Abstract
Objective
To document the prevalence of respiratory virus infections in patients with chronic cardiac or pulmonary disorders admitted to a critical care unit for acute cardiorespiratory failure.
Design, setting, patients
The study took place in a critical care unit during two consecutive winters. All patients admitted to the unit for acute respiratory or cardiac failure were enrolled. A nasal swab was taken for polymerase chain reaction (PCR) detection of influenza virus, respiratory syncytial virus (RSV), metapneumovirus, rhinovirus, and coronavirus.
Results
One hundred twenty-two patients were enrolled. Their mean age was 69 years; 42% of the patients were female; the new simplified acute physiology score (SAPS II) score on admission was 35.6; 94% of patients had acute respiratory failure, 14% reported “influenza-like” illness before admission, and 11% of patients died in the unit. Twenty-one patients (17%) tested positive for a respiratory virus. The per-1,000 positivity rates were influenza virus 66, RSV 49, rhinovirus 33, metapneumovirus 16, and coronavirus 8. No link was found between virologic results and clinical outcome. A strong link was found between the rate of influenza virus positivity and the incidence of flu-like illness in the community (p=0.017).
Conclusion
These results show that respiratory virus infection—particularly influenza virus infection during epidemic periods—is common among patients hospitalized for acute cardiorespiratory failure.
Similar content being viewed by others
Introduction
Respiratory viruses, particularly influenza virus and respiratory syncytial virus (RSV), are often described as potential triggers of acute respiratory or cardiac failure in frail individuals. In studies of elderly people hospitalized for acute cardiopulmonary disorders or influenza-like illness, influenza was diagnosed in 11% of cases and RSV infection in 10% of cases [1, 2]. Other respiratory pathogens, such as rhinoviruses, coronaviruses, and human metapneumoviruses, have rarely been studied in this setting, but some data suggest a high prevalence of infection [3, 4]. The respective frequencies of these pathogens in patients admitted to critical care units (CCUs) have not previously been reported. Our objective was to document the prevalence of respiratory virus infection in patients with chronic cardiac or pulmonary disorders admitted to a CCU for acute respiratory or cardiac failure.
Material and methods
The study took place in a 14-bed CCU located in a 970-bed university hospital in Paris. The Institutional Review Board of the French Society of Critical Care Medicine approved the study protocol. We enrolled all patients admitted to the CCU between 15 October 2002 and 20 March 2003 or between 17 November 2003 and 2 February 2004 for acute respiratory or cardiac failure and who had a chronic cardiac or pulmonary disorder warranting specific treatment. No exclusion criteria were applied. Enrollment took place Monday through Friday. Two nasal swab samples were collected and stored in 3 ml of viral transportation medium, which was prepared in the virology laboratory. One ml of transport medium contained 29.5 mg of tryptose phosphate broth and 5.0 mg of gelatin (Beckton Dickinson, Le Pont de Claix, France), 50 units penicillin, 50 mg streptomycin, and 0.0125 µg amphotericin B (antibiotic antimycotic solution, Sigma, Saint Quentin Fallavier, France). Demographic data, medical history, hospital course, and discharge diagnosis were collected prospectively in each case. Screening for respiratory viruses was based on reverse-transcription polymerase chain reaction amplification (RT-PCR). Viral RNA was extracted from 140 µl of nasal swab samples with the Qiagen viral RNA extraction kit (Qiagen, Courtaboeuf, France). Real-time amplification was performed after cDNA synthesis with random hexamers included in the Applera RT RNA transcription kit (Courtaboeuf, France) as previously described [5]. We used previously described primers and probes to amplify influenza A virus [5], influenza B virus [6], RSV A and B [7], and metapneumovirus [8]. Quantification was achieved by using cycle threshold (Ct) values; Ct values of 35–40, 26–34, and <26 were graded weak, medium, and strong positive, respectively. Conventional RT-PCR methods were used for coronavirus 229 E, coronavirus OC43, and rhinovirus. PCR amplification was done using the Titan One-Tube RT-PCR system (Roche Diagnostics, Meylan, France) and primers described by Pitkaranta et al. [9] in an Applera 9600 Thermocycler. Nested PCR was used for rhinovirus detection with the specific inner primers 5’-TCA ATG AGG ATA TGC TTT AC-3’ and 5’-CGG ACA CCC AAA GTA G-3’. Positive and negative controls were tested in each run.
Data on influenza-like illness in Paris and the surrounding area (Ile-de-France), used as a surrogate for influenza virus infection in the community, were obtained from the French sentinel network [10]. The study periods were chosen to encompass the annual influenza-like illness epidemic.
Statistics
The Kruskal-Wallis test was used for continuous variables, and Fisher’s exact test was used for categorical variables. A univariate logistic regression model was used to examine the link between the weekly incidence of flu-like illness in the community (independent variable) and the rate of influenza virus positivity in the CCU (dependent variable). A p-value <0.05 was considered statistically significant.
Results
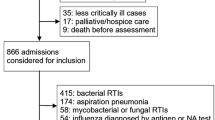
Seventy-five of the 387 patients admitted to the CCU during the first period and 47 of the 325 patients admitted during the second period were enrolled in the study. All of these patients were admitted directly to the CCU. There were significantly more women in the first period than in the second period (49% vs. 30%, p=0.04). The other demographic and clinical characteristics of the patients enrolled during the two winters were similar. Mean age was 69 years [standard deviation (SD) 14], and the new simplified acute physiology score (SAPS II) was 35.6 (SD 17.3; see Table 1). Twenty-three percent of patients were receiving treatment for heart disease, 47% for respiratory disease, and 30% for both. The chronic respiratory disorders were chronic respiratory failure in 74, asthma in 12, lung cancer in three, and other disorders in five. The cardiac disorders were ischemic heart disease in 23 patients, hypertension in 14, chronic heart failure in 10, atrial fibrillation in seven, valvular disease in two, and other cardiac disorders in nine. Twenty-two percent of patients were receiving inhaled corticosteroids. Ninety-four percent of patients were admitted for acute respiratory failure and 13% for acute cardiac failure. The main admission diagnoses were acute exacerbations of chronic respiratory failure in 71, non-chronic obstructive pulmonary disease (COPD)-related acute lung injury in 17, severe asthma in 10, pneumonia in 10, acute pulmonary edema in six, cardiogenic shock in four, and other cardiorespiratory disorders in four. Fourteen percent of patients recalled “flu-like” symptoms within the 10 days prior to CCU admission. Three of these patients were PCR-positive (two influenza, one RSV), while three patients had bacterial pneumonia (twp Streptococcus pneumoniae, one Haemophilus influenzae). Thirty-five percent of patients stated they had received the latest influenza vaccine. Thirteen patients died in the CCU. The median length of CCU stay was 5 days (interquartile range 2–10 days).
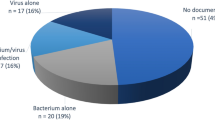
Nine patients (12%) were PCR-positive for a respiratory virus during the first period (four RSV, two rhinovirus, two metapneumoviruses, and one influenza), and 12 patients (26%) were positive in the second period (seven influenza, two RSV, two rhinovirus, and one coronavirus OC43; see Fig. 1). Samples were collected within 24 h, 48 h, or 96 h after admission in 73%, 16%, and 11% of cases. The interval between admission and sample collection did not influence the virologic results (p=0.40). All but one of the RSV- and influenza-positive samples were graded strongly positive. One influenza-positive sample was graded medium positive, and the two metapneumovirus-positive samples were graded weakly positive.
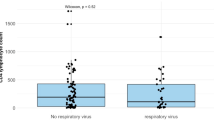
No link was found between the virologic results and demographic characteristics or clinical outcome (Table 1). One (12.5%) of the influenza-positive patients had been vaccinated, compared with 38 (37%) of the influenza-negative patients (p=0.26).
The likelihood of influenza virus positivity in a given week increased 1.3-fold (95% CI 1.1, 1.7) when the incidence of flu-like illness in the community increased by one point per 1,000 inhabitants during the same week (p=0.02), and it increased 1.9-fold (95% CI 1.0, 3.9) when the incidence increased by one point per 1,000 inhabitants aged 65 years or older (p=0.06).
Discussion
This study shows that respiratory viruses, as detected with a highly sensitive method, are common among patients admitted for cardiorespiratory failure. Up to one in four patients who were admitted during the epidemic period of flu-like illness were positive for such viruses.
The significance of a positive respiratory virus PCR test has been debated in the literature. Some data indicate that there is no chronic shedding or carriage of respiratory virus RNA in immunocompetent individuals [11]. It is noteworthy that influenza virus RNA is no longer detectable in samples collected 10 days after disease onset [6]. For rhinovirus RNA, the corresponding interval is 2 weeks in most individuals, and it never exceeds 5 weeks [12]. These findings suggest that our PCR-positive patients had been infected recently, most of them within the 2 weeks before admission. However, patients with stable COPD may be transiently colonized by RSV, although viral load is lower than during acute infection [13, 14]. Using a quantitative scoring system, we found that all RSV-positive samples were strongly positive, supporting the probability that RSV positivity was related to acute viral infection of the airways.
The cumulative incidence of influenza-like illness in individuals aged 65 years or older during the two periods studied here was 0.4% and 1.3%, respectively. The rate of PCR positivity for influenza virus during the second period was 11.7% (p<0.001, compared with 1.3% and adjusted for age). We therefore believe that these PCR-positive patients were infected at a higher than expected frequency, indicating a positive association between infection and acute respiratory or cardiac failure. Our rates of influenza and RSV infection are consistent with the 10–18% of influenza positivity and the 10–12% of RSV positivity observed in prospective surveys of elderly patients with chronic cardiorespiratory diseases who were hospitalized in general medical-surgical hospitals with acute cardiopulmonary conditions [1, 2, 15]. The mechanisms by which these infections may have caused acute respiratory or cardiac failure were not studied. However, a causal relationship between influenza virus infection and hospitalization for respiratory or cardiac disease has been detected in vaccine effectiveness studies [16, 17], which showed that influenza immunization reduced hospitalizations. It seems likely that other respiratory viruses have the capacity to trigger severe illnesses in patients with underlying chronic conditions. This calls for more explanatory studies and should lead to increased vigilance for these infections.
Finally, although the difference was not significant, probably owing to the small number of positive patients, the higher rate of PCR positivity among unvaccinated patients supports influenza vaccination of frail individuals. Our results also call for better treatment and prevention of infections by these respiratory pathogens, such as wider influenza vaccine coverage of elderly and high-risk adults, increased use of antivirals for influenza treatment or contact prophylaxis, and development of new treatments or vaccines for RSV infection.
References
Falsey AR, Cunningham CK, Barker WH, Kouides RW, Yuen JB, Menegus M, Weiner LB, Bonville CA, Betts RF (1995) Respiratory syncytial virus and influenza A infections in the hospitalized elderly. J Infect Dis 172:389–394
Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE (2005) Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med 352:1749–1759
Falsey AR, Walsh EE, Hayden FG (2002) Rhinovirus and coronavirus infection-associated hospitalizations among older adults. J Infect Dis 185:1338–1341
Falsey AR, Erdman D, Anderson LJ, Walsh EE (2003) Human metapneumovirus infections in young and elderly adults. J Infect Dis 187:785–790
Carrat F, Sahler C, Rogez S, Leruez-Ville M, Freymuth F, Le Gales C, Bungener M, Housset B, Nicolas M, Rouzioux C (2002) Influenza burden of illness: estimates from a national prospective survey of household contacts in France. Arch Intern Med 162:1842–1848
van Elden LJ, Nijhuis M, Schipper P, Schuurman R, van Loon AM (2001) Simultaneous detection of influenza viruses A and B using real-time quantitative PCR. J Clin Microbiol 39:196–200
Hu A, Colella M, Tam JS, Rappaport R, Cheng SM (2003) Simultaneous detection, subgrouping, and quantitation of respiratory syncytial virus A and B by real-time PCR. J Clin Microbiol 41:149–154
Maertzdorf J, Wang CK, Brown JB, Quinto JD, Chu M, de Graaf M, van den Hoogen BG, Spaete R, Osterhaus AD, Fouchier RA (2004) Real-time reverse transcriptase PCR assay for detection of human metapneumoviruses from all known genetic lineages. J Clin Microbiol 42:981–986
Pitkaranta A, Arruda E, Malmberg H, Hayden FG (1997) Detection of rhinovirus in sinus brushings of patients with acute community-acquired sinusitis by reverse transcription-PCR. J Clin Microbiol 35:1791–1793
Carrat F, Flahault A, Boussard E, Farran N, Dangoumau L, Valleron AJ (1998) Surveillance of influenza-like illness in France. The example of the 1995/1996 epidemic. J Epidemiol Community Health 52(Suppl 1):32S–38S
Nokso-Koivisto J, Kinnari TJ, Lindahl P, Hovi T, Pitkaranta A (2002) Human picornavirus and coronavirus RNA in nasopharynx of children without concurrent respiratory symptoms. J Med Virol 66:417–420
Jartti T, Lehtinen P, Vuorinen T, Koskenvuo M, Ruuskanen O (2004) Persistence of rhinovirus and enterovirus RNA after acute respiratory illness in children. J Med Virol 72:695–699
Borg I, Rohde G, Loseke S, Bittscheidt J, Schultze-Werninghaus G, Stephan V, Bufe A (2003) Evaluation of a quantitative real-time PCR for the detection of respiratory syncytial virus in pulmonary diseases. Eur Respir J 21:944–951
Seemungal T, Harper-Owen R, Bhowmik A, Moric I, Sanderson G, Message S, Maccallum P, Meade TW, Jeffries DJ, Johnston SL, Wedzicha JA (2001) Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med 164:1618–1623
Walsh EE, Falsey AR, Hennessey PA (1999) Respiratory syncytial and other virus infections in persons with chronic cardiopulmonary disease. Am J Respir Crit Care Med 160:791–795
Nichol KL, Baken L, Nelson A (1999) Relation between influenza vaccination and outpatient visits, hospitalization, and mortality in elderly persons with chronic lung disease. Ann Intern Med 130:397–403
Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M (2003) Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med 348:1322–1332
Acknowledgments
We thank Michelle Pecking (Roche, France) for helpful comments, Yves Dorléans and Elisa Vergu (French Sentinelle network) for technical assistance, and David Young for a critical review of the manuscript. We are indebted to the patients who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no conflicts of interest. The study was supported by a grant from Roche (France).
Rights and permissions
About this article
Cite this article
Carrat, F., Leruez-Ville, M., Tonnellier, M. et al. A virologic survey of patients admitted to a critical care unit for acute cardiorespiratory failure. Intensive Care Med 32, 156–159 (2006). https://doi.org/10.1007/s00134-005-2861-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2861-4