Abstract
Summary
This study determined the cost of treating fractures at osteoporotic sites (except spine fractures) for the year following fracture. While the average cost of treating a hip fracture was the highest of all fractures ($46,664 CAD per fracture), treating other fractures also accounted for significant expenditures ($5,253 to $10,410 CAD per fracture).
Introduction
This study aims to determine the mean direct medical cost of treating fractures at peripheral osteoporotic sites in the year post-fracture (through 2 years post-hip fracture).
Methods
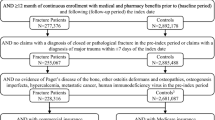
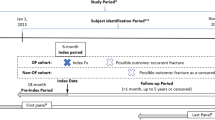
Health administrative databases from the province of Quebec, Canada were used to estimate the cost of treating peripheral fractures at osteoporotic sites for the year following fracture (through 2 years for hip fractures). Included in costs analyses were physician claims, emergency and outpatient clinic costs, hospitalization costs, and subsequent costs for treatment of complications.
Results
A total of 15,827 patients (mean age 72 years) who suffered one fracture at an osteoporotic site had data for analyses. Hip/femur fractures had the highest rate of hospital stays related to fracture (91%) and the highest rate of hospital stays associated with a post-fracture complication (8%). In the year following fracture, the mean (SD) costs (2009 Canadian dollars) of treating acute fractures and post-fracture complications were: hip/femur fracture $46,664 ($43,198), wrist fracture $5,253 ($18,982), and fractures at other peripheral sites $10,410 ($27,641). The average (SD) cost of treating post-fracture complications at the hip/femur in the second year post-fracture was $1,698 ($12,462). Hospitalizations associated with the fracture accounted for 88% of the total cost of fracture treatment.
Conclusions
The treatment of hip fractures accounts for a significant proportion of the costs associated with the treatment of peripheral osteoporotic fractures. Interventions to reduce the incidence of fractures, particularly hip fractures, would result in significant cost savings to the health care system and would preserve quality of life in many patients.



Similar content being viewed by others
References
Papaioannou A, Kennedy CC, Ioannidis G, Sawka A, Hopman WM, Pickard L, Brown JP, Josse RG, Kaiser S, Anastassiades T, Goltzman D, Papadimitropoulos M, Tenenhouse A, Prior JC, Olszynski WP, Adachi JD (2008) The impact of incident fractures on health-related quality of life: 5 years of data from the Canadian Multicentre Osteoporosis Study. Osteoporos Int 20:703–714
Ioannidis G, Papaioannou A, Hopman WM, khtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ 181:265–271
Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E (2001) Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 12:271–278
Jean S, Candas B, Belzile E, Morin S, Bessette L, Dodin S, Brown JP (2011) Algorithms can be used to identify fragility fracture cases in physician-claims databases. Osteoporos Int (in press)
Bessette L, Ste-Marie LG, Jean S, Davison KS, Beaulieu M, Baranci M, Bessant J, Brown JP (2008) The care gap in diagnosis and treatment of women with a fragility fracture. Osteoporos Int 19:79–86
Mackey DC, Lui LY, Cawthon PM, Bauer DC, Nevitt MC, Cauley JA, Hillier TA, Lewis CE, Barrett-Connor E, Cummings SR (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298:2381–2388
Curtis JR, Taylor AJ, Matthews RS, Ray MN, Becker DJ, Gary LC, Kilgore ML, Morrisey MA, Saag KG, Warriner A, Delzell E (2009) “Pathologic” fractures: should these be included in epidemiologic studies of osteoporotic fractures? Osteoporos Int 20:1969–1972
(2011) RAMQ medical specialists’ and general practitioners’ manual. http://wwwramq.gouv.qc.ca. Accessed 2 February 2011
Shi N, Foley K, Lenhart G, Badamgarav E (2009) Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone 45:1084–1090
Burge R, wson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Piscitelli P, Iolascon G, Gimigliano F, Muratore M, Camboa P, Borgia O, Forcina B, Fitto F, Robaud V, Termini G, Rini GB, Gianicolo E, Faino A, Rossini M, Adami S, Angeli A, Distante A, Gatto S, Gimigliano R, Guida G (2007) Incidence and costs of hip fractures compared to acute myocardial infarction in the Italian population: a 4-year survey. Osteoporos Int 18:211–219
Chen LT, Lee JA, Chua BS, Howe TS (2007) Hip fractures in the elderly: the impact of comorbid illnesses on hospitalisation costs. Ann Acad Med Singapore 36:784–787
Borgstrom F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Lunsjo K, Thorngren KG, Sernbo I, Rehnberg C, Jonsson B (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650
Conflicts of interest
Dr. Bessette has received research grants from Abbott, Amgen, Bristol-Myers-Squibb, Eli Lilly, Merck, Pfizer, and Roche, has received consulting fees or other remuneration from Abbott, Amgen, Merck, Novartis, Pfizer, and Roche and has participated on the Speakers Bureau for Amgen, Novartis, Merck, Pfizer, Roche, and Warner Chilcott. Dr. Brown has received research grants from Abbott, Amgen, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche, has received consulting fees or other remuneration from Abbott, Amgen, Eli Lilly, Novartis, Merck, and Warner Chilcott and has participated on the Speakers Bureau for Eli Lilly, Amgen, Novartis, Merck, and Warner Chilcott. Dr. Davison has received consulting fees or other remuneration from Amgen and Servier and has participated on the Speakers Bureau for Amgen, Merck, and Servier. Dr. Ste-Marie has received research grants from the Alliance for Better Bone Health and Novartis, has received consulting fees or other remuneration from the Alliance for Better Bone Health, Amgen, Novartis, Eli Lilly, and Servier and has participated on the Speakers Bureau for the Alliance for Better Bone Health, Amgen, Novartis, Eli Lilly, Servier, and Merck. No other authors have a conflict or interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
The ROCQ Programme was funded by Merck Canada, Inc., Procter and Gamble Pharmaceuticals, now Warner Chilcott Canada Co, Sanofi-Aventis group, Amgen Canada Inc., Eli Lilly Canada, Inc., and Novartis Pharmaceuticals Canada, Inc. None of the funding sources had a role in the collection, analysis, or interpretation of the data or in the decision to publish this article.
Appendices
Appendix 1
Classification of principal diagnostic codes at hospitalization.
Appendix 2
Selection of hospital staysa.

aUnshaded cells with hospitals stays unrelated to the fracture were not used in the cost analysis. Dark gray-shaded cells with hospital stays considered definitively related to the fracture and pale gray-shaded cells with hospitals stays considered as related to a complications.
bDefinition of time between hospital admission and fracture differ between fracture site:
-
Hip fracture: direct = 0–14 days, possible = 15–180 days, first year = 181–365 days, second year 365–730 days
-
Pelvis, knee, tibia/fibula: direct = 0–10 days, possible = 11–180 days, first year = 181–365 days
-
Shoulder/humerus, forearm/elbow, wrist, foot, ankle: direct = 0–10 days, possible = 11–120 days, first year = 121–365 days
cDefinitions of what is considered a principal diagnostic code for fracture, associated to a fracture, of a complication of fracture are given in Appendix 1.
Rights and permissions
About this article
Cite this article
Bessette, L., Jean, S., Lapointe-Garant, MP. et al. Direct medical costs attributable to peripheral fractures in Canadian post-menopausal women. Osteoporos Int 23, 1757–1768 (2012). https://doi.org/10.1007/s00198-011-1785-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1785-9