Abstract
Introduction
Wrist fracture causes pain and decreased physical, social and emotional function. The International Osteoporosis Foundation has developed a specific questionnaire to assess quality of life in patients with wrist fracture. This questionnaire, including 12 questions, was validated in a multicentre study and compared with an osteoporosis-specific questionnaire (Qualeffo-41) and a generic questionnaire (EQ-5D).
Methods
The study included 105 patients with a recent wrist fracture and 74 sex- and age-matched control subjects. The questionnaire was administered as soon as possible after the fracture, at 6 weeks, 3 months, 6 months and 1 year after the fracture. Test–retest reproducibility, internal consistency and sensitivity to change were assessed.
Results and discussion
The results showed adequate repeatability and internal consistency of the International Osteoporosis Foundation (IOF) wrist fracture questionnaire. The discriminatory capacity between patients and control subjects was very high, with significant odds ratios for each question and domain. The IOF-wrist fracture questionnaire domain scores showed significant improvement after 3 and 6 months and some improvement from 6 months up to 1 year. The sensitivity to change was much higher for the IOF-wrist fracture total score than for Qualeffo-41 and EQ-5D.
Conclusion
In conclusion, the IOF-wrist fracture questionnaire appears to be a reliable and responsive quality of life questionnaire.
Similar content being viewed by others
Introduction
Wrist fracture or distal forearm fracture is one of the major osteoporotic fractures [1]. It causes pain and acute loss of physical function and has an impact on social and emotional function [2, 3]. Algodystrophy or complex regional pain syndrome is a debilitating consequence occurring in between 1% and 20 % of patients with distal forearm fracture [4]. Wrist fracture occurs early in the course of osteoporosis, and many patients are still employed. The socioeconomic impact of this fracture therefore is considerable. A wrist fracture often is a predictor of other fractures.
Osteoporotic fractures, such as vertebral and hip fractures, cause a considerable loss of quality of life, both acute loss, immediately after the fracture, and chronic loss because of recurrent fractures and disability due to incomplete recovery [5–9]. Several instruments have been developed for the assessment of quality of life after vertebral fractures. The European Foundation for Osteoporosis, now merged with the International Osteoporosis Foundation, developed a specific questionnaire for quality of life in patients with vertebral fractures. This questionnaire Qualeffo-41 (spine) has been validated and translated into many languages ([10], www.osteofound.org). It showed that quality of life decreased with increasing number of vertebral fractures and that lumbar fractures had more impact on quality of life than thoracic fractures [11]. A shorter version has also been developed [12].
The loss of quality of life after wrist fracture has been assessed with a generic quality of life questionnaire, the EQ-5D, showing a gradual improvement up until 1 year after the fracture [13]. The Working Group for Quality of Life of the International Osteoporosis Foundation has developed a questionnaire for quality of life specific for patients with wrist fracture. This questionnaire can be used as a supplement to the Qualeffo-41. The aim of the study was to test the validity of the International Osteoporosis Foundation (IOF) quality of life questionnaire for wrist fracture and to compare it with other quality of life questionnaires.
Subjects and methods
Development of the IOF-wrist fracture questionnaire
A focus group meeting was held with patients who had suffered a wrist fracture about 1 year ago. The discussion in this group included immediate consequences of the fracture such as pain and upper limb symptoms and more general problems such as physical function and general health, resulting in the identification of items for the questionnaire. The IOF Working Group on Quality of Life designed 12 questions, each with five answers in a Likert scale. The IOF-wrist fracture questionnaire was designed as a supplement to Qualeffo-41. Items on dressing and housekeeping were not included, nor emotional and mental impact of the fracture, because these are covered by Qualeffo-41. The questionnaire was developed in English and translations were made into Czech, Italian and Dutch according to a standard procedure developed for Qualeffo-41 [10]. In short, the translation was made by a native speaker and member of the Working Group, followed by a back-translation into English by an official interpreter. Subsequently, the translation was confronted with the original English version and adjusted as appropriate. The IOF-wrist fracture questionnaire is presented in the Appendix.
Study design
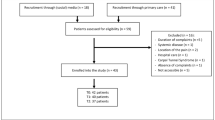
The study was designed as a prospective multicentre study in patients with a recent wrist fracture and age- and sex-matched control subjects with follow-up until 1 year after the fracture. The following questions were addressed: (1) What is the repeatability (test–retest reproducibility) of the IOF-wrist questionnaire? (2) What is the internal consistency of the IOF-wrist questionnaire compared with domains of Qualeffo-41? (3) Is the IOF-wrist questionnaire more sensitive to change following wrist fracture than Qualeffo-41 (spine) and the EQ-5D? The study was performed in five centres: Milan, Cambridge, Leuven, Ghent and Amsterdam. The protocol was approved by the Ethical Review Board of all centres. Informed consent was obtained from all patients and control subjects.
Subjects
Patients with a recent wrist fracture were recruited to participate in the study. They had to be ambulant women and men, aged 45–80 years. The patients had to be recruited within 14 days after the fracture.
Exclusion criteria:
-
patients who were reoperated or remanipulated;
-
patients with comminuted fractures, pathologic fracture or polytrauma or fractures as a consequence of a traffic accident;
-
patients with other diseases that have a severe impact on quality of life;
-
patients with mental problems or patients who were unable to complete the questionnaire;
-
patients with recent (<2 years) clinical vertebral fracture or other osteoporotic fracture;
-
patients with recent unstable malignant disease or other badly controlled disease having a severe impact on quality of life.
Control subjects were outpatients with stable disorders such as treated hypertension and treated hypothyroidism. They were sex- and age-matched (within 3 years) to the patients.
Exclusion criteria:
-
patients who sustained fractures during the last 5 years;
-
patients with mental problems or patients unable to complete the questionnaire;
-
patients with recent unstable malignant disease or other badly controlled disease having a severe impact on quality of life;
-
patients with arthritis.
Methods
After informed consent was obtained, baseline data were collected including age, sex, date of fracture, type of fracture, fracture side, i.e. right or left, dominant or non-dominant, surgical or non-surgical treatment, and analgesics use. The IOF questionnaire for wrist fracture was administered at baseline, i.e. as soon as possible after the fracture, at 6 weeks, 3 months, 6 months and 1 year after the fracture. Other questionnaires to be completed by the patients were the Qualeffo-41 and EQ-5D. The questionnaires were always completed in the same order during clinic visits, i.e. the IOF questionnaire for wrist fracture, Qualeffo-41 (spine), and EQ-5D (EuroQol). If impossible, they were sent to the patients’ home address with a return envelope.
The patients completed questionnaires at a quiet place without assistance from others (including family). A study nurse explained the questionnaires to the patients, answered any questions and checked whether all questions had been completed. In the case of missing data (for postal questionnaire), patients were contacted by telephone. The control subjects completed the questionnaire only once.
The repeatability of the questionnaire was tested in the fracture patients at 3 months after the fracture. At 3 months, the patients were informed that they would receive the IOF-wrist fracture questionnaire (not Qualeffo-41 and EQ-5D) by mail within 2 weeks. They returned it by mail.
Data analysis
The study generated sets of questionnaires (three questionnaires, five time points) from patients with wrist fracture and a set of three questionnaires (one time point) from age- and sex-matched control subjects. The data sets (baseline data, three questionnaires) were sent to C. Cooper (Southampton) for data analysis. The wrist fracture questionnaire was scored as follows: Every question had five answer options from 1—healthy to 5—severe impact on quality of life. The scores on individual questions were summed up to a total score from 12 to 60, and this was recalculated to a score from 0 to 100. The Qualeffo-41 (spine) was scored as described previously with scores ranging from 0, representing the best, to 100, representing the worst quality of life [10]. The EQ-5D was scored according to the manual [14]. The overall score ranging from 0, the worst, to 1, the best quality of life, represents utility and can be used to calculate quality-adjusted life years (QALY) losses.
The test–retest reproducibility was assessed in the patients by comparing the results of the wrist fracture questionnaire at 12 weeks with the results at 14 weeks, as described above, using weighted Cohen kappa. The internal consistency was assessed by Cronbach alpha, comparing the wrist fracture questionnaire with the domains for pain and physical function of Qualeffo-41. Spearman rank correlations were calculated between similar domains of the three questionnaires. Wilcoxon signed-rank test was used to test for significant differences between each time point median score and the baseline median score. The sensitivity to change was assessed by regression analysis comparing the IOF-wrist fracture questionnaire with Qualeffo-41 and EQ-5D.
Results
Data were collected in 105 patients (92 women, 13 men) with wrist fracture and 74 control subjects (61 women, 13 men). Baseline data are shown in Table 1. The fracture was on the right side in 38 patients (36.5%) and on the left side in 66 patients (63.5%), and in one patient, the side was not known. The fracture was on the dominant side in 43 patients and non-dominant side in 60 patients (two missing). Most fractures were Colles type; three were Smith-type fracture. Surgical treatment was done in 32 patients. Analgesics were taken by 25 of 63 patients (42 missing) and algodystrophy was observed in 5 of 82 patients, whilst in 23, it was not known. Data at 12 months were available from 87 patients. Test–retest repeatability, analysed in patients by comparing results at 12 and 14 weeks, was restricted to 19 patients who completed the repeat questionnaire within 11–17 days. The weighted kappa statistic ranged from 0.33 to 0.74, and all scores were higher than 0.30. Cronbach alpha was assessed at baseline by comparing the wrist fracture questionnaire with the domains of pain and physical function of Qualeffo-41 (spine). Cronbach alpha was 0.96.
The 12 questions of the IOF-wrist fracture questionnaire were arranged in four domains: pain, upper limb symptoms, physical function and general health. The total score was calculated by adding up individual answers and normalising the total score to a 100-scale, 0 representing the best and 100 the worst quality of life. As expected, the frequency distribution of responses for each score differed between patients and control subjects. The median domain scores with interquartile range for the IOF-wrist fracture questionnaire, Qualeffo-41 (spine) and the EQ-5D are shown in Table 2. The discriminatory capacity of the 12 questions of the IOF-wrist questionnaire is shown in Table 3. Odds ratios for being in the patient group rather than in the control group were high and significant. The discriminatory capacity of the IOF-wrist and Qualeffo-41 domain scores is shown in Table 4 and Fig. 1. The discriminatory capacity was high except for the pain domain of Qualeffo-41.
Spearman rank correlations between similar domains of the three questionnaires were calculated. Most correlations between corresponding domains of the three questionnaires were highly significant. The highest correlations were observed between the physical function domains of the IOF-wrist fracture questionnaire and Qualeffo-41 (R = 0.81, P < 0.001) and between the total scores of the IOF-wrist fracture questionnaire and Qualeffo-41 (R = 0.77, P < 0.001) and the total scores of the IOF-wrist fracture questionnaire and the EQ-5D (R = −0.72, P < 0.001).
The patients with wrist fracture were followed up for 1 year after the fracture. Median scores and interquartile range for each time point and the significance versus baseline are shown in Table 5. Median domain scores for the IOF-wrist questionnaire during 1 year are shown in Fig. 2. The median domain scores of the IOF-wrist fracture questionnaire had significantly improved at 3 months. Improvement continued up to 6 months for upper limb symptoms, physical function, general health perception and overall score. The physical function improved a little more at 12 months. The scores on Qualeffo-41 and EQ-5D also improved up until 6 months, but the differences were smaller and some domains did not improve at all. Similar observations were made for the total score of these questionnaires (Fig. 3). Patients with a fracture on the right side had significantly higher scores immediately after the fracture for the IOF physical function domain [right vs left, median (interquartile range, IQR): 89 (75, 96) vs 71 (61, 86), P = 0.002]. A fracture on the dominant side was associated with higher scores than a fracture on the non-dominant side with regard to physical function [89 (75, 96) vs 70 (59, 82), P < 0.001] and overall score [67 (54, 79) vs 56 (47, 67), P = 0.016]. The latter is shown in Fig. 4. Patients undergoing surgical treatment had lower scores of Qualeffo-41, indicating better quality of life, on general health (P = 0.013) and mental health (P = 0.004) than patients with non-surgical treatment. Patients using analgesics had a higher scores of the IOF-wrist fracture questionnaire on pain (P = 0.009), on physical function (P = 0.001) and a higher overall score (P = 0.002) than patients not using analgesics.
Utility data could be calculated from the EQ-5D results. Immediately after the fracture, the utility was 0.59, increasing to 0.76 after 3 months and to 0.80 after 1 year. Assuming that the quality of life and the utility after 1 year are similar to that before the fracture, the utility loss due to the distal radius fracture is more than 0.20 in the first weeks. Most of the utility loss was regained after 3 months.
Discussion
The results from this study show that the IOF-wrist fracture questionnaire has an adequate repeatability, since the kappa statistic was moderate to good for most questions and quite similar to data obtained with Qualeffo-41 [10]. The interval of 2 weeks for test–retest repeatability may have negatively influenced the kappa statistic, as quality of life might change in these 2 weeks. The internal consistency was excellent as follows from the very high Crohnbach alpha, similar to that for Qualeffo-41 [10].
The IOF questionnaire on distal radius fracture discriminated well between patients with distal radius fracture and controls, as can be concluded from the high odds ratios. Similar data have been obtained with Qualeffo-41 [10]. The 12 questions discriminated to a similar degree between patients and control subjects, as should be expected, because the items were identified in a focus group of patients with wrist fracture. The discrimination was excellent on all questions, regarding upper limb symptoms, physical function and general health.
The 1-year follow-up in the patients with wrist fracture showed adequate responsiveness to change, since the median score of the IOF-wrist questionnaire decreased from 60 to 25 after 3 months and to less than 10 (on a scale of 100) within a year. The improvement was very rapid in the first 3 months after the fracture followed by a slower improvement up to 1 year. Whether improvement may still continue to occur after 1 year cannot be answered by this study. A similar course of improvement, i.e. fast improvement during the first 3 months, followed by a slower improvement to (almost) complete recovery at 1 year after the fracture, has been observed with other questionnaires and physical assessment, i.e. handgrip strength [13, 15]. As can be expected, fractures on the right side had a higher impact on quality of life than fractures on the left side. This effect was even more marked for the dominant versus non-dominant side. This confirms the face validity of the IOF-wrist fracture questionnaire.
Quality of life could not be measured before the fracture, but it is likely that it is similar or better than the estimate at 12 months after the fracture. The major decrease in quality of life was present during the first 6 months after the fracture. The loss of quality of life after wrist fracture may have been somewhat underestimated due to the exclusion criteria, since patients with comminuted fractures were excluded as well as patients with recent clinical vertebral fracture or other osteoporotic fracture. There was some loss to follow-up, which may also have influenced the results a little.
The utility loss after distal radius fracture was 0.14 during the first 3 months and 0.03 during the second 3 months assuming that utility was 0.80 at baseline similar to the value at 12 months. It indicates loss of QALY of about 0.09 during the first half year and 0.02 during the second half year. The total loss after wrist fracture adds up to 0.055 QALY. This result is similar to a previous study on quality of life after distal radius fracture [13]. In the previous study, the total quality of life lost was 0.05 QALY. An expert panel of the National Osteoporosis Foundation (NOF) estimated the quality of life loss after wrist fracture at 0.0464 in the first and 0.0006 in the second year after the fracture [16]. However, the QALY loss in the second year could increase to 0.30 in the case of dependency after the fracture according to the panel [16]. Thus, the QALY loss may depend on the age of the patient, the type of fracture and complications such as complex regional pain syndrome, all causing dependency of the patient on others. A similar variation was reported by the panel of the NOF regarding quality of life loss in the first year after vertebral fracture, ranging from 0.05 in a vertebral deformation to 0.50 QALY in a clinical fracture with severe pain [16]. Classification of vertebral fractures at diagnosis and a follow-up study on quality of life should be performed to better define the utility losses. The problem is that the onset of a vertebral deformity is often not known, as it may be asymptomatic.
Besides the new IOF instrument and the EQ-5D, other instruments have been used to assess recovery after wrist fracture. The disability of the arm, shoulder and hand (DASH) questionnaire, the patient-rated wrist evaluation (PRWE) and the short form 36 (SF-36) were combined with physical response measures in 59 patients with distal radius fracture [15]. In this study, the questionnaires were highly responsive in the first 3 months after the fracture when physical testing was not possible. The PRWE was more responsive than the DASH, and these two were more responsive than the SF-36, which is a generic quality of life instrument. The PRWE is a specific wrist questionnaire and the DASH is an upper limb questionnaire. Another analysis came to similar conclusions [17]. In our study, the specific IOF instrument was more responsive than the generic EQ-5D and the Qualeffo-41, which is a specific vertebral fracture questionnaire.
Strengths of our study include the design of our questionnaire after focus group interviews, the comparison with a generic instrument generating utility values and the longitudinal multicenter design. A limitation of our study is that the follow-up time points were not always strictly adhered at. However, when restricting the analysis to the subjects whose follow-up was within a strict time frame (e.g., 5–7 weeks for the 6-week time point), this did not change the results. Another weakness of our study is the fact that we did not compare our questionnaire with existing instruments such as DASH and PRWE. In addition, physical assessments such as handgrip strength were not done in our study.
In conclusion, the IOF-wrist fracture questionnaire appears to be a reliable and responsive quality of life questionnaire, showing sufficient repeatability, high internal consistency and adequate sensitivity to change. It is ready for use in patients with wrist fracture, preferably in combination with Qualeffo-41 for overall evaluation of quality of life with regard to osteoporosis.
References
Lips P (1997) Epidemiology and predictors of fractures associated with osteoporosis. Am J Med 103:3S–11S
Cooper C (1997) The crippling consequences of fractures and their impact on quality of life. Am J Med 103:12S–19S
World Health Organization (2003) The burden of musculoskeletal conditions at the start of the new millennium. WHO Technical Report Series 919. WHO Geneva, pp 1–218
Dijkstra PU, Groothoff JW, ten Duis HJ, Geertzen JHB (2003) Incidence of complex regional pain syndrome type I after fractures of the distal radius. Eur J Pain 7:457–462
Burger H, Van Daele PLA, Grashuis K, Hofman A, Grobbee DE, Schutte HE, Birkenhager JC, Pols HAP (1997) Vertebral deformities and functional impairment in men and women. J Bone Miner Res 12:152–157
Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR (1998) The association of radiologically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Pluijm SMF, Tromp AM, Smit JH, Deeg DJH, Lips P (2000) Consequences of vertebral deformities in older men and women. J Bone Miner Res 15:1564–1572
Lips P, Van Schoor NM (2005) Quality of life in patients with osteoporosis. Osteoporosis Int 16:447–455
Silverman SL, Minshall ME, Shen W, Harper KD, Xie S, on behalf of the Health-Related Quality of Life Subgroup of the Multiple Outcomes of Raloxifene Evaluation Study (2001) The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum 44:2611–2619
Lips P, Cooper C, Agnusdei D, Working Party for Quality of Life of the European Foundation for Osteoporosis et al (1999) Quality of life in patients with vertebral osteoporosis. Validation of the quality of life questionnaire of the European Foundation for Osteoporosis (Qualeffo). Osteoporosis Int 10:150–160
Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392
Van Schoor NM, Knol DL, Glas CAW, Ostelo RWJG, Leplege A, Cooper C, Johnell O, Lips P (2006) Development of the Qualeffo-31, an osteoporotic-specific quality-of-life questionnaire. Osteoporosis Int 17:543–551
Dolan P, Torgerson D, Kumar Kakarlapadi T (1999) Health-related quality of life in Colles fracture patients. Osteoporosis Int 9:196–199
Kind P (1996) The EuroQol instrument: an index of health-related quality of life. In: Spilker B (ed) Quality of life and pharmaeconomics in clinical trials, 2nd edn. Lippincott-Raven, Philadelphia, pp 191–201
MacDermid JC, Richards RS, Donner A, Bellamy N, Roth JH (2000) Responsiveness of the SF-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg 25A:330–340
National Osteoporosis Foundation (1998) Osteoporosis: review of the evidence for prevention, diagnosis, and treatment and cost-effectiveness analysis. Osteoporosis Int 8:S1–S88
Changulani M, Okonkwo U, Keswani T, Kalairajah Y (2008) Outcome evaluation measures for wrist and hand—which one to choose? Int Orthopaedics (SICOT) 32:1–6
Acknowledgements
The International Osteoporosis Foundation is acknowledged for its support in the design and performance of the study.
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
† Dr. O. Johnell – deceased.
Appendix
Appendix
IOF-wrist fracture questionnaire
Quality of life questionnaire for patients with wrist fracture.
All questions regard the situation in the last week, except question 12.
All questions should be answered irrespective of the side of fracture and the side of dominance.









Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Lips, P., Jameson, K., Bianchi, M.L. et al. Validation of the IOF quality of life questionnaire for patients with wrist fracture. Osteoporos Int 21, 61–70 (2010). https://doi.org/10.1007/s00198-009-0946-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-0946-6