCs) have been identified as circulating precursors of adult neovasculogenesis and vascular homeostasis [2]; they reside in the bone marrow and are mobilised to the peripheral blood upon many stimuli, including tissue ischaemia and the local release of cytokines and growth factors [3]. Recent data have demonstrated that reduced numbers of circulating EPCs predict cardiovascular events in patients with coronary artery disease [4, 5] and that EPC mobilisation after myocardial infarction parallels modifications of ventricular function during the follow-up [6]. Diabetes mellitus is characterised by a reduction in the number of circulating EPCs and we have shown that a decrease in the number of EPCs is related to the worsening of peripheral vascular complications [7]. We hypothesise that defective mobilisation of EPCs in response to ischaemia accounts for the very low levels of EPCs in the peripheral blood of diabetic patients, and determines the severely impaired compensatory collateralisation that is typical of diabetic vasculopathy. In this study, we employed a model of ischaemia–reperfusion (I/R) injury in control and streptozotocin-induced diabetic rats to test this hypothesis. Specifically, the aim was to evaluate whether the reduction in the number of EPCs in diabetes is attributable to impaired mobilisation in response to ischaemia and/or growth factors. We also explored whether lowering the concentration of glucose in the blood during I/R injury and premedication with haematopoietic growth factors significantly influence EPC mobilisation in diabetic rats.
Materials and methods
Animals
All the procedures involving animals and their care were conducted in accordance with international guidelines, laws and policies and with the National Institutes of Health Principles of Laboratory Animal Care (NIH publication no. 85-23, revised 1985). The protocol was authorised by our local institutions.
In all experiments, adult male Sprague–Dawley rats weighting 250–300 g (Charles River, Wilmington, MA, USA), were used. Experimental diabetes was induced by a single injection of streptozotocin according to a standardised protocol [8]. Briefly, after 12 h of fasting, animals were sedated with inhaled sodium isofluorane followed by intraperitoneal injection of 50 mg/kg streptozotocin in sodium citrate buffer, 50 mmol/l, pH 4.5. Blood glucose concentration was determined on days 2, 7 and 14 by the use of a commercially available human glucose meter (Glucocard; ArkRay, Kyoto, Japan). Diabetes was confirmed when blood glucose was equal to or higher than 16.7 mmol/l (300 mg/dl) on at least two consecutive occasions within the first week. Rats whose blood glucose remained lower than 16.7 mmol/l after 1 week were withdrawn from the study. Control rats were injected intraperitoneally with a corresponding volume of buffer (saline). In order to stabilise hyperglycaemia and diabetes, all experiments were performed 4 weeks after confirmation of hyperglycaemia.
Hindlimb I/R injury
Control and diabetic rats (4 weeks of documented hyperglycaemia) were subjected to a 2-h hindlimb I/R injury as follows. Animals were anaesthetised by intramuscular injection of 700 μg/kg tilethamine hydrochloride–zolazepam hydrochloride mixture (Virbac, Peakhurst, NSW, Australia) plus 150 μg/kg xylazine (Bio 98, Bologna, Italy) subcutaneously. Distal limb perfusion was monitored with a laser Doppler flowmeter (Periflow; Perimed, Milan, Italy). A 9-mm large digit cuff (Perimed) was placed around the thigh and connected to a standard manometer. The cuff was inflated with air until the laser Doppler flowmeter recorded zero biological flow and the pressure on the manometer was above 200 mmHg. Perfusion and pressure in the cuff were monitored during the experiment to assure continuous and stable ischaemia; additional cuff inflations were performed when pressure fell occasionally below 200 mmHg or when perfusion tended to rise. After 2 h the cuff was deflated. At various time points after ischaemia, animals (four at each time point) were anaesthetised and blood samples were drawn by external cardiac aspiration until complete exsanguination. Bone marrow was obtained by flushing femurs and tibias. Euthanasia was then completed by giving an overdose of Tania (Internet International, Boxmeer, The Netherlands).
Insulin treatment during hindlimb I/R
In a separate set of diabetic animals (n=12), insulin was administered in order to achieve euglycaemia during the ischaemia and reperfusion periods. Briefly, 30 min before starting hindlimb ischaemia, 10 U/kg recombinant insulin analogue (Novorapid; Novo Nordisk, Bagsværd, Denmark) was administered subcutaneously. Blood glucose was monitored every 30 min and additional doses of insulin were administered when glucose rose above 11.1 mmol/l (200 mg/dl). In order to achieve prolonged euglycaemia, 50 U/kg of the long-acting insulin analogue glargine (Lantus; Sanofi-Aventis, Bridgewater, NJ, USA) was administered subcutaneously at the time of reperfusion and then daily until euthanasia, which took place 1, 3 or 7 days later, as described above.
Progenitor cell mobilisation with granulocyte-colony stimulating factor and stem cell factor
Control and diabetic rats were treated with granulocyte-colony stimulating factor (G-CSF; Amgen, Thousand Oaks, CA, USA) plus stem cell factor (SCF; Amgen) to study cytokine-mediated progenitor cell mobilisation, as described previously [9]. Briefly, on days 1–5 before I/R injury, rats were injected subcutaneously with 50 μg/kg G-CSF plus 200 μg/kg SCF daily. On day 5, rats were anaesthetised and blood samples were drawn from the tail vein, and then the rats underwent I/R injury as described above. In these experiments, diabetic animals were not treated with insulin. Animals were then killed on day 8 in order to achieve a 3-day reperfusion time.
Flow cytometry
All samples were processed after 1–2 h. Progenitor cells were defined by the surface expression of stem cell antigen-1 (Sca-1) and c-kit (CD117) antigens [10, 11]. Peripheral blood or bone marrow cells were analysed for the expression of cell surface antigens with direct two-colour flow cytometry (FACSCalibur; BD Biosciences, Franklin Lakes, NJ, USA) using conjugated monoclonal antibodies. Briefly, 150 μl of peripheral blood was incubated with 10 μl of phycoerythrin-conjugated anti-mouse Sca-1 monoclonal antibody (Cederlane, Hornby, ON, Canada) and 10 μl of fluoroisothiocyanate-conjugated anti-mouse c-kit monoclonal antibody (BD Biosciences), followed by incubation at 4°C for 30 min. The frequency of peripheral blood cells positive for the above reagents was determined by a two-dimensional side scatter-fluorescence dot plot analysis of the samples stained with the different reagents, after appropriate gating to exclude granulocytes. Initially we gated Sca-1+ peripheral blood cells and then examined the resulting population for dual expression of c-kit (Fig. 1a,b). For further analysis, Sca-1+ cells were studied for the expression of CD31 using a phycoerythrin-conjugated anti-rat CD31 monoclonal antibody (BD Biosciences), reflecting endothelial differentiation of progenitor cells (Fig. 1c,d). Data were processed using the Macintosh CELLQuest software program (BD Biosciences). A single trained operator (I.B.), who was blind to the status of the animal, performed all flow cytometric analyses throughout the study.
Quantification and characterisation of progenitor cells in peripheral blood. Representative cytograms showing double staining with anti-Sca-1 and anti-c-kit antibodies for the determination of Sca-1+c-kit+ cells at time zero (a) and at day 3 after reperfusion (b). c, d CD31 expression on Sca-1+ cells. e–g A group of sorted Sca-1+ cells identified by the surface expression of vWF (red) and Flk-1 (green)
Cell characterisation
To further characterise progenitor cells, Sca-1+ cells were studied for the expression of von Willebrand factor (vWF) and fetal liver kinase-1 (Flk-1) using direct immunofluorescence (Fig. 1e). Peripheral blood mononuclear cells were separated using Histopaque (Sigma Aldrich, St Louis, MO, USA) and fluorescence-activated cell sorting of Sca-1+ cells was performed. Isolated Sca-1+ cells were fixed and incubated with anti-vWF (Dako Cytomation, Glostrup, Denmark) and anti-Flk-1 (Santa Cruz Biotechnology, Santa Cruz, CA, USA) antibodies and secondary Cy2 anti-rabbit (Chemicon International, Temecula, CA, USA) and TRITC-anti-mouse (Dako Cytomation) antibodies. The Sca-1+vWF+Flk-1+ cells were then visualised under a fluorescence microscope.
Histological examination
Five-micrometre cryosections of tibialis anterior and extensor digitorus longus (EDL), as representative of predominantly fast glycolytic muscles, were stained with a haematoxylin and eosin kit (Bio-Optica, Milan, Italy) according to the manufacturer’s protocol.
Capillary density
Capillary density was studied in the EDL because its small cross-section allowed easy determinations of the entire capillary bed. Five-micrometre muscle sections were incubated with purified anti-vWF antibody (Dako Cytomation) and with a secondary goat anti-rabbit Cy2 IgG (Chemicon International) antibody, and then observed under a fluorescence microscope. Nuclei were stained with Hoechst 33258 (Sigma Aldrich). Capillaries were counted by two independent operators in the entire section surface and in five sections at different levels along the length of the muscle. Capillaries were defined as vascular structures surrounded by a monolayer of vWF+ nucleated cells and were distinguished from venules and arterioles on the basis of diameter and because the arteriolar wall included concentric layers of smooth muscles cells. Section area was determined under a light microscope and capillary density was calculated as capillary count divided by section area.
Vascular endothelial growth factor and stromal-derived growth factor assays
Plasma levels of vascular endothelial growth factor (VEGF) and stromal-derived growth factor (SDF-1) were determined with an ELISA using commercially available kits (anti-mouse VEGF ELISA kit, Biosource International; CXCL12/SDF-1α Quantikine ELISA kit, R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s protocol.
Expression of hypoxia-inducible factor 1α
Because of its larger volume in comparison with EDL, the tibialis anterior muscle was used to determine the expression of hypoxia-inducible factor 1α; (HIF-1α). Briefly, tibialis anterior tissue extracts were prepared by homogenisation followed by lysis with the extraction buffer (100 mmol/l NaCl, 50 mmol/l KCl, 0.1 mmol/l EDTA, 20 mmol/l Tris–HCl pH 7.5, 10% glycerol, 0.2% Nonidet NP-40, 0.1% Triton X-100) and treatment with a cocktail of protease inhibitors (Sigma Aldrich). To obtain nuclear proteins, the pellet was treated with extraction buffer plus SDS 10% and centrifuged. Nuclear proteins were then diluted with 750 μl Laemmli’s sample buffer plus 250 μl β-mercaptoethanol (Serva, Heidelberg, Germany), heated, spun down and further diluted with sample buffer. HIF-1α expression was investigated by Western blotting. The area and intensity of the HIF-1α band were normalised to nuclear lamin A/C expression, as described previously [12], using anti-HIF-1α and anti-lamin A/C antibodies (Santa Cruz). Secondary antibodies were rabbit anti-goat IgG conjugated with horseradish peroxidase (HRPO) and pig anti-rabbit check IgG–HRPO (Chemicon International).
Statistical analyses
Data are expressed as mean±SEM. Cell counts are expressed as the number of cells per 106 cytometric events. Student’s t test was applied to compare data from two independent groups. Pearson’s r coefficient was used to assess linear correlations between continuous variables. Statistical significance was accepted at p≤0.05.
Results
Characterisation of progenitor cells
Peripheral blood and bone marrow progenitor cells were characterised by the expression of Sca-1 and c-kit antigens (Fig. 1a,b). To exclude the possibility that variations in Sca-1+ and Sca-1+c-kit+ cells were due to an inflammatory response to I/R injury, granulocytes were gated out of the analysis and the progenitor cell count was always normalised to the total leucocyte count (106 cytometric events). Ranges for Sca-1+ and Sca-1+c-kit+ cells were 0.05–0.9% and 0.004–0.05% of circulating leucocytes, respectively. To further characterise progenitor cells, we determined the co-expression of other markers, showing that 86.3±3.5% of Sca-1+ cells also expressed CD31 (Fig. 1c,d). Moreover, Sca-1+ cells separated by fluorescence-activated cell sorting also included a rare population of vWF+Flk+ cells, as shown by immunofluorescence, which may be considered the true endothelial progenitors (Fig. 1e).
Characterisation of the I/R injury
The hindlimb I/R injury was performed to set up an acute and transient ischaemic insult and to study the mobilisation of progenitor cells from bone marrow to peripheral blood. Ischaemia was ascertained during the procedure by monitoring the pressure around the thigh and the flow distal to the cuff, and the corresponding injury was confirmed at the time the animal was killed in muscle sections stained with haematoxylin and eosin. Myofibres in the lesion area showed extensive disarrangement and ballooning as well as marked signs of myocellular death. These alterations were more evident 1 day after the ischaemic insult, were more pronounced in the EDL, did not differ macro- and microscopically between control and diabetic animals, and did not differ between animals treated or not with insulin or haematopoietic growth factors (Fig. 2).
Kinetics of progenitor cell mobilisation after ischaemia
First, we characterised the normal kinetics of progenitor cells in control animals, by measuring circulating Sca-1+ and Sca-1+c-kit+ cells before ischaemia and every 24 h of reperfusion time, until the cell count returned to baseline. Sca-1+ cells peaked 2 days after ischaemia, showing a four-fold increase compared with baseline, while Sca-1+c-kit+ cells reached a peak 2.7-fold increase 3 days after ischaemia. Both cell counts returned to baseline 7 days after ischaemia (Fig. 3a). The increase in the number of progenitor cells compared with baseline was statistically significant from days 1 to 6. On the basis of this kinetic, a four time-point analysis was performed in diabetic animals, which included evaluation of progenitor cells at baseline and days 1, 3 and 7 after ischaemia (Fig. 3b,c). Diabetic rats did not show an increase in progenitor cell count after I/R injury; it is noteworthy that a paradoxical 1.61-fold decrease from days 1 to 3 was observed for Sca-1+c-kit+ cells. At each specified time point, including baseline, the numbers of Sca-1+ and Sca-1+c-kit+ cells were significantly lower in diabetic than in control animals.
Peripheral blood and bone marrow progenitor cells after IR injury. a Temporal kinetics of Sca-1+ (filled triangles), c-kit+ (filled squares) and Sca-1+c-kit+ (empty triangles) progenitor cells in control rats. b, c Progenitor cell kinetics in diabetic (filled squares) and control animals (filled triangles). Numbers of cells in insulin-treated animals are also shown (empty triangles). *p<0.05, diabetic vs non-diabetic rats; **p<0.05, untreated vs insulin-treated diabetic rats. d Frequencies of bone marrow Sca-1+ (white columns), c-kit+ (grey columns) and Sca-1+c-kit+ (black columns) progenitor cells in basal conditions and 3 days after ischaemia in control and diabetic rats. Data for insulin-treated rats at day 3 (d3+INS) are also shown
Quantification of progenitor cells in bone marrow
To explore the relationship between peripheral blood and bone marrow progenitor cells, we also determined the levels of Sca-1+ and Sca-1+c-kit+ cells in bone marrow of control and diabetic rats at baseline and at the moment of maximal marrow stimulation according to the kinetic described above. In both control and diabetic animals there was a small, non-significant increase in marrow Sca-1+ cells from baseline to day 3, while the Sca-1+c-kit+ cell count did not vary. Remarkably, at both baseline and day 3, the numbers of bone marrow progenitors were not statistically different in diabetic and control animals (Fig. 3d).
Capillary density
To explore whether altered mobilisation of progenitor cells in diabetes was associated with defective angiogenesis in the ischaemic muscles, we evaluated capillary density in the injured and contralateral muscles 7 days after ischaemia (Fig. 4). In control rats, there was a mean 50% increase in EDL capillary density compared with contralateral non-ischaemic muscles. No increase in capillary density was seen in ischaemic muscles from diabetic rats.
a Representative immunofluorescence with anti-vWF antibodies (green) for capillary density determination in control and diabetic rats. Arrows indicate examples of arterioles, which were not included in the vessel count. b In control rats, at day 7 (black columns) vs basal (white columns), capillary density was increased by about 50%, whereas it was not significantly modified in diabetic rats. *p<0.05
Plasma levels of VEGF and SDF-1α after I/R injury
To investigate putative mechanisms of reduced progenitor cell mobilisation in the setting of diabetes, we measured plasma levels of VEGF and SDF-1α at the same time points as those used in the analysis of progenitor cell kinetics (Fig. 5a,b). In control animals, both VEGF and SDF-1α increased after ischaemia and peaked at day 3 (2.9- and 2-fold, respectively). In diabetic animals, VEGF showed an analogous peak at day 1 after I/R and decreased rapidly to baseline levels on day 3, whereas no significant variation in SDF-1α occurred throughout the reperfusion period. Interestingly, at day 3, which corresponded to the peak of VEGF and SDF-1α and the mean peak time of progenitor cells in control animals, levels of both VEGF and SDF-1α were significantly lower in diabetic than in control rats. Plasma levels of SDF-1α were also closely correlated to the numbers of Sca-1+ and Sca-1+c-kit+ cells in both control and diabetic animals (Fig. 5c), while correlations of VEGF with progenitor cells were not statistically significant (not shown).
Plasma concentrations of VEGF (a) and SDF-1α (b) in basal conditions and at days 1, 3 and 7 after ischaemia in control (continuous line and empty triangles) and diabetic (dashed line and filled squares) rats. c Linear regression analyses showing correlations between plasma SDF-1 and Sca-1+c-kit+ cells in control (filled triangles, r=0.85) and diabetic animals (empty squares, r=0.72). d Protein levels of HIF-1α normalised to lamin A/C and expressed as fold-variation vs basal and representative Western blots at the same time points in diabetic (black columns) and control (white columns) rats. *p<0.05
HIF-1α expression in the target tissue
We then hypothesised that altered expression and release of VEGF and SDF-1 were due to inability to upregulate hypoxia-sensitive systems. HIF-1α expression increased dramatically in control rats after ischaemia, with a 5.5-fold peak on day 3, and returned to near the basal level after 7 days, whereas it was paradoxically downregulated in diabetic animals (Fig. 5d).
Effects of blood glucose lowering during I/R
As the main metabolic alteration in streptozotocin-induced diabetes in rats is severe hyperglycaemia, we tested the hypothesis that diabetes-induced defective progenitor cell mobilisation can be reversed by lowering blood glucose. In the insulin-treated group, blood glucose was kept below 11.1 mmol/l (6.9±1.2 mmol/l) during ischaemia and we actively sought to achieve sustained euglycaemia during the whole reperfusion time despite wide variability in daily insulin needs (blood glucose during reperfusion 9.4±1.7 mmol/l). Lowering the blood glucose concentration during I/R was followed by partial recovery of mobilisation capacity, since circulating Sca-1+ cells had increased 4.7-fold at day 3 compared with baseline, and Sca-1+c-kit+ cells had increased 1.8-fold (Fig. 3b,c). This improvement in progenitor cell mobilisation was mirrored by increases, albeit non-significant, in the numbers of bone marrow Sca-1+ (1.8-fold) and Sca-1+c-kit+ cells (1.7-fold) (Fig. 3d). Moreover, glucose lowering led to a significant 2.6-fold increase in VEGF levels at day 3 compared with non-treated animals (56.3±12.0 vs 21.6±10.2 pg/ml, p=0.03), while SDF-1 levels were not affected (not shown).
Mobilisation of progenitor cells after growth factor administration
To establish whether growth factor-mediated progenitor cell mobilisation was also defective in the presence of diabetes, we employed a protocol for bone marrow stimulation described previously [9]. To verify whether this treatment allowed recovery of mobilisation capacity in diabetic animals, an I/R injury was set up after marrow stimulation (Fig. 6). In control rats, Sca-1+ increased 3.7-fold compared with baseline at the end of marrow stimulation and peaked 7.9-fold at day 3 of reperfusion after ischaemia; Sca-1+c-kit+ cells did not increase after marrow stimulation, but reached a 2.34-fold peak after I/R injury. In diabetic rats, a similar trend was seen, although at lower levels: Sca-1+ cells increased 2.2-fold after marrow stimulation and peaked 4.7-fold after ischaemia; Sca-1+c-kit+ cells did not increase after marrow stimulation, but had a 1.6-fold peak at day 3 after ischaemia. Taken together, these results suggest that preventive marrow stimulation leads to a partial recovery of ischaemia-induced progenitor cell mobilisation in diabetic animals, but also suggest that marrow responsiveness is subnormal in diabetes.
Discussion
Diabetic patients are at increased risk of cardiovascular disease and their prognosis after acute events is poorer than that of non-diabetic subjects [13]. The present study demonstrates that ischaemia- and growth factor-mediated mobilisation of progenitor cells is defective in diabetic rats.
We have demonstrated previously in humans that worsening degrees of diabetic vascular complications are paralleled by progressive EPC exhaustion [7]. This is in accordance with the hypothesis that diabetes lowers the number of circulating EPCs and that the resulting poor regenerative capacity favours the clinical development of vascular disease, by altering endothelial homeostasis and inhibiting compensatory angiogenesis [14]. Available data make this picture likely, but the mechanisms are largely unknown [15]. EPC reduction in diabetes may have two causes: shortened peripheral survival due to hyperglycaemic stress, and altered bone marrow mobilisation. While the former hypothesis has been substantiated [16, 17], the latter has not been tested before. In the present work, we have used a model of transient ischaemia to study the mobilisation of Sca-1+ and Sca-1+c-kit+ progenitors in control and diabetic rats. The selected cell populations represent highly immature cells that account for a small fraction of circulating mononuclear cells and include endothelial-committed precursors involved in compensatory angiogenesis at ischaemic sites [10, 11]. Moreover, circulating Sca-1+ cells exhibited very high expression of the endothelial marker CD31 and included a small population of vWf+Flk-1+ cells. At baseline, Sca-1+ and Sca-1+c-kit+ cell counts were lower in diabetic than in control animals. Moreover, after injury, Sca-1+ and Sca-1+c-kit+ cells increased transiently with a time course of 7 days in control rats, whereas they were almost unchanged in their diabetic counterparts. Bone marrow progenitors were not significantly reduced in diabetic animals, suggesting that the mobilisation process rather than the central compartment was affected by the diabetic state. Consistently, hampered mobilisation of progenitor cells in diabetic rats was followed by inability to increase the capillary density of the target tissue in comparison with controls.
It is likely that the weakened mobilisation process was due to deficient bone marrow stimulation after ischaemia, as shown by the altered release of VEGF and SDF-1α, both of which are implicated in EPC mobilisation [18]. In control animals, the time course of the plasma concentrations of both VEGF and SDF-1α peaked at day 3 after ischaemia. In diabetic animals, whereas SDF-1α remained at baseline, VEGF had an early peak at day 1. Therefore, inability to upregulate SDF-1α seemed to account for the defective progenitor cell mobilisation in diabetes. According to the recently described comprehensive effects of SDF-1α on progenitor cells [19], in our study plasma levels of SDF-1α were strictly correlated to Sca-1+ and Sca-1+-c-kit+ levels, suggesting a relevant role of SDF-1α in progenitor cell mobilisation. Since it has been proposed that VEGF and SDF-1α act together in stimulating angiogenic processes [20], the time-discordant activation of these factors in diabetes may have an important impact on the efficiency of neovascularisation. In fact, both VEGF and SDF-1α are regulated by hypoxia and are responsive to the oxygen-sensing system involving HIF-1α. The HIF-1α–SDF-1α axis has been shown to mediate adhesion, migration and homing of circulating progenitor cells to ischaemic tissues [21]. It is noteworthy that in control animals we have shown that peak plasma levels of VEGF and SDF-1α were synchronous with the highest expression of HIF-1α, which is potently upregulated after muscle ischaemia. Conversely, in diabetic animals the altered release of angiogenic factors into the circulation was associated with downregulation of HIF-1α after I/R injury. Alterations of hypoxia-sensitive genes have been reported previously in diabetes: for example, blunted HIF-1α induction after myocardial ischaemia has been associated with increased infarct size [22]. I/R injury sets up a typical pro-oxidative condition that may be worsened by the diabetic state, which is characterised by increased oxidative stress and reduced anti-oxidative defences [23–25]. Enhanced production of reactive oxygen species simulates a hyperoxic state and may lead to HIF-1α ubiquitination and degradation after ischaemia in diabetes [26]. Moreover, hyperglycaemia itself has been shown to inhibit hypoxia-induced stabilisation of HIF-1α protein against degradation [27]. Therefore, we suggest that the weak angiogenic response to ischaemia in diabetes depends upon inability to mobilise the progenitor cells necessary for new vessel growth. Speculatively, the mechanistic explanation can be traced back to the well-known unifying hypothesis [23], because oxidative stress may represent the prime mover of this alteration. It is noteworthy that stimulation of angiogenesis through an increase in the number of EPCs has been demonstrated recently in diabetic mice after administration of benfotiamine, which is believed to block the biochemical pathways responsible for the enhanced production of reactive oxygen species in diabetes [28]. Future research could be directed to verifying whether inhibition of oxidative stress is able to prevent the downregulation of HIF-1α after ischaemia, allowing adequate bone marrow stimulation, release of angiogenic cells and collateralisation to overwhelm vascular obstruction.
This study also explored possible treatment strategies to restore progenitor cell release after ischaemia. We show that the ability of progenitor cells to be mobilised is partly recovered if insulin is administered to diabetic rats during the I/R period to correct hyperglycaemia. Treated rats also showed a significant increase in VEGF levels at day 3, which may have compensated, in part, for the SDF-1α deficiency and supported progenitor cell mobilisation. Lowering blood glucose remains the standard therapy to prevent late diabetic complications [29]. Intensified glucose control also increases survival after acute coronary syndromes [30], and the ability to upregulate progenitor cells after myocardial infarction is directly correlated to the residual left ventricular function [6]. Even if the results of the present study need to be confirmed in humans, we may hypothesise that glucose control increases progenitor cell levels and ameliorates compensatory angiogenesis, thus minimising residual ischaemia. Whether the increase in progenitor cell levels was due to decreased blood glucose levels rather than insulin itself is not clear. Consistent with the existing literature, we would like to speculate that lower glucose levels prolong progenitor cell survival [16] and insulin supplementation mobilises marrow cells, possibly through nitric oxide stimulation [31].
Haematopoietic growth factors have been shown to mobilise EPCs and increase neovascularisation of ischaemic tissues [32, 33], but it was not known whether these effects are preserved in diabetes. Our results indicate that pretreatment with G-CSF and SCF leads to a partial recovery of mobilisation of Sca-1+ and Sca-1+c-kit+ cells in diabetic animals, although its efficiency is still blunted with respect to controls. On the whole, our data suggest that defective progenitor cell release in diabetes may be due to both weak bone marrow stimulation by the ischaemic tissue and reduced bone marrow responsiveness to mobilising factors.
In conclusion, this study demonstrates that diabetes is associated with defective ischaemia-induced mobilisation of progenitor cells from bone marrow to peripheral blood, with a subsequent deficiency in compensatory angiogenesis in the ischaemic tissue. This dysfunction may be due to inability to upregulate hypoxia-sensing systems after an ischaemic insult, and to depressed bone marrow responsiveness. Both blood glucose lowering and pretreatment with haematopoietic growth factors can acutely restore the mobilisation of progenitor cells to some extent, suggesting that these therapeutic strategies may predispose to favourable outcomes in diabetic ischaemic syndromes.
Abbreviations
- c-kit:
-
cellular-kinase in tyrosine
- EDL:
-
extensor digitorus longus
- EPC:
-
endothelial progenitor cell
- Flk-1:
-
fetal liver kinase-1
- G-CSF:
-
granulocyte-colony stimulating factor
- HIF-1α:
-
hypoxia-inducible factor 1α
- I/R:
-
ischaemia–reperfusion
- Sca-1:
-
stem cell antigen-1
- SCF:
-
stem cell factor (c-kit ligand)
- SDF-1:
-
stromal-derived growth factor
- VEGF:
-
vascular endothelial growth factor
- vWF:
-
von Willebrand factor
References
Waltenberger J (2001) Impaired collateral vessel development in diabetes: potential cellular mechanisms and therapeutic implications. Cardiovasc Res 49:554–560
Asahara T, Masuda H, Takahashi T et al (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 85:221–228
Urbich C, Dimmeler S (2004) Endothelial progenitor cells: characterization and role in vascular biology. Circ Res 95:343–353
Schmidt-Lucke C, Rossig L, Fichtlscherer S et al (2005) Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation 111:2981–2987
Werner N, Kosiol S, Schiegl T et al (2005) Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med 353:999–1007
Leone AM, Rutella S, Bonanno G et al (2005) Mobilization of bone marrow-derived stem cells after myocardial infarction and left ventricular function. Eur Heart J 26:1196–1204
Fadini GP, Miorin M, Facco M et al (2005) Circulating endothelial progenitor cells are reduced in peripheral vascular complications of type 2 diabetes mellitus. J Am Coll Cardiol 45:1449–1457
Yoon YS, Uchida S, Masuo O et al (2005) Progressive attenuation of myocardial vascular endothelial growth factor expression is a seminal event in diabetic cardiomyopathy: restoration of microvascular homeostasis and recovery of cardiac function in diabetic cardiomyopathy after replenishment of local vascular endothelial growth factor. Circulation 111:2073–2085
Orlic D, Kaystura J, Chimenti S et al (2001) Mobilized bone marrow cells repair the infarcted heart, improving function and survival. Proc Natl Acad Sci U S A 98:10344–10349
Bailey AS, Jiang S, Afentoulis M et al (2004) Transplanted adult hematopoietic stems cells differentiate into functional endothelial cells. Blood 103:13–19
Jackson AK, Majka SM, Wang H et al (2001) Regeneration of ischemic cardiac muscle and vascular endothelium by adult stem cells. J Clin Invest 107:1395–1402
Pisani D, Dechesne C (2005) Skeletal muscle HIF-1alpha expression is dependent on muscle fiber type. J Gen Physiol 126:173–178
Aronson D, Rayfield EJ, Chesebro JH (1997) Mechanisms determining course and outcome of diabetic patients who have had acute myocardial infarction. Ann Intern Med 126:296–306
Fadini GP, Agostini C, Avogaro A (2005) Endothelial progenitor cells and vascular biology in diabetes mellitus: current knowledge and future perspectives. Current Diabetes Rev 1:41–58
Tamarat R, Silvestre JS, Le Ricousse-Roussanne S et al (2004) Impairment in ischemia-induced neovascularization in diabetes: bone marrow mononuclear cell dysfunction and therapeutic potential of placenta growth factor treatment. Am J Pathol 164:457–466
Krankel N, Adams V, Linke A et al (2005) Hyperglycemia reduces survival and impairs function of circulating blood-derived progenitor cells. Arterioscler Thromb Vasc Biol 25:698–703
Seeger FH, Haendeler J, Walter DH et al (2005) p38 mitogen-activated protein kinase downregulates endothelial progenitor cells. Circulation 111:1184–1191
Aicher A, Zeiher AM, Dimmeler S (2005) Mobilizing endothelial progenitor cells. Hypertension 45:321–325
Ceradini DJ, Gurtner GC (2005) Homing to hypoxia: HIF-1 as a mediator of progenitor cell recruitment to injured tissue. Trends Cardiovasc Med 15:57–63
Kryczec I, Lange A, Mottram P et al (2005) CXCL12 and vascular endothelial growth factor synergistically induce neoangiogenesis in human ovarian cancers. Cancer Res 65:465–472
Ceradini DJ, Kulkarni AR, Callaghan MJ et al (2004) Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med 10:858–864
Marfella R, D’Amico M, Di Filippo C et al (2002) Myocardial infarction in diabetic rats: role of hyperglycaemia on infarct size and early expression of hypoxia-inducible factor 1. Diabetologia 45:1172–1181
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625
Moreno PR, Fuster V (2004) New aspects in the pathogenesis of diabetic atherothrombosis. J Am Coll Cardiol 44:2293–2300
Pagnin E, Fadini G, de Toni R, Tiengo A, Calo L, Avogaro A (2005) Diabetes induces p66shc gene expression in human peripheral blood mononuclear cells: relationship to oxidative stress. J Clin Endocrinol Metab 90:1130–1136
Eyries M, Collins T, Khachigian LM (2004) Modulation of growth factor gene expression in vascular cells by oxidative stress. Endothelium 11:133–139
Catrina SG, Okamoto K, Pereira T, Brismar K, Poellinger L (2004) Hyperglycemia regulates hypoxia-inducible factor-1a protein stability and function. Diabetes 53:3226–3232
Gadau S, Emanueli C, Van Linthout S et al (2006) Benfotiamine accelerates the healing of ischaemic diabetic limbs in mice through protein kinase B/Akt-mediated potentiation of angiogenesis and inhibition of apoptosis. Diabetologia 49:405–420
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive therapy of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
Malmberg K, Dryden L, Efendic S et al (1995) Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI Study): effects on mortality at 1 year. J Am Coll Cardiol 26:57–65
Landmesser U, Engberding N, Bahlmann FH et al (2004) Statin-induced improvement of endothelial progenitor cell mobilization, myocardial neovascularization, left ventricular function, and survival after experimental myocardial infarction requires endothelial nitric oxide synthase. Circulation 110:1933–1939
Kong D, Melo LG, Gnecchi M et al (2004) Cytokine-induced mobilization of circulating endothelial progenitor cells enhances repair of injured arteries. Circulation 110:2039–2046
Woo YJ, Grand TJ, Berry MF et al (2005) Stromal cell-derived factor and granulocyte–monocyte colony-stimulating factor form a combined neovasculogenic therapy for ischemic cardiomyopathy. J Thorac Cardiovasc Surg 130:321–329
Acknowledgements
This work was partially supported by a grant to S. Sartore from Consortium Agreement European Community Heart Failure and Cardiac Repair-IP 018630.
Duality of interest
The authors have no conflict of interest to disclose in relation to the findings contained in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fadini, G.P., Sartore, S., Schiavon, M. et al. Diabetes impairs progenitor cell mobilisation after hindlimb ischaemia–reperfusion injury in rats. Diabetologia 49, 3075–3084 (2006). https://doi.org/10.1007/s00125-006-0401-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0401-6