Abstract
Rationale
Up to 60% of children with attention-deficit/hyperactivity disorder (ADHD) suffer from comorbid affective or behavioral impairments, the most common condition being oppositional defiant disorder (ODD), which occurs in 40–60% of children with ADHD.
Objectives
This post hoc meta-analysis was performed to determine the effect of the presence of comorbid ODD symptoms on clinical outcomes among pediatric and adolescent subjects being treated for ADHD.
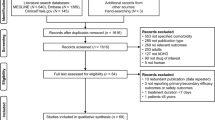
Methods
Acute-phase data were analyzed from three randomized, double-blind, placebo-controlled studies in outpatients aged 6–16 and meeting the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, criteria for ADHD. Subjects received placebo or atomoxetine (max 1.8 mg/kg/day, daily) for 6–8 weeks. Patients were diagnosed with comorbid ODD on structured diagnostic interview (Schedule for Affective Disorders and Schizophrenia for School-aged Children—Present and Lifetime Versions).
Results
Of the 512 subjects studied, 158 were diagnosed with comorbid ODD. Relative to placebo, atomoxetine treatment significantly reduced ADHD symptoms in both ODD-comorbid and noncomorbid subjects irrespective of the comorbidity with ODD. ADHD subjects also showed significant improvements from baseline on most of the psychosocial measures of the child health questionnaire irrespective of the comorbidity with ODD. Reduction in ODD symptoms was highly related to the magnitude of ADHD response.
Conclusions
Atomoxetine treatment significantly reduced ADHD symptoms in both ODD-comorbid and noncomorbid subjects to similar extents, indicating that the presence of comorbid symptoms of oppositionality does not affect clinical outcomes of treatment of ADHD with atomoxetine.
Similar content being viewed by others
References
Banaschewski T, Brandeis D, Heinrich H, Albrecht B, Brunner E, Rothenberger A (2003) Association of ADHD and conduct disorder—brain electrical evidence for the existence of a distinct subtype. J Child Psychol Psychiatry 44:356–376
Baving L, Rellum T, Kaucht M, Schmidt MH (2006) Children with oppositional-defiant disorder display deviant attentional processing independent of ADHD symptoms. J Neural Transm 113:685–693
Biederman J, Newcorn J, Sprich S (1991) Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 148:564–577
Biederman J, Mick E, Faraone SV, Braaten E, Doyle A, Spencer T, Wilens TE, Frazier E, Johnson MA (2002) Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry 159:36–42
Bostic JQ, Biederman J, Spencer TJ, Wilens TE, Prince JB, Monuteaux MC, Sienna M, Polisner DA, Hatch M (2000) Pemoline treatment of adolescents with attention deficit hyperactivity disorder: a short-term controlled trial. J Child Adolesc Psychiatr Nurs 10:205–216
Burns GL, Walsh JA (2002) The influence of ADHD-hyperactivity/impulsivity symptoms on the development of oppositional defiant disorder symptoms in a 2-year longitudinal study. J Abnorm Child Psychol 30:245–256
Burns GL, Boe B, Walsh JA, Sommers-Flanagan R, Teegarden LA (2001) A confirmatory factor analysis on the DSM-IV ADHD and ODD symptoms: what is the best model for the organization of these symptoms? J Abnorm Child Psychol 29:339–349
Chen TJH, Blum K, Mathews D, Fisher L, Schnautz N, Braverman ER, Schoolfield J, Downs BW, Comings DE (2005) Are dopaminergic genes involved in a predisposition to pathological aggression? Hypothesizing the importance of “super normal controls” in psychiatricgenetic research of complex behavioral disorders. Med Hypotheses 65:703–707
Comings DE, Chen C, Wu S, Muhleman D (1999) Association of the androgen receptor gene (AR) with ADHD and conduct disorder. Neuroreport 10:1589–1592
Comings DE, Gade-Andavolu R, Gonzalez N, Wu S, Muhleman D, Blake H, Chiu F, Wang E, Farwell K, Darakjy S, Baker R, Dietz G, Saucier G, MacMurray JP (2000) Multivariate analysis of associations of 42 genes in ADHD, ODD and conduct disorder. Clin Genet 58:31–40
Conners CK (1997) Conners’ rating scales: revised technical manual. Multi-Health Systems, North Tonawanda, NY
Connor DF, Barkley RA, Davis HT (2000) A pilot study of methylphenidate, clonidine, or the combination in ADHD comorbid with aggressive oppositional defiant or conduct disorder. Clin Pediatr (Bologna) 39:15–25
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R (1998) ADHD rating scale-IV: checklists, norms, and clinical interpretations. Guilford, New York
Faraone SV, Sergeant J, Gillberg C, Biederman J (2003) The worldwide prevalence of ADHD: is it an American condition? World Psychiatry 2:104–113
Goldman LS, Genel M, Bezman RJ, Slanetz PJ (1998) Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. JAMA 279:1100–1107
Guy W (1976) ECDEU Assessment manual for psychopharmacology, revised. Publication ADM 76-338. United States Department of Health, Education, and Welfare, Bethesda, MD
Hazell P, Zhang S, Wolanczyk T, Barton J, Johnson M, Zuddas A, Danckaerts M, Ladikos A, Benn D, Yoran-Hegesh R, Zeiner P, Michelson D (2006) Comorbid oppositional defiant disorder and the risk of relapse during 9 months of atomoxetine treatment for attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 15:886–894
Hechtman L (2000) Assessment and diagnosis of attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am 9:481–498
Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, March JS, Arnold LE, Cantwell DP, Conners CK, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Pelham WE, Severe JB, Swanson JM, Wells KC, Wigal T, Vitiello B (2001) ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 40:147–158
Kaplan S, Heiligenstein J, West S, Busner J, Harder D, Dittmann R, Casat C, Wernicke JF (2004) Efficacy and safety of atomoxetine in childhood attention-deficit/hyperactivity disorder with comorbid oppositional defiant disorder. J Atten Disord 8:45–52
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997) Schedule for affective disorders and schizophrenia for school-age children—present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
Kelsey DK, Sumner CR, Casat CD, Coury DL, Quintana H, Saylor KE, Sutton VK, Gonzales J, Malcolm SK, Schuh KJ, Allen AJ (2004) Once-daily atomoxetine treatment for children with attention-deficit/hyperactivity disorder, including an assessment of evening and morning behavior: a double-blind, placebo-controlled trial. Pediatrics 114:e1–e8
Klein RG, Abikoff H, Klass E, Ganaeles D, Seese LM, Pollack S (1997) Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Arch Gen Psychiatry 54:1073–1080
Klorman R, Hazel-Fernandez LA, Shaywitz SE, Fletcher JM, Marchione KE, Holahan JM, Stuebing KK, Shaywitz BA (1999) Executive functioning deficits in attention-deficit/hyperactivity disorder are independent of oppositional defiant or reading disorder. J Am Acad Child Adolesc Psychiatry 38:1148–1155
Kolko DJ, Bukstein OG, Barron J (1999) Methylphenidate and behavior modification in children with ADHD and comorbid ODD or CD: main and incremental effects across settings. J Am Acad Child Adolesc Psychiatry 38:578–586
Kuhne M, Schachar R, Tannock R (1997) Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 36:1715–1725
Landgraf JM, Abetz L, Ware JE (1996) The CHQ user’s manual, 1st edn. The Health Institute, New England Medical Center, Boston, MA
Landgraf JM, Rich M, Rappaport L (2002) Measuring quality of life in children with attention-deficit/hyperactivity disorder and their families—development and evaluation of a new tool. Arch Pediatr Adolesc Med 156:384–391
Michelson D, Faries D, Wernicke J, Kelsey D, Kendrick K, Sallee FR, Spencer T; Atomoxetine ADHD Study Group (2001) Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose–response study. Pediatrics 108:e83
Michelson D, Allen AJ, Busner J, Casat C, Dunn D, Kratochvil C, Newcorn J, Sallee FR, Sangal RB, Saylor K, West S, Kelsey D, Wernicke J, Trapp NJ, Harder D (2002) Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry 159:1896–1901
MTA Cooperative Group (1999a) A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56:1073–1086
MTA Cooperative Group (1999b) Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56:1088–1096
Newcorn JH, Miller SR, Ivanova I, Schulz KP, Kalmar J, Marks DJ, Halperin JM (2004) Adolescent outcome of ADHD: impact of childhood conduct and anxiety disorders. CNS Spectr 9:668–678
Newcorn J, Spencer TJ, Biederman J, Milton DR, Michelson D (2005) Atomoxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry 44:240–248
Oosterlaan J, Scheres A, Sergeant JA (2005) Which executive functioning deficits are associated with AD/HD, ODD/CD and comorbid AD/HD+ODD/CD? J Abnorm Child Psychol 33:69–85
Pelham WE, Aronoff HR, Midlam JK, Shapiro CJ, Gnagy EM, Chronis AM, Onyango AN, Forehand G, Nguyen A, Waxmonsky J (1999) A comparison of Ritalin and Adderall: efficacy and time-course in children with attention-deficit/hyperactivity disorder. Pediatrics 103:e431
Prince JB, Wilens TE, Biederman J, Spencer TJ, Millstein R, Polisner DA, Bostic JQ (2000) A controlled study of nortriptyline in children and adolescents with attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 10:193–204
Sondeijker FEPL, Ferdinand RF, Oldehinkel AJ, Veenstra R, De Winter AF, Ormel J, Verhulst FC (2005) Classes of adolescents with disruptive behaviors in a general population sample. Soc Psychiatry Psychiatr Epidemiol 40:931–938
Spencer TJ, Abikoff HB, Connor DF, Biederman J, Pliszka SR, Boellner S, Read SC, Pratt R (2006) Efficacy and safety of mixed amphetamine salts extended release (Adderall XR) in the management of oppositional defiant disorder with or without comorbid attention-deficit/hyperactivity disorder in school-aged children and adolescents: a 4-week, multicenter, randomized, double-blind, parallel-group, placebo-controlled, forced-dose-escalation study. Clin Ther 28:402–418
Wechsler D (1991) Wechsler Intelligence Scale for Children (WISC-III). The Psychological Corporation. Harcourt Brace and Company, San Antonio, TX
Weiss M, Tannock R, Kratochvil C, Dunn D, Velez-Borras J, Thomason C, Tamura R, Kelsey D, Stevens L, Allen AJ (2005) A randomized, placebo-controlled study of once-daily atomoxetine in the school setting in children with ADHD. J Am Acad Child Adolesc Psychiatry 44:647–655
World Medical Association (2000) Declaration of Helsinki: recommendations guiding medical doctors in biomedical research involving human subjects. As adopted by the 18th World Medical Association General Assembly, Helsinki, Finland, June 1964 and amended by the 52nd General Assembly, Edinburgh, Scotland, October 2000
Acknowledgment
Research funded by Eli Lilly and Company.
Conflict of interest statement
Dr. Joseph Biederman receives/d research support from, is/has been a speaker for, or is/has been on the advisory board for the following Pharmaceutical Companies:
Shire, Eli Lilly, Pfizer, McNeil, Abbott, Bristol-Myers-Squibb, New River Pharmaceuticals, Cephalon, Janssen, Novartis, UCB Pharma, Astra-Zeneca, Forest Laboratories, Glaxo-Smith Kline and Neurosearch
Other Sources of Research Support:
-
Private Foundations
-
Stanley Medical Institute, Inc, Lilly Foundation, Prechter Foundation
-
-
NIH
-
NIMH, NICHD and NIDA
-
Dr. Thomas Spencer receives research support from the following sources: Shire Laboratories, Inc and Eli Lilly & Company, Glaxo-Smith Kline, Pfizer Pharmaceutical, McNeil Pharmaceutical, Novartis Pharmaceutical, and NIMH
Dr. Thomas Spencer is a speaker for the following speaker’s bureaus: Glaxo-Smith Kline, Eli Lilly & Company, Novartis Pharmaceutical, Wyeth Ayerst, Shire Laboratories Inc, McNeil Pharmaceutical
Dr. Thomas Spencer is on the advisory board for the following pharmaceutical companies: Shire Laboratories, Inc and Eli Lilly & Company, Glaxo-Smith Kline, Pfizer Pharmaceutical, McNeil Pharmaceutical, and Novartis Pharmaceutical
Dr. Jeffrey Newcorn has not disclosed any conflicts of interest.
Dr. Haitaio Gao is an employee of Eli Lilly & Company.
Dr. Denise Milton is an employee of Eli Lilly & Company.
Dr. Peter D. Feldman is an employee of Eli Lilly & Company.
Dr. Michael M. Witte is an employee of Eli Lilly & Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biederman, J., Spencer, T.J., Newcorn, J.H. et al. Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: a meta-analysis of controlled clinical trial data. Psychopharmacology 190, 31–41 (2007). https://doi.org/10.1007/s00213-006-0565-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-006-0565-2