Abstract
Summary
This analysis was conducted to assess the effect of high versus lower doses of ibandronate on nonvertebral fractures. The results were adjusted for clinical fracture, age, and bone density. The treatment effect was dose-dependent. Higher doses of ibandronate significantly reduced the risk of nonvertebral fractures more effectively compared with lower doses.
Introduction
The objective of this study was to assess the efficacy of different doses of ibandronate on nonvertebral fractures in a pooled analysis.
Methods
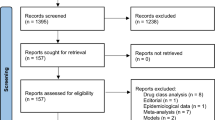
Eight randomized trials of ibandronate were reviewed for inclusion. Alternative definitions of high versus low doses based on annual cumulative exposure (ACE) were explored. A time-to-event analysis was conducted using Kaplan–Meier methodology. Hazard ratios (HR) were derived using Cox regression and adjusted for covariates.
Results
Combining higher ACE doses of ≥ 10.8 mg (150 mg once monthly, 3 mg i.v. quarterly, and 2 mg i.v. every 2 months) versus ACE doses of 5.5 mg, from two trials, resulted in an HR 0.62 (95% CI 0.396–0.974, p = 0.038). There was a dose–response trend with increasing ACE doses (7.2–12 mg) versus ACE of 5.5 mg.
Conclusions
A dose–response effect on nonvertebral fractures was observed when comparing high with low ACE doses. A significant reduction in nonvertebral fractures was noted when pooling data from trials using ACE doses of ≥ 10.8 mg versus ACE ≤ 7.2 mg; and with ACE ≥ 10.8 mg versus ACE of 5.5 mg (38% reduction). Higher ibandronate dose levels (150 mg monthly or 3 mg i.v. quarterly) significantly reduced nonvertebral fracture risk in postmenopausal women.

Similar content being viewed by others
References
Chesnut CH III, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A et al (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 8:1241–1249
Recker R, Stakkestad JA, Chesnut CH III, Christiansen C, Skag A, Hoiseth A et al (2004) Insufficiently dosed intravenous ibandronate injections are associated with suboptimal antifracture efficacy in postmenopausal osteoporosis. Bone 34(5):890–899
Miller PD, McClung MR, Macovei L, Stakkestad JA, Luckey M, Bonvoisin B et al (2005) Monthly oral ibandronate therapy in postmenopausal osteoporosis: 1-year results from the MOBILE study. J Bone Miner Res 20(8):1315–1322
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D et al (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54(6):1838–1846
Ravn P, Neugebauer G, Christiansen C (2002) Association between pharmacokinetics of oral ibandronate and clinical response in bone mass and bone turnover in women with postmenopausal osteoporosis. Bone 30(1):320–324
Adami S, Felsenberg D, Christiansen C, Robinson J, Lorenc RS, Mahoney P et al (2004) Efficacy and safety of ibandronate given by intravenous injection once every 3 months. Bone 34(5):881–889
Riis BJ, Ise J, von Stein T, Bagger Y, Christiansen C (2001) Ibandronate: a comparison of oral daily dosing versus intermittent dosing in postmenopausal osteoporosis. J Bone Miner Res 16(10):1871–1878
Thiebaud D, Burckhardt P, Kriegbaum H, Huss H, Mulder H, Juttmann JR et al (1997) Three monthly intravenous injections of ibandronate in the treatment of postmenopausal osteoporosis. Am J Med 103(4):298–307
Delmas PD, Recker RR, Chesnut CH III, Skag A, Stakkestad JA, Emkey R et al (2004) Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int 15(10):792–798
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL et al (2006) Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis 65(5):654–661
Barrett J, Worth E, Bauss F, Epstein S (2004) Ibandronate: a clinical pharmacological and pharmacokinetic update. J Clin Pharm 44(9):951–965
Cremers SC, Pillai G, Papapoulos SE (2005) Pharmacokinetics/pharmacodynamics of bisphosphonates: use for optimization of intermittent therapy for osteoporosis. Clin Pharmacokinet 44(6):551–570
Papapoulos SE, Schimmer RC (2007) Changes in bone remodelling and antifracture efficacy of intermittent bisphosphonate therapy: implications from clinical studies with ibandronate. Ann Rheum Dis 66(7):853–858
Harrington JT, Ste-Marie LG, Brandi ML, Civitelli R, Fardellone P, Grauer A et al (2004) Risedronate rapidly reduces the risk for nonvertebral fractures in women with postmenopausal osteoporosis. Calcif Tissue Int 74(2):129–135
Papapoulos SE, Quandt SA, Liberman UA, Hochberg MC, Thompson DE (2005) Meta-analysis of the efficacy of alendronate for the prevention of hip fractures in postmenopausal women. Osteoporos Int 16(5):468–474
Acknowledgements
Funding for this project was from an unrestricted research grant from F. Hoffman-La Roche. The authors would like to thank Hoffman La Roche and GlaxoSmithKline for supplying the individual patient data utilized in the analysis, and acknowledge that the analysis was completed without influence from either company. A. Cranney (AC) would like to acknowledge salary support from the Canadian Institutes of Health Research.
Conflicts of interest
Ethel S. Siris: consultant for Wyeth, Procter & Gamble/sanofi-aventis, Novartis, Eli Lilly, Roche/GlaxoSmithKline, Amgen; speaker for Eli Lilly, Procter & Gamble/Sanofi-aventis, Novartis.
Stuart L. Silverman: speaker’s bureau for Eli Lilly, Merck, Procter & Gamble, Roche; consultant for Merck, Procter & Gamble, Wyeth, Roche, Novartis; research support: Novartis, Eli Lilly, Wyeth, Roche, Procter & Gamble, Merck; board of directors, Compumed
Philip Sambrook: consultant/speaker: for Amgen, GSK, Merck, Novartis, sanofi-aventis, Servier; clinical trials for Amgen, Servier, GSK, Merck, Novartis
Jean-Yves Reginster: consulting fees or paid advisory boards, Servier, Novartis, Negma, Eli Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, Theramex; lecture fees when speaking from Merck Sharp and Dohme, Eli Lilly, Rottapharm, IBSA, Genevrier, Novartis, Servier, Roche, GlaxoSmithKline, Teijin, Teva, Ebewee Pharma, Zodiac, Analis, Theramex, Nycomed, Novo-Nordisk; grant support from Bristol Myers Squibb, Merck Sharp & Dohme, Rottapharm, Teva, Eli Lilly, Novartis, Roche, GlaxoSmithKline, Amgen, Servier
Socrates Papapoulos: consulting fees from Amgen, Eli Lilly, Merck & Co, Novartis, Procter & Gamble, Roche/GSK, Servier; research grant support from Merck Sharp & Dohme, Procter & Gamble
Pierre D. Delmas: research grants from Procter & Gamble, Eli Lilly, Amgen; consultation for and/or speaker fees from: Acceleron, Amgen, Eli Lilly, GSK, MSD, Novartis, Nycomed, Organon, Pfizer, Procter & Gamble, Roche, Sanofi-Aventis, Servier, Wyeth, Zelos
Jonathan D. Adachi: consultant/speaker: for Amgen, Astra Zeneca, Eli Lilly, GSK, Merck, Novartis, Pfizer, Procter & Gamble, Roche, Sanofi-Aventis, Servier; clinical trials for Amgen, Eli Lilly, GSK, Merck, Novartis, Pfizer, Procter & Gamble, Roche
A. Cranney: consultant fees from Amgen, Merck Frosst, Procter & Gamble
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cranney, A., Wells, G.A., Yetisir, E. et al. Ibandronate for the prevention of nonvertebral fractures: a pooled analysis of individual patient data. Osteoporos Int 20, 291–297 (2009). https://doi.org/10.1007/s00198-008-0653-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0653-8