Abstract
Aims/hypothesis
Variation within six novel genetic loci has been reported to confer risk of type 2 diabetes and may be associated with beta cell dysfunction. We investigated whether these polymorphisms are also associated with impaired proinsulin to insulin conversion.
Methods
We genotyped 1,065 German participants for single nucleotide polymorphisms rs7903146 in TCF7L2, rs7754840 in CDKAL1, rs7923837 and rs1111875 in HHEX, rs13266634 in SLC30A8, rs10811661 in CDKN2A/B and rs4402960 in IGF2BP2. All participants underwent an OGTT. Insulin, proinsulin and C-peptide concentrations were measured at 0, 30, 60, 90 and 120 min during the OGTT. Insulin secretion was estimated from C-peptide or insulin levels during the OGTT using validated indices. We used the ratio proinsulin/insulin during the OGTT as indicator of proinsulin conversion.
Results
In our cohort, we confirmed the significant association of variants in TCF7L2, CDKAL1 and HHEX with reduced insulin secretion during the OGTT (p < 0.05 for all). Variation in SLC30A8, CDKN2A/B and IGF2BP2 was not associated with insulin secretion. The risk alleles of the variants in TCF7L2, CDKAL1 and SLC30A8 reduced proinsulin to insulin conversion (p < 0.05 for all), whereas the risk alleles in HHEX, CDKN2A/B and IGF2BP2 were not associated with reduced proinsulin to insulin conversion (p > 0.6).
Conclusions/interpretation
Diabetes-associated variants in TCF7L2 and CDKAL1 impair insulin secretion and conversion of proinsulin to insulin. However, both aspects of beta cell function are not necessarily linked, as impaired insulin secretion is specifically present in variants of HHEX and impaired proinsulin conversion is specifically present in a variant of SLC30A8.
Similar content being viewed by others
Introduction
Recent genome-wide association scans have found various new diabetes susceptibility genes including TCF7L2, CDKAL1, HHEX, SLC30A8, CDKN2A/B and IGF2BP2 [1–3]. Impaired insulin secretion and impaired insulin sensitivity are the major pathogenic mechanisms leading to type 2 diabetes. Several of these novel risk loci for type 2 diabetes have been found to be associated mainly with impaired beta cell function [4–8]. Furthermore, a recently published study found associations between single nucleotide polymorphisms (SNPs) in TCF7L2 and increased fasting proinsulin concentration, suggesting that, in addition to insulin secretion, variation in TCF7L2 might be involved in insulin synthesis and processing [9].
The conversion of proinsulin to insulin is one aspect of beta cell function. The relative proportion of proinsulin to insulin (PI/I) in the secretory granule represents an estimate of the efficiency of proinsulin processing [10]. A decrease in the PI/I ratio indicates an increase in the rate of proinsulin processing and vice versa. An elevated PI/I ratio has been observed in conditions with impaired beta cell function, such as type 2 diabetes [11] and impaired glucose tolerance [12].
The present study examined the association of SNPs in TCF7L2 (rs7903146), CDKAL1 (rs7754840), HHEX (rs7923837, rs1111875), SLC30A8 (rs13266634), CDKN2A/B (rs10811661) and IGF2BP2 (rs4402960) with proinsulin processing. We hypothesised that an impaired proinsulin to insulin conversion might be part of the mechanisms leading to impaired insulin secretion in carriers of these polymorphisms.
Methods
Participants
The participants were selected from the ongoing Tübingen Family Study, which currently includes ~2,000 individuals at increased risk of diabetes [4, 8]. Less than 1% of participants are related to each other. Individuals on medication affecting glucose metabolism were excluded. Inclusion of the participants in the present study was based on availability of: (1) DNA samples for genotyping (n = 1,650); and (2) complete OGTT data (glucose, insulin, C-peptide and proinsulin levels available for all time points during the OGTT, n = 1,065). Data on C-peptide levels during IVGTT and OGTT from 545 participants (51%) included in the present study have been published previously [8].
The anthropometric characteristics of the study population are shown in Table 1. A positive family history for diabetes was reported by 750 participants (70%). All participants were genotyped for the following SNPs: TCF7L2, rs7903146; CDKAL, rs7754840; HHEX, rs7923837 and rs1111875; SLC30A8, rs13266634; CDKN2A/B, rs10811661; and IGF2BP2, rs4402960. Informed written consent was obtained from all participants and the local Ethics Committee approved the protocol.
Genotyping
Genotyping was done using the TaqMan assay (Applied Biosystems, Forster City, CA, USA). The TaqMan genotyping reaction was amplified on a GeneAmp PCR system 7000 and fluorescence was detected on an ABI PRISM 7000 sequence detector (Applied Biosystems). The overall genotyping success rate was 99.98%. Re-screening of 3.16% of participants generated 100% identical results. All SNPs were distributed according to Hardy–Weinberg equilibrium.
Oral glucose tolerance test
After an overnight fast of 12 h, participants ingested a solution containing 75 g glucose at 08:00 hours. Venous blood samples were obtained at 0, 30, 60, 90 and 120 min and plasma glucose, insulin, C-peptide and proinsulin concentrations were determined.
Analytical procedures
Blood glucose was determined using a bedside glucose analyser (glucose-oxidase method; Yellow Springs Instruments, Yellow Springs, CO, USA). Plasma insulin and proinsulin were determined by microparticle enzyme immunoassay (Abbott Laboratories, Tokyo, Japan, and IBL, Hamburg, Germany, respectively). The proinsulin assay has 0% cross-reactivity with human insulin and C-peptide. The insulin assay has 0% cross-reactivity with proinsulin.
Calculations
Insulin secretion in the OGTT was assessed by calculating the AUC for C-peptide divided by the AUC for glucose. For additional validated insulin secretion and sensitivity indices see Electronic supplementary material (ESM) Tables. Proinsulin to insulin conversion was determined by dividing AUC proinsulin by AUC insulin.
Statistical analyses
Data are given as mean ± SEM. Data that were not normally distributed were logarithmically transformed. A p value of <0.05 was considered statistically significant. All risk alleles show an additive inheritance pattern [3]; we therefore used an additive linear model for all analyses. The statistical software package JMP 4.0 (SAS Institute, Cary, NC, USA) was used.
Our study was sufficiently powered (1−β > 0.8, α = 0.05) to detect effect sizes with Cohen’s d ≥0.19 for the SNPs with the lowest minor allele frequencies. Power calculations were performed using G*power software (www.psycho.uni-duesseldorf.de/aap/projects/gpower/).
Results
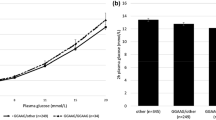
Insulin secretion
The risk alleles of rs7903146 in TCF7L2, rs7754840 in CDKAL1 and rs7923837/rs1111875 in HHEX were associated with lower insulin secretion measured as AUC (C-peptide)/AUC (glucose) during the OGTT (p < 0.05 for all; Table 2). Other validated indices for insulin secretion estimated from OGTT data showed similar results (ESM Tables 1–7). Insulin secretion based on measurement of C-peptide and insulin levels during the OGTT was not associated with polymorphisms in SLC30A8, IGF2BP2 and CDKN2A/B (p > 0.5).
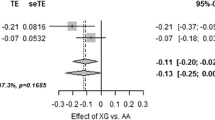
Proinsulin/insulin ratio during the OGTT
The risk alleles of rs7903146 in TCF7L2, rs7754840 in CDKAL1 and rs13266634 in SLC30A were associated with a significantly higher AUC proinsulin/AUC insulin ratio (p < 0.05 for all) (Table 2). The fasting and 30 min proinsulin/insulin ratios were significantly increased in carriers of the risk alleles in TCF7L2, whereas carriers of the risk alleles in CDKAL1 had significantly increased proinsulin/insulin ratios at 30 min only and carriers of risk alleles in SLC30A8 had increased proinsulin/insulin ratios at 60 and 90 min during the OGTT (ESM Tables 1, 2, 3). There were no significant differences in proinsulin/insulin ratios during the OGTT between the genotypes of rs7923837 and rs1111875 in HHEX, rs10811661 in CDKN2A/B and rs4402960 in IGF2BP2. Homozygote carriers of the risk allele in IGF2BP2 merely had increased fasting proinsulin levels and proinsulin/insulin ratio (Table 2, ESM Table 7).
Discussion
In the present study, we found that common variants associated with increased risk of diabetes in TCF7L2, CDKAL1 and SLC30A8 are also associated with impaired conversion of proinsulin to insulin. However, we found no impact on proinsulin conversion for the diabetes-associated SNPs in HHEX, CDKN2A/B and IGF2BP2.
The mechanisms by which the variants in TCF7L2, CDKAL1 and SLC30A8 influence proinsulin processing are a matter of speculation. Recently, Loos et al. [9] demonstrated that the genes of proprotein convertases 1 and 2, which are key proteins in the conversion from proinsulin to insulin, exhibit binding sites for T cell transcription factor. Therefore, an interaction with these proprotein convertases may be a mechanism leading to increased proinsulin levels in carriers of the risk alleles of TCF7L2. Another possibility is that the impaired glucagon-like peptide 1 (GLP-1) action present in carriers of the risk alleles in TCF7L2 leads to impaired proinsulin processing. Two recent studies [4, 5] have demonstrated that the risk alleles in TCF7L2 are associated with impaired incretin effect, as the insulin response to oral glucose was lower than that to intravenous glucose. In addition, GLP-1 infusion led to lower insulin secretion in carriers of the risk alleles in TCF7L2 [4]. As GLP-1 infusion is able to normalise reduced proinsulin conversion [13] and GLP-1 signalling is impaired in carriers of the risk alleles in TCF7L2, it is conceivable that the GLP-1 signalling defect also leads to impaired proinsulin processing.
The mechanism by which the variant in the SLC30A8 gene affects proinsulin processing is also unclear. SLC30A8 encodes the zinc transporter protein member 8 (ZnT-8), which is important for storage and maturation of insulin in the granules of the beta cell [14]. It might well be that a functional defect in ZnT-8 impairs proinsulin processing. While demonstrating impaired proinsulin processing in the risk allele of rs13266634 in SLC30A8, we found no effect of this variant on insulin secretion after an oral glucose load, a finding which is in agreement with our previously published results [8]. However, we did demonstrate an effect on insulin secretion in the IVGTT [8]. This finding suggests a defect in proinsulin processing that only leads to impaired insulin secretion under a strongly increased secretory demand, as is present during the IVGTT.
Variation in HHEX results in a marked impairment of insulin secretion, in response to both oral and intravenous glucose administration [8]. The present results show that this is not due to impaired proinsulin processing, at least during an oral glucose challenge. To our knowledge, no other beta cell defects are known to alter insulin secretion but not proinsulin conversion or vice versa.
In carriers of the risk allele in IGF2BP2 we found increased fasting proinsulin levels but no differences in proinsulin conversion after glucose stimulation. Fasting levels of proinsulin and insulin are largely affected by different clearance rates and do not represent the proinsulin conversion in the beta cell [10, 13]. Therefore, we believe that variation in IGF2BP2 has no major impact on proinsulin conversion.
In conclusion, our data suggest that impaired proinsulin processing is one possible mechanism that leads to impaired insulin secretion and increased risk of diabetes in carriers of the risk alleles in TCF7L2 and CDKAL1. However, these two aspects of beta cell dysfunction, impaired insulin secretion and proinsulin processing, are not necessarily linked. Carriers of a variant in SLC30A8 specifically showed impaired proinsulin conversion during oral glucose challenge, whereas carriers of variants in HHEX specifically exhibited impaired insulin secretion.
Abbreviations
- GLP-1:
-
glucagon-like peptide 1
- PI/I:
-
relative proportion of proinsulin to insulin
- SNP:
-
single nucleotide polymorphism
References
Sladek R, Rocheleau G, Rung J et al (2007) A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445:881–885
Scott LJ, Mohlke KL, Bonnycastle LL et al (2007) A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316:1341–1345
Zeggini E, Weedon MN, Lindgren CM et al (2007) Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 316:1336–1341
Schafer SA, Tschritter O, Machicao F et al (2007) Impaired GLP-1 induced insulin secretion in carriers of TCF7L2 polymorphisms. Diabetologia 50:2443–2450
Lyssenko V, Lupi R, Marchetti P et al (2007) Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 117:2155–2163
Steinthorsdottir V, Thorleifsson G, Reynisdottir I et al (2007) A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat Genet 39:770–775
Pascoe L, Tura A, Patel SK et al (2007) Common variants of the novel type 2 diabetes genes, CDKAL1 and HHEX/DIE, are associated with decreased pancreatic z-cell function. Diabetes 56:3101–3104
Staiger H, Machicao F, Stefan N et al (2007) Polymorphisms within novel risk loci for type 2 Diabetes determine β-cell function. PloS ONE 2:e832
Loos RJF, Franks PW, Francis RW et al (2007) TCF7L2 polymorphisms modulate proinsulin levels and β-cell function in a British Europid population. Diabetes 56:1943–1947
Fritsche A, Madaus A, Stefan N et al (2002) Relationships among age, proinsulin conversion, and beta-cell function in nondiabetic humans. Diabetes 51(Suppl 1):S234–S239
Roder ME, Porte D Jr, Schwartz RS, Kahn SE (1998) Disproportionately elevated proinsulin levels reflect the degree of impaired B cell secretory capacity in patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 83:604–608
Larsson H, Ahrén B (1999) Relative hyperproinsulinemia as a sign of islet dysfunction in women with impaired glucose tolerance. J Clin Endocrinol Metab 84:2068–2074
Stumvoll M, Fritsche A, Stefan N, Hardt E, Häring H (2001) Evidence against a rate limiting role of proinsulin processing for maximal insulin secretion in subjects with impaired glucose tolerance and β-cell dysfunction. J Clin Endocrinol Metab 86:1235–1239
Chimienti F, Devergnas S, Favier A, Seve M (2004) Identification and cloning of a β-cell-specific zinc transporter, ZnT-8, localised into insulin secretory granules. Diabetes 53:2330–2337
Acknowledgements
We thank all study participants for their cooperation. We thank the International HapMap Consortium for the public allocation of genotype data. We gratefully acknowledge the technical assistance of A. Bury, A. Guirguis, H. Lutz, M. Weisser, R. Werner, E. Kollmar and B. Horrer. The study was supported by a grant from the Deutsche Forschungsgemeinschaft (KFO 114).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
Anthropometrics and metabolic characteristics of participants carrying the rs7903146 in TCF7L22 (PDF 36.0 KB)
ESM Table 2
Anthropometrics and metabolic characteristics of participants carrying the rs7754840 in CDKAL1 (PDF 31.8 KB)
ESM Table 3
Anthropometrics and metabolic characteristics of participants carrying the rs13266634 in SLC30A8 (PDF 31.8 KB)
ESM Table 4
Anthropometrics and metabolic characteristics of participants carrying the rs7923837 in HHEX (PDF 31.7 KB)
ESM Table 5
Anthropometrics and metabolic characteristics of participants carrying the rs1111875 in HHEX (PDF 31.8 KB)
ESM Table 6
Anthropometrics and metabolic characteristics of participants carrying the rs10811661 in CDKN2A/B (PDF 31.8 KB)
ESM Table 7
Anthropometrics and metabolic characteristics of participants carrying the rs4402960 in IGF2BP2 (PDF 31.9 KB)
Rights and permissions
About this article
Cite this article
Kirchhoff, K., Machicao, F., Haupt, A. et al. Polymorphisms in the TCF7L2, CDKAL1 and SLC30A8 genes are associated with impaired proinsulin conversion. Diabetologia 51, 597–601 (2008). https://doi.org/10.1007/s00125-008-0926-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-0926-y