Abstract
Purpose
Non-invasive positive pressure ventilation (NIV) is being increasingly used in paediatric critical care, although its use in acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) is still debated. No definite data are available for the prediction of NIV outcome in such selected populations. We aimed to identify which factors might affect NIV failure in paediatric ALI/ARDS patients.
Methods
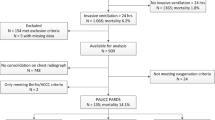
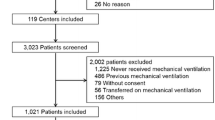
A retrospective cohort study using comprehensive predictivity analysis was performed. All children admitted to our paediatric intensive care unit over a 4-year period for ALI/ARDS were reviewed. Basic, clinical, physiological parameters and their change after 1 h of NIV were considered and subjected to univariate analysis. Candidate prognostic variables were then subjected to multicollinearity scrutiny and logistic regression. Finally, variables significant in the logistic regression were subjected to predictivity analysis.
Results
The number of organ failures at admission (NOF) is a strong predictor of NIV failure (odds ratio 5.26; p = 0.004). Having only one organ failure provides a probability of NIV success of 85.7% (sensitivity 87%; specificity 49%). One NIV failure will be predicted and avoided for every four cases in which the presence of other organ failures is incorporated into the clinical decision.
Conclusions
NOF significantly predicts the NIV failure. Children with no organ failures other than ALI/ARDS may safely be treated with NIV.

Similar content being viewed by others
References
Essouri S, Chevret L, Durand P, Haas V, Faroux B, Devictor D (2006) Noninvasive positive pressure ventilation: five years of experience in a pediatric intensive care unit. Pediatr Crit Care Med 7:329–334
Yanez LJ, Yunge M, Emilfork M, Lapadula M, Alcantara A, Fernandez C, Lozano J, Contreras M, Conto L, Arevalo C, Gayan A, Hernandez RN, Pedraza M, Feddersen M, Bejares M, Morales M, Mallea F, Glasinovic M, Cavada G (2008) A prospective, randomized, controlled trial of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 9:484–489
Mayordomo-Colunga J, Medina A, Rey C, Concha A, Menendez S, Los Arcos M, Garcia I (2010) Noninvasive ventilation after extubation in paediatric patients: a preliminary study. BMC Pediatrics 10:29
Piastra M, Antonelli M, Caresta E, Chiaretti A, Polidori G, Conti G (2006) Noninvasive ventilation in childhood acute neuromuscular respiratory failure: a pilot study. Respiration 73:791–798
Thill PJ, McGuire JK, Baden HP, Green TP, Checchia PA (2004) Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediatr Crit Care Med 5:337–342
Piastra M, Antonelli M, Chiaretti A, Polidori G, Polidori L, Conti G (2004) Treatment of acute respiratory failure by helmet-delivered noninvasive pressure support ventilation in children with acute leukemia: a pilot study. Intensive Care Med 30:472–476
Chin K, Takahashi K, Ohmori K, Toru I, Matsumoto H, Niimi A, Doi H, Ikeda T, Nakahata T, Komeda M, Mishima M (2007) Noninvasive ventilation for pediatric patients under 1 year of age after cardiac surgery. J Thorac Cardiovasc Surg 134:260–261
Antonelli M, Conti G, Bufi M, Costa MG, Lappa A, Rocco M, Gasparetto A, Meduri GU (2000) Noninvasive ventilation for the treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA 283:235–241
Antonelli M, Conti G, Rocco M, Bufi M, De Blasi RA, Vivino G, Gasparetto A, Meduri GU (1998) A comparison of noninvasive positive pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med 339:429–435
Nava S, Hill N (2009) Noninvasive ventilation in acute respiratory failure. Lancet 374:250–259
Bernet V, Hug MI, Frey B (2005) Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med 6:660–664
Mayordomo-Colunga J, Medina A, Rey C, Diaz JJ, Concha A, Los Arcos M, Menendez S (2009) Predictive factors of noninvasive ventilation failure in critically ill children: a prospective epidemiological study. Intensive Care Med 35:527–536
Munoz-Bonet JI, Flor-Macian EM, Brines J, Rossellò-Millet PM, Llopis MC, Lòpez-Pratz JL, Castillo S (2010) Predictive factors for the outcome of noninvasive ventilation in pediatric acute respiratory failure. Pediatr Crit Care Med 11:675–680
Piastra M, De Luca D, Pietrini D, Pulitanò S, D’Arrigo S, Mancino A, Conti G (2009) Noninvasive pressure-support ventilation in immunocompromised children with ARDS: a feasibility study. Intensive Care Med 35:1420–1427
Demoule A, Girou E, Richard JC, Taille S, Brochard L (2006) Benefits and risks of success or failure of non invasive ventilation. Intensive Care Med 32:1756–1765
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Rocco M, Dell’Utri D, Morelli A, Spadetta G, Conti G, Antonelli M, Pietropaoli P (2004) Noninvasive ventilation by helmet or face mask in immunocompromised patients: a case–control study. Chest 126:1508–1515
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM-III: an updated pediatric risk of mortality score. Crit Care Med 24:743–752
Goldstein B, Giroir B, Randolph A, The members of the international consensus conference on pediatric sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2–8
Norusis M (2004) SPSS 130 advanced statistical procedures companion. Prentice Hall, Upper Saddle River
Allison PD (1999) Logistic regression using the SAS system. SAS Institute, Cary
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Lacroix J, Cotting J, Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (2005) Severity of illness and organ dysfunction scoring in children. Pediatr Crit Care Med 6:S126–S134
Nichols DG, Walker LK, Wingard JR, Bender KS, Bezman M, Zahurak ML, Piantadosi S, Frey-Simon M, Rogers MC (1994) Predictors of acute respiratory failure after bone marrow transplantation in children. Crit Care Med 22:1485–1491
Shah PS, Ohlsson A, Shah JP (2008) Continuous negative extrathoracic pressure or continuous positive airway pressure for acute hypoxemic respiratory failure in children. Cochrane Database Syst Rev 1:CD003699
Randolph AG (2009) Management of acute lung injury and acute respiratory distress syndrome in children. Crit Care Med 37:2448–2454
Conflict of interest
Authors have neither funding nor conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Piastra, M., De Luca, D., Marzano, L. et al. The number of failing organs predicts non-invasive ventilation failure in children with ALI/ARDS. Intensive Care Med 37, 1510–1516 (2011). https://doi.org/10.1007/s00134-011-2308-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2308-z