Abstract
Objective
To evaluate the relationship between the HSV-1 and -2 loads in BAL fluid (BALF) and clinical outcome.
Design
Retrospective study.
Setting
The general intensive care unit of the University Hospital Maastricht.
Patients
Five hundred and twenty-one BALF samples from 462 patients were included. Patients were divided into three groups; (1) patients admitted to the hospital <48 h before lavage (Community), (2) patients admitted to the ICU >48 h before lavage (ICU) and (3) the remaining patients (non-ICU group).
Interventions
No additional interventions were conducted.
Measurements and results
HSV-1 and HSV-2 loads were determined by real-time polymerase chain reaction (PCR). HSV-1 DNA was detected in 4.3% (4/92) of samples in the community group, 15% (18/121) in the non-ICU group and in 32% (99/308) of the ICU group. In the age group <50 years HSV-1 DNA was less frequently isolated compared to the age group ≥50 years (16/129 (12%) versus 187/376 (25%), respectively, OR = 2.6; P < 0.001). HSV-1 loads of >105 genome equivalents (ge)/ml were associated with an increased 14-day in-hospital mortality compared to patients with a HSV-1 load ≤105 ge/ml in BALF (41 vs. 20%, respectively, P = 0.001). HSV-1 pneumonia was histologically proven in two patients with a HSV-1 load exceeding 105 ge/ml.
Conclusions
HSV-1 occurred more in critically ill patients and high loads in BALF were associated with an increased mortality. The higher mortality observed in patients with HSV-1 load >105 ge/ml enforces its clinical relevance and necessitates to start randomized medical intervention studies.
Similar content being viewed by others
Introduction
Human herpes simplex virus (HSV) belongs to the family of Herpesviridae and encompasses two subtypes, HSV-1 and HSV-2, both of which are highly prevalent and ubiquitously distributed [1, 2]. In the immunocompetent adult, host HSV infection usually has a benign course. As is the case with other herpesviruses, the initial infection is followed by a lifelong latent infection, from which reactivation can occur. Occasionally, HSV may cause pneumonia as a result of immunosuppression [3, 4], with a high mortality. In earlier reports, HSV was isolated from respiratory secretions from patients with adult respiratory distress syndrome, burns and in other non-immunosuppressed patients without a history of lung disease [5–7]. Interestingly, Schuller et al. [8] showed that immunocompetent patients from which HSV-1 was recovered from the respiratory tract showed severer illness and worse outcome compared to immunocompromised patients. Nevertheless, HSV can also be isolated from the respiratory tract of asymptomatic adults (up to 5%) [1]. Since this virus may severely affect pulmonary function in a wide range of patients and effective treatment with aciclovir is available, it is crucial to distinguish asymptomatic carrier ship of HSV from symptomatic infection. To investigate the presence of HSV in bronchoalveolar lavage fluid (BALF), we subjected a series of BALF samples to HSV-1 and HSV-2 specific quantitative, real-time PCR assays. Subsequently, the viral loads were correlated with clinical parameters and outcome.
Materials and methods
Patients included
This retrospective study was conducted at the University Hospital Maastricht from January 1999 until December 2004. All consecutive BALF samples obtained from critically ill ICU patients clinically suspected of ventilator-associated pneumonia (VAP) and all BALF samples from non-ICU patients (presented for viral culture) were included. In the ICU patients clinical evolution was assessed by means of sequential organ failure assessment (SOFA) score [9]. Patients were divided into three groups: (1) patients admitted to the hospital <48 h before lavage were classified as community; (2) patients admitted to the ICU and on mechanical ventilation >48 h before lavage as ICU and (3) the remaining patients were included in the non-ICU group.
Clinical variables
Clinical suspicion of VAP was defined as described by Bonten et al. [10]. Microbiologically confirmed VAP was defined as admission to the ICU >48 h prior to BAL collection, a total quantitative culture result of ≥104 cfu/ml and/or ≥2% infected cells (IC) [11, 12]. Mortality was measured as a dichotomous variable, death within 14 days after BAL-procedure (yes/no) in hospitalised patients.
Collected data included patients’ demographic characteristics such as age, gender and clinical data such as reason for performing BAL, diagnosis upon admittance, admittance to ICU ward, smoking, length of ICU stay before the performance of BAL, total length of stay at ICU, total length of hospital stay, mortality, diagnosis at post-mortem examination, antiviral therapy, diagnosis of pulmonary disease after BAL and laboratory data concerning BALF: total cell count, differential cell count presence of ciliated epithelial cells, squamous epithelial cells, reactive pneumocytes type II (RPII) [13] and quantitative culture results.
Sampling technique
Bronchoscopy with subsequent lavage was performed as previously described [14]. BALF samples were transported to the laboratory within 15 min after collection and processed immediately upon arrival at the microbiology laboratory.
Laboratory processing
The first fraction of BALF represents the bronchial fraction and was not used in this study. The remaining three fractions (alveolar fractions) were pooled. A total cell count was performed using a Fuchs Rosenthal haemocytometer chamber. Quantitative bacterial culture was performed as previously described [15]. Cytocentrifuged preparations [16] were made and stained with May-Grünwald Giemsa stain and Gram stain. Differential cell count [17] was performed including infected cells (IC) and RPII [13]. From each sample 6 ml was centrifuged (250 g, 10 min), dividing the sample into cells and supernatant. The supernatant was stored in tubes of 1 ml at −80°C. The cells were resuspended in 6 ml of a mixture of Eagle’s Minimal Essential Medium (EMEM) with 2% dimethyl sulfoxide (DMSO) and also stored in tubes of 1 ml at −80°C.
Virological assessment
A total of 500 μl of the stored cell fraction was used for DNA isolation using the Wizard® Genomic DNA Purification Kit (Promega, Madison, USA). Purified DNA was resuspended in a final volume of 120 μl. Each sample was spiked with a control plasmid (murine cytomegalovirus glycoprotein B gene (MCMV gB) [18] before DNA isolation as an isolation and amplification control. An in-house real-time PCR was performed using primers and probes which target the glycoprotein G-(gG) gene (HSV-1) and the glycoprotein D- (gD) gene (HSV-2) [19]. Assays (both HSV-1 and HSV-2) were performed in a 96-well Optical Reaction plate (Applied Biosystems, Foster City, California) in a total volume of 50 μl which contained 0.2 μM forward primer, 0.6 μM reverse primer, 0.075 μM probe, 1 × Taqman® Universal Master Mix (ABI) and 20 μl purified DNA. The PCR reactions for the internal control (MCMV gB) were carried out as described previously [18]. The PCR thermal profile consisted of an initial incubation of 2 min at 50°C, followed by activation of the AmpliTaq Gold® Polymerase during 10 min at 95°C. A total of 42 cycles of amplification were run consisting of 15 s at 95°C and 1 min at 60°C. Amplification was performed using the ABI PRISM 7000 Sequence Detection System (ABI) and data were interpreted using the ABI Prism software. Quantification was done by extrapolation of data to standardcurves generated by amplification of quantified dilutions of plasmids containing the HSV-1gG gene and HSV-2 gDgene.
Clinical chemistry
Urea was measured in BALF (as a marker of dilution) and in serum using a commercially available kit (Urea, Beckman Coulter, Fullerton, California, USA).
Statistical analysis
To compare the quantitative real-time PCR results between recovered BALF samples, the quantity was converted to those present in the epithelial lining fluid (ELF) using the formula described by Wiedermann et al. [20], which is based upon urea concentrations in BALF and in serum:
Geometrical mean viral loads were calculated as log 10 of HSV-positive BALF samples. Groups were compared by t test statistics and Chi-square statistics where appropriate. Risk factors for HSV-1 shedding (yes/no) were identified by univariate logistic regression analysis (Table 1). Clinical outcome measures were defined as in-hospital death within 14 days, presence of pneumonia and/or and presence of HSV-pneumonitis at post-mortem examination. Furthermore, we used Kaplan–Meier method for computing the probability of survival in both groups up to day 30 after BAL. A log rank test (Mantel-Cox) was performed and no cases were censored.
Results
Patient population
During the study period 1,033 BALF samples (from 866 patients) were eligible for inclusion in our study. This included 456 samples retrieved from ICU patients and 577 samples retrieved from non-ICU patients. Insufficient material for PCR was available for 148 and 55 BALF samples respectively, therefore these patients were excluded. Viral culture was requested on 132 out of the 522 (25%) samples from non-ICU patients. Figure 1 shows an overview of the included patients. Out of the 89 community patients, 19 were eventually admitted to the ICU (3 immediately after BAL), out of the 113 non-ICU patients 6 were eventually admitted to the ICU. None of the patients were treated with aciclovir. Reason for performing BAL included: ICU group, suspicion of VAP; non-ICU patients, suspicion of pneumonia; community group, suspicion of sarcoidosis (n = 10), suspicion of infection (n = 50) and as a diagnostic work-up of an interstitial pulmonary disease (n = 32).
Table 1 shows the demographic and clinical characteristics of the three groups. Table 2 shows the demographic and clinical characteristics of patients with and without HSV in BALF.
Factors associated with HSV-1 shedding in BALF
Among the patient and clinical variables only age over 50 years BALF and admittance to the ICU were significantly associated with HSV-1 in BALF (Table 2). None of the cytological parameters of BALF were associated with the presence of HSV-1 in BALF (data not shown). Multivariate analysis showed that hospital admittance and age over 50 years were independent associated with the presence of HSV-1 in BALF with odds ratios of 3.7 [95% confidence interval (CI 1.2–11) for the non-ICU, 9.6 (95%CI 3.4–27) for the ICU and 2.6 (95%CI 1.5–4.6) for age over 50.
Quantitative PCR results
The HSV-1 PCR positive BALF samples were divided into logarithmic categories based upon quantitative PCR results (10 ge/ml = log 1, 100 ge/ml = log 2 and so forth). Figure 2 shows the number of BALF samples with HSV-1 divided into logarithmic categories. All patients in the community group had a viral load in BALF of 104 ge/ml or less. Among the ICU and non-ICU group 36% (36/99) and 28% (5/18) had a BALF viral load ≥105 ge/ml, respectively. In one patient, BAL was performed twice within a period of 5 days, both BALF samples showed the presence of HSV-1 with increasing quantities (105 and 107 ge/ml). The patient died 4 days after the second BAL. Post-mortem examination revealed an extended pneumonia caused by HSV-1.
Distribution of quantitative HSV-1 loads in BALF. Each bar is divided into ICU, non-ICU and community patients. The y axis represents the number of samples, whereas the x axis represents the HSV-1 load in logarithmic categories. BALF Bronchoalveolar lavage fluid, ICU intensive care unit, HSV-1 herpes simplex virus type 1, PCR polymerase chain reaction, ge/ml genome equivalents per millilitre
Establishing a clinical relevant cut-off value for HSV-1 viral load for ICU patients
To assess a clinical relevant cut-off value for the HSV-1 viral load, the in-hospital mortality within 14 days after collection of BALF was selected as relevant clinical parameter. For this analysis we included only ICU patients. At each possible cut-off value, the in-hospital mortality was compared to the in-hospital mortality of patients with a non-reactive HSV-1 PCR. Up to the cut-off value of 105 ge/ml HSV-1 in BALF, the group above the cut-off value showed a significant higher mortality. At higher cut-off values there were no significant differences between the groups. Therefore, the cut-off value for HSV-1 load in BALF was set at 105 ge/ml. This resulted in an in-hospital death within 14 days of 20% below compared to 41% above the cut-off value. Survival at day 30 after BAL in the group below and above the cut-off value was, respectively, 37.4 and 11.1% (Log rank test; χ2 = 13.83, P < 0.001) (Fig. 3).
Survival curve for the ICU patients. The y axis shows the percentage of patients surviving, the x axis represents the days after lavage. Patients are divided into two groups, patients with HSV-1 viral load in BALF < 105 ge/ml and patients with HSV-1 viral load ≥105 ge/ml (represented by the dotted line). BALF Bronchoalveolar lavage fluid, ICU intensive care unit, HSV-1 herpes simplex virus type 1, ge/ml genome equivalents per millilitre
The mean duration of survival after lavage was 80 days (95%CI 61–97) in the group with a HSV-1 viral load <105 ge/ml, compared to 13 days (95%CI 5–21) in the group with a HSV-1 viral load ≥105 ge/ml.
Post-mortem examination results
Out of the 152 (152/462, 33%) patients who died during hospitalisation, 98 died within 14 days after BAL (community: 6, non-ICU: 11 and ICU: 81). Out of these 98 patients, 84 showed a HSV-1 load ≤105 ge/ml and 14 patients showed a HSV-1 load exceeding 105 ge/ml. In 37 patients, post-mortem examination was performed (community: 4, non-ICU: 5, ICU: 28). In the group patients with a HSV-1 load ≤105 ge/ml 32 (32/84, 38%) post-mortem examinations were performed. In 70% (26/37) of these patients, pneumonia was determined the cause of death. Out of the 14 patients with >105 ge/ml, post-mortem examination was available for five (5/14, 36%). All five post-mortem examination reports stated pneumonia as the cause of death, including two patients (2/5, 40%) diagnosed with HSV-1 associated pneumonia, showing the presence of specific herpetic nuclear inclusions in the lungs at post-mortem examination which stained positive in the HSV-1 immunofluorescent stain. In the group of patients with a HSV-1 load in BALF ≤105 ge/ml this diagnosis was never attributed.
Concomitant presence of VAP
Out of the 308 episodes of suspected VAP in 260 patients, 135 episodes (44%) in 125 patients were microbiologically confirmed VAP (Table 3). The causative organisms were Pseudomonas aeruginosa (n = 37), Staphylococcus aureus (n = 27), Enterobacteriaceae (n = 38), Haemophilus influenzae (n = 4), Streptococcus pneumoniae (n = 3) and others (e.g. Stenotrophomonas maltophilia, Moraxella catarrhalis, n = 26). In 44 (33%) episodes of VAP, the quantitative PCR for HSV-1 was positive. In 13 (10%) cases the HSV-1 load in BALF exceeded 105 ge/ml. There were no significant differences in type of bacteria causing VAP between the HSV-1 positive- and negative group.
Results of HSV-2 detection in BALF
HSV-2 was detected in only 2 out of 521 examined BALF with low viral loads. Both BALF samples were from non-ICU patients admitted to the department of internal medicine (Fig. 2). One patient was diagnosed with Morbus Wegener, the other with a bacterial pneumonia. In neither of the patients the recovery of HSV-2 was associated with morbidity or mortality.
Discussion
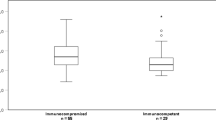
In this study, HSV-1 DNA was detected in 32% of BALF samples from ICU patients compared to 4.3% BALF obtained from community patients and 15% obtained from non-ICU patients. From the clinical and demographic variables we studied, only age above 50 years and admittance to the ICU appeared to be independent predictive factors for HSV-1 shedding. A significantly higher 14-day in-hospital mortality was observed in ICU patients with HSV-1 loads >105 ge/ml compared to ICU patients with HSV-1 loads ≤105 ge/ml in BALF, 41 versus 20%, respectively. HSV-1 viral loads in BALF exceeding 105 ge/ml reflected serious disease and was associated with an increased mortality rate of 21% in critically ill patients in this study.
Infections of the lung caused by HSV are considered to be extremely rare except in severely immunosuppressed patients [21, 22]. However, animal models, case reports and pilot studies showed that a HSV-1 pneumonia is not exclusively linked to a state of immunosuppression [4, 23, 24]. Moreover, two recent reports, with a large number of patients included, detected HSV-1 in ICU patients that were not considered to be primarily immunocompromised [25, 26]. In both studies, a significant adverse effect of HSV-1 shedding in the respiratory tract on clinical outcome was established. To be able to determine a relevant cut-off value for the presence of HSV-1 and -2 loads in BALF, we applied a quantitative real-time PCR. Overall detection rate in samples obtained from the hospital population (ICU and non-ICU group combined) was 27%. The detection rate found in this study is similar to the 27% that has been reported by Ong et al. using BAL and PCR in ICU patients [26]. Bruynseels et al. found a lower prevalence (16%), however they used viral culture instead of the more sensitive PCR technique to detect HSV [25]. A third study showed a much higher prevalence of up to 64% [27], probably because their study population consisted only of severely ill ICU patients who were on ventilation for more than 5 days. In our study group, an overall mortality of 35% was observed. The 14 day in-hospital mortality in patients with a HSV-1 load in BALF ≤105 ge/ml was 20% compared to 41% in patients with a load >105 ge/ml. Thus, a HSV-1 viral load of >105 ge/ml was associated with 21% increase in mortality. A recent study by Luyt et al. [27] showed the patients they classified as having bronchopneumonitis had BALF viral loads of 102 to 108 copies/106 cells present in BALF. In this study, only ICU patients with prolonged ventilation (>5 days) were included. They classified their patients as having bronchopneumonitis by clinical suspicion of lower respiratory tract infection associated with the presence of HSV-1 in the lower respiratory tract and specific herpetic inclusions in BAL or bronchial biopsies. Using the HSV-1 viral load in BALF to predict the presence of HSV-1 bronchopneumonitis led to a sensitivity of 81% and a specificity of 83% at a cut-off value of 104 copies/106 cells present in BALF. The fact that they found a lower cut-off value may be due to the fact that they normalised the HSV-1 load in BALF by the number of cells in BALF, whilst we used the dilution factor of BALF compared to ELF. Since the number of cells present in BALF increases due to inflammation [28] and the total cell count of BALF depends upon technical variables [29], the number of HSV copies per cells present in BALF may not be the most objective way of representing the HSV load in BALF.
In a recent study, it was concluded that HSV-1 has a low pulmonary pathogenicity [30]. This notion was based on a normal capillary permeability measured in the lungs of only four critically ill patients without quantifying HSV-1 in the respiratory tract. Although the study was not designed to prove HSV-1 to be the absolute cause of mortality, in at least two of the four patients with a HSV-1 in BALF of >105 ge/ml, HSV-1 pneumonia was determined as the cause of death at post-mortem examination. These results indicate that HSV-1 could play a causative role in the development of respiratory pathology, as was previously described for immunocompromised patients [5, 31, 32]. Apart from the more general causes of immunosuppression, such as immunosuppressive therapy, it has been shown that major surgery, trauma and excessive blood loss may also cause a dramatic decrease in cell-mediated immunity and hence induce the reactivation of HSV-1.
Besides the presence of HSV-1 in BALF, we also determined the presence of HSV-2. In only two out of 521 BALF samples HSV-2 was recovered, with relatively low loads of 253 and 104 ge/ml. This finding corresponds with the notion that HSV-1 infections in our population are generally restricted to the oropharynx, whereas HSV-2 infections are usually limited to the genital mucosa.
Although this study shows an increase in mortality in patients with a HSV-1 load in BALF exceeding 105 ge/ml, the design of this study was insufficient to prove HSV-1 to be the cause of death in all but 2 patients. Due to the retrospective nature of the study it was not possible to measure an intervention (admittance of aciclovir) and clinical outcome. A large prospective, randomized medical intervention study in a wide range of critically ill patients is needed. Using the proposed cut-off level of 105 ge/ml HSV-1 in BALF patients this may provide the opportunity to ultimately unravel the role of HSV-1 in pulmonary disease.
In conclusion, HSV-1 was present in approximately one-third of all BALF samples acquired from ICU patients. Furthermore, our results indicated that a HSV-1 load in BALF of >105 ge/ml is an independent predictor for a poor outcome in critically ill patients, with an increase in mortality rate of 21%. It remains to be determined whether HSV-1 is causally linked with a low survival or whether it is a marker of a severely disturbed immune system. Until additional data of a large prospective, randomised intervention study are available, the administration of aciclovir in ICU patients with a HSV-1 load in BALF exceeding 105 ge/ml should be considered.
References
Cleator GM, Klapper PE (2005) Principles and practice of clinical virology. Wiley, London
Whitley RJ, Roizman B (2001) Herpes simplex virus infections. Lancet 357:1513–1518
Byers RJ, Hasleton PS, Quigley A, Dennett C, Klapper PE, Cleator GM, Faragher EB (1996) Pulmonary herpes simplex in burns patients. Eur Respir J 9:2313–2317
Arata K, Sakata R, Iguro Y, Toda R, Watanabe S, Eitsuru Y (2003) Herpes simplex viral pneumonia after coronary artery bypass grafting. Jpn J Thorac Cardiovasc Surg 51:158–159
Wallace JM (1989) Pulmonary infection in human immunodeficiency disease: viral pulmonary infections. Semin Respir Infect 4:147–154
James E, Robinson L, Griffiths PD, Prentice HG (1996) Acute myeloblastic leukaemia presenting with herpes simplex type-1 viraemia and pneumonia. Br J Haematol 93:401–402
Prellner T, Flamholc L, Haidl S, Lindholm K, Widell A (1992) Herpes simplex virus—the most frequently isolated pathogen in the lungs of patients with severe respiratory distress. Scand J Infect Dis 24:283–292
Schuller D (1994) Lower respiratory tract reactivation of herpes simplex virus. Comparison of immunocompromised and immunocompetent hosts. Chest 106:3S–7S discussion 34S–35S
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Bonten MJ, Bergmans DC, Stobberingh EE, van der Geest S, De Leeuw PW, van Tiel FH, Gaillard CA (1997) Implementation of bronchoscopic techniques in the diagnosis of ventilator-associated pneumonia to reduce antibiotic use. Am J Respir Crit Care Med 156:1820–1824
Baselski V (1993) Microbiologic diagnosis of ventilator-associated pneumonia. Infect Dis Clin North Am 7:331–357
Allaouchiche B, Jaumain H, Dumontet C, Motin J (1996) Early diagnosis of ventilator-associated pneumonia. Is it possible to define a cutoff value of infected cells in BAL fluid? Chest 110:1558–1565
Linssen KC, Jacobs JA, Poletti VE, van Mook W, Cornelissen EI, Drent M (2004) Reactive type II pneumocytes in bronchoalveolar lavage fluid. Acta Cytol 48:497–504
Linssen CF, Jacobs JA, Schouten JS, van Mook WN, Ramsay G, Drent M (2008) Influence of antibiotic therapy on the cytological diagnosis of ventilator-associated pneumonia. Intensive Care Med 34:865–872
Jacobs JA, De Brauwer EI, Cornelissen EI, Drent M (2000) Accuracy and precision of quantitative calibrated loops in transfer of bronchoalveolar lavage fluid. J Clin Microbiol 38:2117–2121
De Brauwer EI, Jacobs JA, Nieman F, Bruggeman CA, Wagenaar SS, Drent M (2000) Cytocentrifugation conditions affecting the differential cell count in bronchoalveolar lavage fluid. Anal Quant Cytol Histol 22:416–422
De Brauwer EI, Jacobs JA, Nieman F, Bruggeman CA, Drent M (2002) Bronchoalveolar lavage fluid differential cell count. How many cells should be counted? Anal Quant Cytol Histol 24:337–341
Vliegen I, Duijvestijn A, Stassen F, Bruggeman C (2004) Murine cytomegalovirus infection directs macrophage differentiation into a pro-inflammatory immune phenotype: implications for atherogenesis. Microbes Infect 6:1056–1062
van Doornum GJ, Guldemeester J, Osterhaus AD, Niesters HG (2003) Diagnosing herpesvirus infections by real-time amplification and rapid culture. J Clin Microbiol 41:576–580
Wiedermann FJ, Mayr AJ, Kaneider NC, Fuchs D, Mutz NJ, Schobersberger W (2004) Alveolar granulocyte colony-stimulating factor and alpha-chemokines in relation to serum levels, pulmonary neutrophilia, and severity of lung injury in ARDS. Chest 125:212–219
Tang IT, Shepp DH (1992) Herpes simplex virus infection in cancer patients: prevention and treatment. Oncology (Williston Park) 6:101–106, 109; discussion 109–110
Nichols WG, Boeckh M, Carter RA, Wald A, Corey L (2003) Transferred herpes simplex virus immunity after stem-cell transplantation: clinical implications. J Infect Dis 187:801–808
Miyazato A, Kishimoto H, Tamaki K, Nakama K, Saito A (2001) Herpes simplex virus bronchopneumonia in a non-immunocompromized individual. Intern Med 40:836–840
Cherr GS, Meredith JW, Chang M (2000) Herpes simplex virus pneumonia in trauma patients. J Trauma 49:547–549
Bruynseels P, Jorens PG, Demey HE, Goossens H, Pattyn SR, Elseviers MM, Weyler J, Bossaert LL, Mentens Y, Ieven M (2003) Herpes simplex virus in the respiratory tract of critical care patients: a prospective study. Lancet 362:1536–1541
Ong GM, Lowry K, Mahajan S, Wyatt DE, Simpson C, O’Neill HJ, McCaughey C, Coyle PV (2004) Herpes simplex type 1 shedding is associated with reduced hospital survival in patients receiving assisted ventilation in a tertiary referral intensive care unit. J Med Virol 72:121–125
Luyt CE, Combes A, Deback CA, Aubriot-Lorton MH, Nieszkowska A, Trouillet JL, Capron F, Agut H, Gilbert G, Chastre J (2007) Herpes simples cirus lung infection in patients undergoing prolonged mechanical ventilation. Am J Respir Crit Care Med 175:935–942
Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM (1991) Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis 143:1121–1129
Timsit JF, Misset B, Goldstein FW, Vaury P, Carlet J (1995) Reappraisal of distal diagnostic testing in the diagnosis of ICU-acquired pneumonia. Chest 108:1632–1639
Verheij J, Groeneveld AB, Beishuizen A, van Lingen A, Simoons-Smit AM, van Schijndel RJ (2004) Herpes simplex virus type 1 and normal protein permeability in the lungs of critically ill patients: a case for low pathogenicity? Crit Care 8:R139
Graham BS, Snell JD Jr (1983) Herpes simplex virus infection of the adult lower respiratory tract. Medicine (Baltimore) 62:384–393
Kim E, Lee K, Primack S, Yoon H, Byun H, Kim TS, Suh OJ, Han J (2002) Viral pneumonias in adults: radiologic and pathologic findings. Radiographics 22:S137–S149
Author information
Authors and Affiliations
Corresponding author
Additional information
The abstract of this article was published in ESCV/SGM Conference, Birmingham, as an oral presentation.
Rights and permissions
About this article
Cite this article
Linssen, C.F.M., Jacobs, J.A., Stelma, F.F. et al. Herpes simplex virus load in bronchoalveolar lavage fluid is related to poor outcome in critically ill patients. Intensive Care Med 34, 2202–2209 (2008). https://doi.org/10.1007/s00134-008-1231-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1231-4