Abstract
Objective
To assess whether the passive leg raising test can help in predicting fluid responsiveness.
Design
Nonsystematic review of the literature.
Results
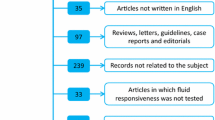
Passive leg raising has been used as an endogenous fluid challenge and tested for predicting the hemodynamic response to fluid in patients with acute circulatory failure. This is now easy to perform at the bedside using methods that allow a real time measurement of systolic blood flow. A passive leg raising induced increase in descending aortic blood flow of at least 10% or in echocardiographic subaortic flow of at least 12% has been shown to predict fluid responsiveness. Importantly, this prediction remains very valuable in patients with cardiac arrhythmias or spontaneous breathing activity.
Conclusions
Passive leg raising allows reliable prediction of fluid responsiveness even in patients with spontaneous breathing activity or arrhythmias. This test may come to be used increasingly at the bedside since it is easy to perform and effective, provided that its effects are assessed by a real-time measurement of cardiac output.
Similar content being viewed by others
Physiological changes in hemodynamics during PLR
Lifting the legs in the event of circulatory collapse is a rescue maneuver that has been used for years by first-aid rescuers. Passive leg raising (PLR) has recently gained interest as a test for monitoring functional hemodynamic and assessing fluid responsiveness since it is a simple way to transiently increase cardiac preload. Lifting the legs passively from the horizontal plane in a lying subject obviously induces a gravitational transfer of blood from the lower part of the body toward the central circulatory compartment and especially toward the cardiac cavities. Using radiolabeled erythrocytes a physiological study in humans demonstrated that the volume of blood contained in the calves was reduced during PLR, a reduction corresponding to the transfer of approx. 150 ml blood [1]. Thus PLR recruits a part of blood contained in the venous reservoir and converts unstressed volume to stressed volume. In turn PLR increases right cardiac preload, likely through an increase in the mean circulatory pressure which is the driving pressure for venous return. If the right ventricle is preload responsive, the increase in systemic venous return results in an increase in right cardiac output and hence in the left ventricular filling. Clinical studies conducted in various hemodynamic conditions have reported an increase in pulmonary artery occlusion pressure [2–5], left ventricular end-diastolic dimension [2, 6], E wave of the mitral flow [2, 3, 7], and left ventricular ejection time [8] during PLR, supporting the evidence that the volume of blood transferred to the heart during PLR is sufficient to increase left cardiac preload. Nonetheless, if the preload reserve of the right heart is limited, the increase in right cardiac preload should not result in an increased flow toward the left ventricle, and thus PLR should not increase left-side preload in such cases. The response to PLR of the markers of right preload (e. g., central venous pressure) and of left preload may therefore differ.
As a result of the increase in left ventricular preload PLR may ultimately result in an increase in cardiac output, depending on the degree of left ventricular preload reserve. Interestingly, Wong and colleagues [9] reported that the increase in stroke volume induced by a 45° leg lifting in healthy subjects was of larger magnitude after withdrawal of 500 ml blood, suggesting that PLR affects cardiac output differently according to the central volume status and thus the degree of cardiac preload reserve. An important point is that the PLR-induced increase in cardiac preload vanishes completely when the legs are returned to horizontal position [5, 8, 10, 11]. Therefore PLR can be considered as a brief and completely reversible “self-volume challenge”. It must also be stressed that the effect of PLR on cardiac output—when it occurs—is not always sustained when the leg elevation is prolonged. In septic shock patients capillary leak may account for this attenuation. In a study including critically ill patients with circulatory failure we observed that the increase in the blood flow of the descending thoracic aorta induced by PLR in “preload-dependent” patients occurred in few seconds and was maximal approx. 1 min after starting the PLR maneuver [8]. In patients who did not have a sustained response to PLR the response to volume infusion also was not sustained. Thus the hemodynamic effects of PLR should be assessed during the time frame of 30–90 s after the onset of the test.
Postural changes during PLR are important to consider. If the trunk is in the semirecumbent position before the maneuver, PLR consists in pivoting the entire body, with the legs lifted up and the trunk ultimately in the horizontal position. With this method one would expect that PLR induces the transfer of a larger blood volume than if the trunk is initially lying horizontally since not only the venous blood of the legs but also that contained into the large splanchnic compartment is mobilized in such a case (Fig. 1; Electronic Supplementary Material, ESM). This should increase the total amount of blood that is mobilized during the postural maneuver.
Postural change during passive leg raising. If at baseline the patient is not lying horizontally but is in semirecumbent position, PLR consists of a simple pivoting of the entire bed. Compared to a case in which the trunk of the patient lies horizontally at baseline, this method is advantageous because (a) it does not change the hip angle, and (b) it may induce the transfer of a larger volume of blood
The response to PLR may also depend upon the ability of the venous reservoir to be recruited. In a patient who is vasoconstricted because of hypovolemic/cardiogenic shock the venous reservoir is likely reduced, and the volume recruited by the PLR would be expected to be less. By contrast, in a patient with a vasodilatory state such as septic shock a higher unstressed volume is expected to be recruited by PLR. Based on this hypothesis, PLR should theoretically increase right ventricle preload less in patients with hypovolemic than in those with septic shock. However, in volume-depleted patients with high volume responsiveness even a moderate increase in preload can result in a significant change in cardiac output. In support of this, the increase in cardiac output in normal subjects in response to PLR has been shown to be increased after blood removal [12].
PLR for testing fluid responsiveness in the critically ill
Facing a hemodynamic failure, the clinician is often tempted to give fluid in order to increase cardiac output by fueling the reservoir in which the heart is pumping. However, fluid administration does not always result in cardiac output enhancement. This comes from the curvilinearity of the Frank–Starling relationship: if the heart is operating on the initial and steep part of the curve, it should have some preload reserve, and any increase in cardiac preload results in an increase in stroke volume. In this case the patient “responds” positively to fluid administration (Fig. 2). In contrast, if the heart is operating on the distal and flat part of the Frank–Starling curve (absence of preload reserve), no significant increase in stroke volume is expected from volume loading. In this case fluid administration may induce harmful effects (e. g., lung inflation, worsening of gas exchange in the case of pulmonary injury, worsening of tissue oxygen transfer) that would not be counterbalanced by any hemodynamic benefit. Thus the need has risen to find diagnostic tools for predicting which shocked patients will respond to fluid administration [13].
Challenging the Frank–Starling curve with the passive leg raising (PLR). In patients with circulatory failure it is not possible to predict the response to volume administration because not just one but numerous curves rely stroke volume and cardiac preload. PLR induces a change in preload that enables to challenge the relationship. If the increase in cardiac preload occurring during the test (from A to B) produces a large increase in stroke volume (from a' to b'), preload responsiveness is likely and the patient should respond to fluid administration. If the increase in stroke volume during the test is of small amplitude (from a to b), preload responsiveness is unlikely and fluid administration should be avoided
Predicting fluid responsiveness solely on the basis of measures of preload must be discouraged. Not only one but a family of Frank–Starling curves rely cardiac preload and stroke volume according to individual factors such as cardiac contractility (Fig. 2). Accordingly, a given value of preload could be associated with preload reserve in patients with normal cardiac contractility but with absence of preload reserve in the case of patients with profoundly impaired contractility because they are on the steep part of their cardiac function curve. Numerous studies now support the evidence that static measures of cardiac preload are not appropriate to assess preload reserve [14, 15]. In this regard cardiac filling pressures such as central venous pressure and pulmonary artery occlusion pressure cannot differentiate between patients responding and patients not responding to fluid administration [16]. Fluid responsiveness assessment must be rather based on the response to dynamic tests which induce transient changes in cardiac preload [17].
Since mechanical ventilation is able to induce cyclic changes in cardiac preload, the respiratory variation in stroke volume has been proposed to assess preload reserve [17]. Accordingly, the respiratory variations in surrogates of stroke volume such as arterial pulse pressure [18], Doppler subaortic flow [19], pulse contour derived stroke volume [20, 21], descending aortic blood flow [22], and even pulse oximetry wave [23] have been demonstrated to predict fluid responsiveness in the critically ill. Nonetheless, such heart–lung interaction indices can be used in only specific conditions, such as regular sinus cardiac rhythm and full adaptation of the patient to the ventilator as during deep sedation or coma. If not, the irregularity of the cardiac rhythm or of the respiratory cycle also account for variability in stroke volume such that fluid responsiveness can no longer be predicted by the variations in stroke volume [8, 24]. In patients with spontaneous ventilation respiratory variation in the central venous pressure has been proposed as an alternative [25]. Conflicting results have subsequently been reported [24], perhaps because the test is effective only in cases of no forced expiration [26].
PLR is an alternative means to predict the hemodynamic response to fluid administration since it can be used as a “self-volume challenge” at the bedside [27]. In mechanically ventilated patients fully adapted to their ventilator PLR-induced changes in stroke volume have been found to be closely correlated with the changes in stroke volume induced by a subsequent 300 ml colloid infusion [5]. Importantly, the hemodynamic changes induced by PLR are not affected by arrhythmias or by ventilator triggering. Therefore the PLR can be still used in circumstances where heart–lung interaction indices are misleading. In a study including 71 shocked patients monitored by esophageal Doppler we investigated whether the response of descending aortic blood flow to PLR predicts fluid responsiveness [8]. Interestingly, PLR increased the aortic flow time—a marker of left cardiac preload—to the same proportion in both responders and nonresponders, suggesting that this test actually performs as a volume challenge. The changes in the descending aortic blood observed during a PLR test were closely correlated with those induced by the subsequent volume expansion. Moreover, a PLR-induced increase in aortic blood flow by more than 10% predicted a fluid-induced increase in aortic blood flow by more than 15% (i. e., fluid responsiveness) with very good sensitivity and specificity [8] (Fig. 3). In the subgroup of patients fully adapted to their ventilator the response to PLR performed equally to pulse pressure respiratory variation in predicting volume responsiveness [8]. More importantly, in the subgroup of patients who triggered their ventilator or who experienced arrhythmias we found that the aortic blood flow response to PLR to predict fluid responsiveness retained its predictive value while pulse pressure variation was no longer reliable [8]. These findings emphasize the specific interest of PLR under conditions where heart–lung interactions indices cannot be interpretable. Recently two studies performed in patients with spontaneous breathing activity demonstrated that an increase in echocardiographic stroke volume by more than 12% in response to PLR well distinguished between responders and nonresponders to fluid administration [11, 28]. In addition, stroke volume response to PLR performed far better than static ultrasonographic indices of cardiac filling such as left ventricular end-diastolic area and Doppler estimates of left ventricular filling pressure [11].
As with any method for predicting response to fluid administration, the cutoff value found for the PLR effects should not be considered as a magic number. Furthermore, sensitivity and specificity values are not absolute. They should be interpreted differently depending upon the clinical context. For instance, the risk of giving fluid unduly may be more dangerous in patients with acute lung injury or acute respiratory distress syndrome. In these cases the physician should administer fluid if the effects of PLR on the cardiac output estimate are clearly above the proposed cutoff value.
Practical aspects of the PLR test
A simple way to perform PLR is to transfer the patient from the 45° semirecumbent to the PLR position by using the automatic pivotal motion of the patient's bed [8] (Fig. 1; see ESM). In addition to its ease of use, this method allows PLR to be performed rapidly without inducing hip flexion and femoral catheters motion. This is important since such procedures should avoid any pain-induced sympathetic stimulation that can result in erroneous interpretation of the hemodynamic effects of PLR. Accordingly, when performed in such a way, PLR did not increase heart rate, suggesting that no confusing sympathetic alteration occurred during the test [8]. Additionally, keeping the thorax in the horizontal position, and not lower, may avoid the risk of gastric inhalation. Nevertheless, it is reasonable to avoid PLR in patients with head trauma since it can increase the intracerebral pressure. Elastic compression stocking may also alter the venous volume recruited by the PLR [29].
Another important point concerns the conditions that must be fulfilled for correct measurement and interpretation of PLR effects. The first condition is that it be a real-time cardiovascular assessment able to track hemodynamic changes in the time frame of PLR effects, i. e., 30–90 s [30] (see ESM). The second is that the limits of precision in the technique used for assessing the response of cardiac output to PLR be far below the 10–15% increase in cardiac output found as a predicting cutoff [30]. PLR-induced changes in arterial pulse pressure [5, 11], descending aorta blood flow [8, 31], pulse contour-derived stroke volume [32], and pulsed Doppler-derived velocity–time integral [11, 28] have been proposed to be used for this purpose. In patients monitored with esophageal Doppler we found that PLR-induced changes in arterial pulse pressure were less accurate than PLR-induced changes in descending aorta blood flow [8] in predicting fluid responsiveness in critically ill patients. This is probably explained by the fact that the descending aorta blood flow is a more direct estimate of cardiac output than arterial pulse pressure [33]. Given the good sensitivity and specificity values reported in recent clinical studies it is likely that other real-time hemodynamic assessment methods such as transthoracic echocardiography (pulsed Doppler subaortic flow) [11, 28] and pulse contour cardiac output monitor [32] can be also appropriately used for quantifying the short-term hemodynamic response to PLR. The third requirement is to ensure that there is actually a change in preload in response to PLR before trying to determine whether there is an increase in cardiac output or preload. In the case of increase in cardiac preload with PLR the absence of increase in stroke volume should indicate that the patient is not fluid responsive. On the other hand, in the case of insufficient increase in preload with PLR (insufficient volume recruitment) the absence of PLR-induced increase in stroke volume cannot be interpreted. In such cases the PLR cannot be used to predict volume responsiveness. Thus it should be recommended to follow the changes in a marker of cardiac preload as a prerequisite to a correct interpretation of the PLR test [34]. Central venous pressure, duration of the aortic flow measured by esophageal Doppler, or end-diastolic dimensions at echocardiography can be used for this purpose. Finally, the level of the intra-abdominal pressure may be important to consider since it can impede the PLR-induced blood transfer when elevated. This point may be one of those that should be addressed by further studies concerning PLR.
In summary, the physiological effects of PLR consist of an increase in venous return and cardiac preload. The PLR thus acts as a self-volume challenge which is easy-to-perform and completely reversible. It has gained an increasing interest in the field of functional hemodynamic monitoring since it can help to detect fluid responsiveness in critically ill patients even in cases of ventilator spontaneous triggering or cardiac arrhythmias. Its optimal use requires a real-time cardiovascular assessment device able to quantify accurately the short-term hemodynamic response.
References
Rutlen DL, Wackers FJ, Zaret BL (1981) Radionuclide assessment of peripheral intravascular capacity: a technique to measure intravascular volume changes in the capacitance circulation in man. Circulation 64:146–152
Pozzoli M, Traversi E, Cioffi G, Stenner R, Sanarico M, Tavazzi L (1997) Loading manipulations improve the prognostic value of Doppler evaluation of mitral flow in patients with chronic heart failure. Circulation 95:1222–1230
Takagi S, Yokota M, Iwase M, Yoshida J, Hayashi H, Sotobata I, Koide M, Saito H (1989) The important role of left ventricular relaxation and left atrial pressure in the left ventricular filling velocity profile. Am Heart J 118:954–962
Rocha P, Lemaigre D, Leroy M, Desfonds P, De Zuttere D, Liot F (1987) Nitroglycerin-induced decrease of carbon monoxide diffusion capacity in acute myocardial infarction reversed by elevating legs. Crit Care Med 15:131–133
Boulain T, Achard JM, Teboul JL, Richard C, Perrotin D, Ginies G (2002) Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 121:1245–1252
Kyriakides ZS, Koukoulas A, Paraskevaidis IA, Chrysos D, Tsiapras D, Galiotos C, Kremastinos DT (1994) Does passive leg raising increase cardiac performance? A study using Doppler echocardiography. Int J Cardiol 44:288–293
Paelinck BP, van Eck JW, De Hert SG, Gillebert TC (2003) Effects of postural changes on cardiac function in healthy subjects. Eur J Echocardiogr 4:196–201
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Wong DH, O'Connor D, Tremper KK, Zaccari J, Thompson P, Hill D (1989) Changes in cardiac output after acute blood loss and position change in man. Crit Care Med 17:979–983
Bertolissi M, Broi UD, Soldano F, Bassi F (2003) Influence of passive leg elevation on the right ventricular function in anaesthetized coronary patients. Crit Care 7:164–170
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL (2007) Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33:1125–1132
Wong DH, Tremper KK, Zaccari J, Hajduczek J, Konchigeri HN, Hufstedler SM (1988) Acute cardiovascular response to passive leg raising. Crit Care Med 16:123–125
Michard F, Teboul JL (2002) Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest 121:2000–2008
Bendjelid K, Romand JA (2003) Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intensive Care Med 29:352–360
Monnet X, Teboul JL (2006) Invasive measures of left ventricular preload. Curr Opin Crit Care 12:235–240
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL (2007) Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med 35:64–68
Pinsky MR, Teboul JL (2005) Assessment of indices of preload and volume responsiveness. Curr Opin Crit Care 11:235–239
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, Perel A (2001) Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 92:984–989
Reuter DA, Felbinger TW, Schmidt C, Kilger E, Goedje O, Lamm P, Goetz AE (2002) Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 28:392–398
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL (2005) Esophageal Doppler monitoring predicts fluid responsiveness in critically ill ventilated patients. Intensive Care Med 31:1195–1201
Feissel M, Teboul JL, Merlani P, Badie J, Faller JP, Bendjelid K (2007) Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med 33:993–999
Heenen S, De Backer D, Vincent JL (2006) How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care 10:R102
Magder SA, Goeogiadis G, Tuck C (1992) Respiratory variations in right atrial pressure predict response to fluid challenge. J Crit Care 7:76–85
Magder S (2006) Predicting volume responsiveness in spontaneously breathing patients: still a challenging problem. Crit Care 10:165
Monnet X, Richard C, Teboul JL (2007) Passive leg raising. In: Vincent JL (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin Heidelberg New York, pp 542–548
Maizel J, Airapetian N, Lorne E, Tribouilloy C, Massy Z, Slama M (2007) Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med 33:1133–1138
Zogheib E, Defouilloy C, Mahjoub Y, Cherradi N, Moubarak M, Beloucif S, Dupont H (2007) Modification of hemodynamic effect after passive leg raising test by the use of elastic compression stocking (abstract). Intensive Care Med 33:S72
De Backer D (2006) Can passive leg raising be used to guide fluid administration? Crit Care 10:170
Lafanechere A, Pene F, Goulenok C, Delahaye A, Mallet V, Choukroun G, Chiche J, Mira J, Cariou A (2006) Changes in aortic blood flow induced by passive leg raising predict fluid responsiveness in critically ill patients. Crit Care 10:R132
Ridel C, Lamia B, Monnet X, Richard C, Teboul JL (2006) Passive leg raising and fluid responsiveness during spontaneous breathing: pulse contour evaluation. Intensive Care Med 32:S81
De Backer D, Pinsky MR (2007) Can one predict fluid responsiveness in spontaneously breathing patients? Intensive Care Med 33:1111–1113
Antonelli M, Levy M, Andrews PJ, Chastre J, Hudson LD, Manthous C, Meduri GU, Moreno RP, Putensen C, Stewart T, Torres A (2007) Hemodynamic monitoring in shock and implications for management. Intensive Care Med 33:575–590
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Monnet, X., Teboul, JL. Passive leg raising. Intensive Care Med 34, 659–663 (2008). https://doi.org/10.1007/s00134-008-0994-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-0994-y