Abstract
Background
Repeated use of a psychiatric emergency room (PER) is inadequate, and revolving door patients represent a burden on PER. Their socio-demographic and diagnostic profiles need to be better documented to enable early identification.
Methods
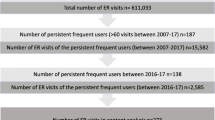
A retrospective study was undertaken over a 16-month period following the initial visit. Non-repeaters, occasional (2–3 contacts) or frequent repeaters (4 or more) were compared with univariate and logistic regression techniques.
Results
Frequent repeaters—4% of 2,470 patients and 15% of 3,511 contacts—were more likely to be younger socially handicapped males stressed by grief, pharmaceutical drug misusers and self-referred with no previous hospitalization history. The diagnostic profile was a mixture of severity (psychosis) and less structured complaints (secondary depressive disorder). Disposition upon first contact was temporary hospitalization at PER revealing case assessment difficulties. A continuum of social disability from occasional to frequent repetition of contact was observed.
Conclusion
Repeaters have characteristics that may permit early identification. Their diagnosis, a mixture of non-specific complaints and primarily residual or disorganized schizophrenia, defies evaluation and adequate treatment. Networking with services able to provide help for this type of patient would alleviate the burden on PER. If not available within the community, the development of an ad hoc program should be considered.
Similar content being viewed by others
References
Adityanjee MD, Mohan D, Wig NN (1988) Unwelcome guests: bugbears of the emergency room physician. Int J Soc Psychiatry 34:196–199
Arfken CL, Zeman LL, Yeager L, Mischel E, Amirsadri A (2002) Frequent visitors to psychiatric emergency services: staff attitudes and temporal patterns. J Behav Health Serv Res 29(4):490–496
Arfken CL, Zeman LL, Yeager L, White A, Mischel E, Amirsadri A (2004) Case-control study of frequent visitors to an urban psychiatric emergency service. Psychiatr Serv 55:295–301
Bassuk E, Gerson S (1980) Chronic crisis patients: a discrete clinical group. Am J Psychiatry 137:1513–1517
Dhossche DM, Ghani SO (1989) A study on recidivism in the psychiatric emergency room. Hosp Community Psychiatry 40:958–960
Ellison JM, Blum NR, Barsky AJ (1989) Frequent repeaters in a psychiatric emergency service. Hosp Community Psychiatry 40:958–960
Gerson S, Bassuk E (1980) Psychiatric emergencies: an overview. Am J Psychiatry 137(1):1–11
Hansel TE, Elliott KD (1993) Frequent psychiatric visitors to a Veterans Affairs Medical Center emergency care unit. Hosp Community Psychiatry 44:376–380
Kent S, Yellowlees P (1993) The relationship between social factors and frequent use of psychiatric services. Hosp Community Psychiatry 44:372–375
Oyewumi LK, Odejide O, Kazarian SS (1992) Psychiatric emergency services in a Canadian city. 1. Prevalence and patterns of use. Can J Psychiatry 37:91–95
Passic J, Russo J, Roy-Byrne P (2005) High utilizers of psychiatric emergency services. Psychiatr Serv 56:678–684
Perez E, Minoletti A, Blouin J, Blouin A (1986) Repeated users of a psychiatric emergency service in a Canadian general hospital. Hosp Community Psychiatry 37:37–41
Raphling D, Lion J (1970) Patients with repeated admissions to a psychiatric emergency service. Community Ment Health J 6:313–318
Saarento O, Hakko H, Joukamaa M (1998) Repeated use of psychiatric emergency out-patient services among new patients: a 3-year follow-up study. Acta Psychiatr Scand 98:276–282
Segal SP, Akutsen PD, Watson MA. Factors (1998) Associated with involuntary return to a psychiatric emergency service within 12 months. Psychiatr Serv 49:1212–1217
Segal SP, Akutsen PD, Watson MA (2002) Involuntary return to a psychiatric emergency service within twelve months. Soc Work Health Care 35(1–2):591–603
Spooren DJ, De Bacquer D, Van Heeringen K, Jannes C (1997) Repeated psychiatric referrals to Belgian emergency departments: a survival analysis of the time interval between first and second episodes. Eur J Emerg Med 2:61–67
Sullivan PF, Bulik CM, Forman SD, Mezzich JE (1993) Characteristics of repeat users of a psychiatric emergency service. Hosp Community Psychiatry 44:376–380
Warwick HMC, Solkovskis PM (1985) Reassurance. Br Med J 290:1028
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ledoux, Y., Minner, P. Occasional and frequent repeaters in a psychiatric emergency room. Soc Psychiat Epidemiol 41, 115–121 (2006). https://doi.org/10.1007/s00127-005-0010-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0010-6