Abstract
Aims/hypothesis
The anatomic location of excess body fat has an impact on associated cardiometabolic morbidity, and visceral adipose tissue (VAT) is more pathogenic than subcutaneous adipose tissue (SAT). However, VAT or SAT alone provides little information regarding the relative distribution of body fat. We hypothesised that the propensity to store energy in VAT relative to SAT depots may be a correlate of cardiometabolic risk, and tested this hypothesis using the VAT/SAT ratio as a metric of fat distribution.
Methods
We investigated associations of the VAT/SAT ratio with cardiometabolic traits in 3,223 participants (48% women) from the Framingham Heart Study. Fat depots were quantified by multidetector computed tomography (CT) scanning.
Results
In women and men, higher VAT/SAT ratio was associated (p < 0.05) with most assessed cardiovascular risk factors reflecting blood pressure, dyslipidaemia and insulin resistance. Additional adjustment for BMI did not materially change the findings in women, and generally strengthened associations in men. Further adjustment for VAT attenuated some associations in women, but those with lower HDL-cholesterol, higher triacylglycerol (both p < 0.0001) and higher prevalence of hypertension (p = 0.02), diabetes (p = 0.01) and the metabolic syndrome (p = 0.005) remained significant. Similarly, in men, associations with higher systolic (p = 0.006) and diastolic blood pressure (p = 0.03), higher fasting glucose (p = 0.0005), lower HDL-cholesterol and higher triacylglycerol (both p < 0.0001) and higher prevalence of diabetes (p = 0.006) remained significant.
Conclusions/interpretation
VAT/SAT ratio is a correlate of cardiometabolic risk, above and beyond BMI and VAT. The propensity to store fat viscerally versus subcutaneously may be a unique risk factor independent of absolute fat volumes.
Similar content being viewed by others
Introduction
Obesity is an important risk factor for diabetes, dyslipidaemia, hypertension and cardiovascular disease [1, 2]. BMI and waist circumference are commonly used to assess adiposity, but these anthropometric measures contain little or no information regarding the anatomical location of stored excess fat. This is particularly important because several studies have indicated that visceral adipose tissue (VAT) demonstrates a stronger association with metabolic disturbances and cardiovascular risk than subcutaneous adipose tissue (SAT) [3, 4]. However, these investigations are challenged by a relatively high correlation between VAT and SAT, and it has been suggested that SAT may have protective properties [5, 6]. In addition, the absolute quantification of any given fat depot does not reflect its relative distribution in the human body. For example, high VAT volume may reflect both a high overall fat mass as well as propensity to store fat viscerally.
To disentangle the absolute quantity of fat from the propensity to store it viscerally vs subcutaneously, we assessed the VAT/SAT ratio as a metric of relative body fat composition. We hypothesised that the propensity to store surplus energy in the visceral relative to the subcutaneous fat depot would be an independent correlate of cardiometabolic risk. Thus, we investigated associations of the VAT/SAT ratio with metabolic and cardiovascular disease risk factors in participants in the Framingham Heart Study.
Methods
Study sample
Individuals were participants in the Framingham Offspring and Third Generation cohorts that have been previously described [7, 8]. Beginning in 1971, the Framingham Offspring study enrolled 5,124 participants who were offspring of the Framingham Original cohort or their spouses. From 2002, the Third Generation cohort recruited 4,095 children of the Framingham Offspring cohort and their spouses. Participants were evaluated approximately every 3–4 years. Each examination included a detailed medical history and physical examination by a study physician, basic anthropometry measures, and assessment of standard cardiovascular and metabolic risk factors. Data for the Framingham Offspring participants were retrieved from examination cycle 7 (1998–2001), and Framingham Third Generation participant data were collected at examination cycle 1 (2002–2005). The study sample for the current investigation includes individuals that were part of the Framingham CT substudy [6]. This subcohort contains mainly individuals residing in the New England area of the USA. Participants were eligible if they were male and ≥35 years of age or female and ≥40 years of age, not pregnant, and with a body weight of <160 kg. Of the 3,370 individuals with available VAT and SAT measurements, we excluded 147 for missing covariates, leaving 3,223 individuals (1,543 women) for the current analyses. All participants provided informed consent and the study complies with the Declaration of Helsinki and was approved by the Institutional Review Board at the Boston University Medical Center.
Risk factor assessment
Serum lipids were assessed after an overnight fast. Diabetes was defined as fasting plasma glucose ≥7.0 mmol/l or use of hypoglycaemic drugs or insulin. Impaired fasting glucose was defined as fasting plasma glucose level of 5.6–6.9 mmol/l in the absence of hypoglycaemic drug treatment. Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg or the intake of antihypertensive drugs. Elevated triacylglycerols were defined as levels ≥1.7 mmol/l or intake of lipid-lowering drugs. Low HDL-cholesterol was defined as <1.29 mmol/l in women and <1.04 mmol/l in men. Current smoking was defined as ≥1 cigarette/day over the last year. Alcohol use was classified as more or less than seven drinks in women and 14 drinks in men per week. The metabolic syndrome was defined by modified Adult Treatment Panel III criteria (impaired fasting glucose defined as above, high triacylglycerol defined as above, blood pressure criteria modified to include antihypertensive treatment) [6]. Insulin was measured using a radioimmunoassay in the Offspring cohort and an enzyme-linked immunosorbent assay in the Third Generation cohort [9]. In the Offspring cohort, the intra-assay coefficient of variation was 3.9% and the inter-assay coefficient of variation had a range of 4.7–6.1%; in the Third Generation cohort the intra-assay coefficient of variation was 2.7% and the inter-assay coefficient of variation was 8.1%. To account for the differing assays used in the two cohorts, all values for the Third Generation cohort were standardised to those for the Offspring cohort [9]. The HOMA of insulin resistance (HOMA-IR) was calculated for all participants, and insulin resistance was defined as the upper quartile of HOMA-IR [9].
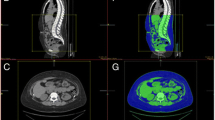
CT measurements
Fat measurement protocols for subcutaneous and abdominal fat have been described in detail elsewhere [10]. Briefly, participants underwent assessment with an eight-slice multidetector computed tomography (CT) scanner (LightSpeed Ultra; General Electric, Milwaukee, WI, USA). Five-millimetre slices were acquired covering 125 mm superiorly from the upper edge of the S1 vertebrae. Fat depots were quantified semi-automatically on a dedicated offline workstation (Aquarius 3D Workstation; TeraRecon Inc., San Mateo, CA, USA). The abdominal muscular wall was traced manually to separate VAT from the SAT depot. Inter- and intra-reader reproducibility was excellent (intraclass correlations >0.99) for both VAT and SAT measurements [4].
Statistical analyses
Because of the sex interactions we have observed previously [4], all analyses were performed stratified by sex. The VAT/SAT ratio distribution was skewed and therefore natural log-transformed for further analyses. We calculated age-adjusted Pearson correlations of log VAT/SAT ratio with continuous cardiometabolic variables. We further stratified our sample by tertiles of VAT/SAT ratio and calculated age-adjusted means of continuous cardiometabolic traits and age-adjusted prevalence of binary traits for each stratum using linear or logistic regression models. To assess whether the VAT/SAT ratio is associated with cardiovascular risk, we performed multivariable adjusted regressions with cardiometabolic traits as dependent variables and VAT/SAT ratio as independent variable. All models were adjusted for age, current smoking status, alcohol use and physical activity. Menopausal status and hormone replacement were also included in models describing women. Models of lipid traits were, in addition, adjusted for lipid-lowering treatment, models of fasting glucose were adjusted for treatment of diabetes, and blood pressure models were also adjusted for hypertension treatment. In a second modelling step, we added BMI as a covariate to the models, and in a third step, we further adjusted for VAT (in addition to BMI). All analyses were performed using SAS Version 9.1 (SAS Institute, Cary, NC, USA).
Results
The clinical and biochemical characteristics of the study sample are given in Table 1. Overall 1,543 women and 1,680 men were available for the current analyses. The mean age was 51.8 years in women and 49.5 years in men and the median VAT/SAT ratio was 0.39 in women and 0.84 in men.
Pearson correlation coefficients of log-transformed VAT/SAT ratio with cardiometabolic traits are given in Table 2. The VAT/SAT ratio was positively correlated with age in both sexes (r = 0.42 and r = 0.37). In women, VAT/SAT ratio was weakly correlated with increasing BMI (r = 0.06) and waist circumference (r = 0.10), whereas in men there were inverse correlations of VAT/SAT ratio with BMI and waist (r = −0.14 and r = −0.16). In women, the VAT/SAT ratio showed a stronger correlation with VAT (r = 0.53) than with SAT (r = −0.11), whereas in men correlations were of similar magnitude for VAT and SAT (r = 0.42 and r = −0.43). In both women and men, a higher VAT/SAT ratio was correlated with more adverse levels of the risk factors examined.
Age-adjusted means or prevalence of cardiovascular risk factors, partitioned by sex and tertiles of VAT/SAT ratio, are provided in Table 3. In women, the prevalence of hypertension, impaired fasting glucose, insulin resistance (defined by HOMA-IR), diabetes, the metabolic syndrome and current smoking increased significantly with tertiles of VAT/SAT ratio (all p < 0.0001 for trend, except diabetes: p = 0.001). In men, trends were similar, but generally weaker.
We next explored the association of VAT/SAT ratio with cardiometabolic traits in multivariable adjusted models (Table 4). In women, higher VAT/SAT ratio was associated with higher levels of all assessed cardiometabolic traits (or with lower levels for HDL-cholesterol) reflecting blood pressure, glucose homeostasis and dyslipidaemia (all p < 0.0003). In men, findings were similar, although associations were generally weaker and did not reach significance (p > 0.05) for fasting glucose, impaired fasting glucose, insulin resistance and diabetes.
To assess whether VAT/SAT ratio is associated with cardiometabolic traits independent of BMI, we additionally adjusted our models for BMI. In women, associations of VAT/SAT ratio with cardiometabolic risk factors remained fairly stable after BMI adjustment. In men, BMI-adjustment strengthened several associations, including those with fasting glucose (p = 0.0005), impaired fasting glucose (p = 0.01) and insulin resistance (p < 0.0001). Figure 1 depicts adjusted means of systolic blood pressure, fasting glucose, HDL-cholesterol and log-transformed triacylglycerols, partioned by sex-specific tertiles of VAT/SAT ratio. Additional adjustment for waist circumference did not materially change our findings (data not shown).
VAT-SAT ratio tertiles and risk factors. Multivariable (including BMI)-adjusted means of fasting glucose (a), systolic blood pressure (SBP) (b), log-transformed triacylglycerols (c) and HDL-cholesterol (HDL) (d), partitioned by sex-specific tertiles of VAT/SAT ratio (black columns, women; grey columns, men)
To further explore whether the VAT/SAT ratio is a correlate of cardiometabolic risk independent of VAT, we additionally adjusted our models for VAT (Table 4; the effect estimates for VAT in these models are given in electronic supplementary material [ESM] Table 1). In the VAT-adjusted models, several associations of VAT/SAT ratio in women were attenuated, but those with lower HDL-cholesterol, higher triacylglycerols (both p < 0.0001) and higher prevalence of hypertension (p = 0.02), diabetes (p = 0.01) and the metabolic syndrome (p = 0.005) remained significant. Similarly, in men, additional VAT-adjustment attenuated some associations, but those with higher systolic (p = 0.006) and diastolic blood pressure (p = 0.03), higher fasting glucose (p = 0.0005), lower HDL-cholesterol and higher triacylglycerols (both p < 0.0001) and higher prevalence of diabetes (p = 0.006) remained significant.
To assess the potential impact of menopause on our observations in women, we stratified our female study sample by menopausal status in a secondary analysis. We observed similar associations between VAT/SAT ratio and cardiometabolic risk in pre- and postmenopausal women (ESM Table 2).
Discussion
Principal findings
We cross-sectionally analysed cardiometabolic correlates of VAT/SAT ratio (a measure of body fat distribution between VAT and SAT compartments) in the Framingham Heart Study cohort. We observed that in women, the VAT/SAT ratio demonstrated a weak, positive correlation with BMI and waist circumference. Conversely, in men, the VAT/SAT ratio was inversely associated with BMI and waist circumference. In both sexes, the VAT/SAT ratio was a significant correlate of several cardiometabolic risk factors, above and beyond associations with BMI and VAT. These findings suggest that ectopic fat distribution, independent of the absolute fat quantity, is a correlate of metabolic risk.
We have hypothesised that the VAT/SAT ratio is a metric of the propensity to store fat viscerally relative to subcutaneous fat stores. The ‘lipid overflow ectopic fat model’ suggests that surplus energy is physiologically primarily stored in subcutaneous compartments, and that when this depot is dysfunctional, energy can alternatively be deposited in visceral compartments [11]. Failure of adipocyte proliferation and differentiation has been discussed as a possible mechanism of functional SAT insufficiency [12]. Lipodystrophy is characterised by SAT dysfunction leading to marked increases in visceral and ectopic fat storage with a paucity of subcutaneous fat. Visceral fat may cause hepatic insulin resistance by releasing a variety of biologically active molecules, such as NEFAs and inflammatory mediators, into the portal vein system (‘portal vein hypothesis’) [11, 13]. Taken together, the propensity to store energy viscerally as compared with subcutaneously may be both a cause and a consequence of multiple different factors, including insulin resistance, smoking, stress and lack of physical activity, and may also be influenced by glucocorticosteroids and sex hormones [11, 12, 14, 15].
Pharmacological studies suggest that the VAT/SAT ratio may be a determinant of metabolic risk. The VAT/SAT ratio can be lowered by thiazolidinedione (‘insulin sensitiser’) treatment, which expands SAT volume and reduces VAT [16], leading to improved insulin sensitivity despite weight gain [17–19]. Conversely, drugs can also cause lipodystrophy, specifically as a common side effect of HIV protease-inhibitor therapy. This adverse pattern of fat redistribution corresponds to a higher VAT/SAT ratio [20], and is associated with insulin resistance and dyslipidaemia [21]. Hence, even though not associated with weight gain [20] (in fact, often weight loss [22]), protease-inhibitor-induced lipodystrophy demonstrates the metabolic profile of the metabolic syndrome [21].
VAT/SAT ratio, other measures of body fat, and sex differences
We observed a weak positive correlation of VAT/SAT ratio with waist circumference in women (and even weaker with BMI), whereas these correlations were modestly inversely associated in men. In a sample of 62 individuals, Gastaldelli and colleagues observed a weak, but positive, association of VAT/SAT ratio with BMI in both women and men [23]. Our considerably larger analysis supports the notion of a very weak relation between VAT/SAT ratio and BMI, but also suggests a different directionality of this weak association in women and men. Taken together, the VAT/SAT ratio appears to provide information that is independent of standard measures of generalised or abdominal adiposity. Also the relations of VAT/SAT ratio with VAT and SAT differ between sexes: in women, VAT/SAT ratio was to a much larger extent determined by VAT than by SAT, whereas in men, VAT and SAT contributed more similarly to the VAT/SAT ratio.
Generally, associations of the VAT/SAT ratio with cardiovascular risk factors were stronger in women than in men. In women, higher levels of the VAT/SAT ratio were also associated with current smoking, with a more than twofold increase in smoking prevalence from the lowest to the highest VAT/SAT ratio tertile. We have previously reported that women who currently smoke have somewhat higher VAT and lower SAT than non-smokers or ex-smokers [24]. The principles underlying this sex-specific association are not entirely clear, but may be related to a decreased bioavailability of oestrogen in smokers [25]. Oestrogen plays an important role in regulating metabolism and lipogenesis [26]. Also, nicotine increases metabolic rate [27] and inhibits appetite [28], which may result in lower SAT. Alternatively, the association between current smoking and higher VAT/SAT ratio may be mediated by other nutritional or lifestyle factors related to smoking.
VAT/SAT ratio and cardiovascular risk
Several studies have investigated the correlation of either VAT or SAT with cardiometabolic risk, and many have concluded that VAT is a stronger correlate of cardiometabolic risk than SAT [3, 4, 11]. However, little is known regarding how the relative distribution of fat between visceral and subcutaneous compartments is associated with cardiometabolic traits. Some smaller studies have previously reported a positive association of VAT/SAT ratio with cardiovascular risk factors [23, 29–31]. In their paper based on 62 individuals, Gastaldelli et al [23] reported that VAT/SAT ratio was associated with fasting glucose (whereas SAT or VAT alone were not). Conversely, VAT alone was associated with fasting insulin and insulin sensitivity, whereas VAT/SAT ratio was not. Notably, these analyses were conducted after pooling sexes. Miyazaki and DeFronzo [29] reported that, in a sample of 36 men with type 2 diabetes, the VAT/SAT ratio correlated with endogeneous glucose production during insulin clamp (a measure of hepatic insulin resistance), whereas VAT or SAT alone did not. In contrast, total glucose disposal (a measure of peripheral insulin sensitivity) correlated inversely with VAT and SAT, but not with VAT/SAT ratio. He et al [30] observed that, in a sample of 437 individuals, the VAT/SAT ratio was independently associated with cardiometabolic risk factor clustering in women (n = 197), whereas in men VAT was a stronger correlate of cardiometabolic risk than the VAT/SAT ratio. In a sample of 13 spinal cord injury patients, Gorgey et al reported an inverse association of VAT/SAT ratio with fasting insulin [31]. A recent investigation by Kim et al [32] demonstrated that, in a Korean population, a higher SAT/VAT ratio (i.e. the inverse of our trait) was associated with lower prevalence of the metabolic syndrome, higher HDL-cholesterol, lower triacylglycerol and lower fasting glucose, even after adjustment for BMI. Our data is consistent with this study, and extends these findings to a large white population. We furthermore demonstrate that the VAT/SAT ratio is a correlate of cardiometabolic risk above and beyond BMI and VAT. These observations suggest that the propensity to store energy in visceral vs subcutaneous fat compartments is a correlate of metabolic dysregulation, independent of overall obesity and absolute visceral fat mass. Of note, our study was not designed to demonstrate that VAT/SAT is a stronger correlate of cardiometabolic risk than VAT alone. In fact, when we evaluated VAT and VAT/SAT jointly, VAT was associated with several cardiometabolic traits independently of the VAT/SAT ratio and, in particular, was associated with some traits that were not independently related to VAT/SAT ratio.
Strengths and limitations
Several strengths of our study warrant mention. We used a highly reproducible, highly specific CT-derived volumetric assessment of fat depots rather than anthropometric surrogate measures of body fat composition. The design of the Framingham Heart Study with regular examinations in the dedicated on-site participants clinic assures high quality of clinical and biochemical data. Limitations of our study are the observational design, precluding any definite causal inference. Furthermore, our study cohort is middle-aged and primarily white. Although our findings are similar to observations made in an Asian population [32], generalisibility to other age groups and ethnic groups remains to be shown. Also, we only assessed HOMA-IR as a measure of insulin resistance. However, more sophisticated methods such as hyperinsulinaemic euglycaemic clamp were not feasible in our large community-based cohort. Last, as hip measurements are not part of the Framingham study protocols, we were not able to compare VAT/SAT ratio with waist/hip ratio.
Conclusion
We demonstrate in a large community-based sample that VAT/SAT ratio—a measure of relative body fat distribution—is a unique correlate of metabolic risk, independent of BMI and VAT. These findings suggest that the propensity for ectopic, relative to subcutaneous, fat deposition is associated with increased cardiovascular risk, independent of overall obesity and absolute visceral fat mass.
Abbreviations
- CT:
-
Computed tomography
- HOMA-IR:
-
HOMA of insulin resistance
- SAT:
-
Subcutaneous adipose tissue
- VAT:
-
Visceral adipose tissue
References
Mokdad AH, Ford ES, Bowman BA et al (2003) Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289:76–79
Kaess BM, Jozwiak J, Mastej M et al (2010) Association between anthropometric obesity measures and coronary artery disease: a cross-sectional survey of 16,657 subjects from 444 Polish cities. Heart 96:131–135
Liu J, Fox CS, Hickson DA et al (2010) Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab 95:5419–5426
Fox CS, Massaro JM, Hoffmann U et al (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116:39–48
Tran TT, Yamamoto Y, Gesta S, Kahn CR (2008) Beneficial effects of subcutaneous fat transplantation on metabolism. Cell Metab 7:410–420
Porter SA, Massaro JM, Hoffmann U, Vasan RS, O’Donnel CJ, Fox CS (2009) Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care 32:1068–1075
Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP (1979) An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol 110:281–290
Splansky GL, Corey D, Yang Q et al (2007) The Third Generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 165:1328–1335
Preis SR, Massaro JM, Robins SJ et al (2010) Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obesity (Silver Spring) 18:2191–2198
Maurovich-Horvat P, Massaro J, Fox CS, Moselewski F, O’Donnell CJ, Hoffmann U (2007) Comparison of anthropometric, area- and volume-based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi-detector computed tomography. Int J Obes (Lond) 31:500–506
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887
Heilbronn L, Smith SR, Ravussin E (2004) Failure of fat cell proliferation, mitochondrial function and fat oxidation results in ectopic fat storage, insulin resistance and type II diabetes mellitus. Int J Obes Relat Metab Disord 28(Suppl 4):S12–S21
Bjorntorp P (1990) 'Portal’ adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 10:493–496
Matsuzawa Y, Shimomura I, Nakamura T, Keno Y, Kotani K, Tokunaga K (1995) Pathophysiology and pathogenesis of visceral fat obesity. Obes Res 3(Suppl 2):187S–194S
Lee MJ, Gong DW, Burkey BF, Fried SK (2010) Pathways regulated by glucocorticoids in omental and subcutaneous human adipose tissues: a microarray study. Am J Physiol Endocrinol Metab 300:E571–E580
Miyazaki Y, Mahankali A, Matsuda M et al (2002) Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab 87:2784–2791
Akazawa S, Sun F, Ito M, Kawasaki E, Eguchi K (2000) Efficacy of troglitazone on body fat distribution in type 2 diabetes. Diabetes Care 23:1067–1071
Nakamura T, Funahashi T, Yamashita S et al (2001) Thiazolidinedione derivative improves fat distribution and multiple risk factors in subjects with visceral fat accumulation – double-blind placebo-controlled trial. Diabetes Res Clin Pract 54:181–190
Yang X, Smith U (2007) Adipose tissue distribution and risk of metabolic disease: does thiazolidinedione-induced adipose tissue redistribution provide a clue to the answer? Diabetologia 50:1127–1139
Miller KD, Jones E, Yanovski JA, Shankar R, Feuerstein I, Falloon J (1998) Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 351:871–875
Troll JG (2011) Approach to dyslipidemia, lipodystrophy, and cardiovascular risk in patients with HIV infection. Curr Atheroscler Rep 13:51–56
Carr A, Samaras K, Burton S et al (1998) A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS 12:F51–F58
Gastaldelli A, Sironi AM, Ciociaro D et al (2005) Visceral fat and beta cell function in non-diabetic humans. Diabetologia 48:2090–2096
Molenaar EA, Massaro JM, Jacques PF et al (2009) Association of lifestyle factors with abdominal subcutaneous and visceral adiposity: the Framingham Heart Study. Diabetes Care 32:505–510
Michnovicz JJ, Hershcopf RJ, Naganuma H, Bradlow HL, Fishman J (1986) Increased 2-hydroxylation of estradiol as a possible mechanism for the anti-estrogenic effect of cigarette smoking. N Engl J Med 315:1305–1309
Faulds MH, Zhao C, Dahlman-Wright K, Gustafsson JA (2012) The diversity of sex steroid action: regulation of metabolism by estrogen signaling. J Endocrinol 212:3–12
Perkins KA, Epstein LH, Marks BL, Stiller RL, Jacob RG (1989) The effect of nicotine on energy expenditure during light physical activity. N Engl J Med 320:898–903
Mineur YS, Abizaid A, Rao Y et al (2011) Nicotine decreases food intake through activation of POMC neurons. Science 332:1330–1332
Miyazaki Y, DeFronzo RA (2009) Visceral fat dominant distribution in male type 2 diabetic patients is closely related to hepatic insulin resistance, irrespective of body type. Cardiovasc Diabetol 8:44
He H, Ni Y, Chen J et al (2011) Sex difference in cardiometabolic risk profile and adiponectin expression in subjects with visceral fat obesity. Transl Res 155:71–77
Gorgey AS, Mather KJ, Gater DR (2011) Central adiposity associations to carbohydrate and lipid metabolism in individuals with complete motor spinal cord injury. Metabolism 60:843–851
Kim S, Cho B, Lee H et al (2011) Distribution of abdominal visceral and subcutaneous adipose tissue and metabolic syndrome in a Korean population. Diabetes Care 34:504–506
Funding
This work was supported by the National Heart, Lung and Blood Institute’s (Bethesda, MD, USA) Framingham Heart Study (N01-HC-25195).
Duality of interest
A. Pedley is a Merck employee and owns Merck stock. All other authors declare that they have no duality of interest associated with this manuscript.
Contribution statement
BMK coordinated analyses, interpreted results and wrote the manuscript. AP performed statistical analyses and revised the manuscript. JMM advised and supervised statistical analyses and revised the manuscript. JM contributed to study design, data interpretation and manuscript revision. UH contributed to data interpretation and manuscript revision. CSF designed and led the project and revised the manuscript. All authors have approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
PDF 22.9 kb
ESM Table 2
PDF 29.6 kb
Rights and permissions
About this article
Cite this article
Kaess, B.M., Pedley, A., Massaro, J.M. et al. The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia 55, 2622–2630 (2012). https://doi.org/10.1007/s00125-012-2639-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2639-5