Abstract
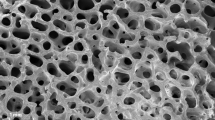
We randomly assigned 17 patients with scaphoid non-union at the proximal pole to three treatment groups: (1) autologous iliac graft (n=6), (2) autologous iliac graft + osteogenic protein-1 (OP-1; n=6), and (3) allogenic iliac graft + OP-1 (n=5). Radiographic, scintigraphic, and clinical assessments were performed throughout the follow-up period of 24 months. OP-1 improved the performance of both autologous and allogenic bone implants and reduced radiographic healing time to 4 weeks compared with 9 weeks in group 1. Helical CT scans and scintigraphy showed that in OP-1-treated patients sclerotic bone was replaced by well-vascularised bone. The addition of OP-1 to allogenic bone implant equalised the clinical outcome with the autologous graft procedure. Consequently the harvesting of autologous graft can be avoided.
Résumé
Nous avons réparti 17 malades avec une pseudarthrose du pôle proximal du scaphoide en trois groupes aléatoires de traitement: (1) greffe autologue iliaque (n=6), (2) greffe autologue iliaque + protéine osteogenique-1 (OP-1; n=6), et (3) greffe allogène iliaque + OP-1 (n=5). L’estimation radiographique, scintigraphique et clinique a été exécutée pendant une période de suivi de 24 mois. L’OP-1 a amélioré la performance des autogreffes et des allogreffes osseuses et a réduit le temps curatif radiographique à 4 semaines, comparé à 9 semaines dans le groupe traité uniquement avec de l’os autologues. Chez les malades traités avec l’OP-1, la tomodensitométrie hélicoïdale et la scintigraphie ont montré que l’os scléreux était remplacé par de l’os bien vascularisé. L’addition d’OP-1 à la greffe allogène a égalisé le résultat clinique avec la procédure de greffe autologue et a permis de supprimer le temps de prise de greffe.


Similar content being viewed by others
References
Bilic R, Korzinek K (1987) Results of scaphoid non-union treatment by Matti-Russe procedure using compressed cancellous bone. Unfallchirurg 90:134–138
Burkus JK, Gornet MF, Dickman CA, Zdeblick TA (2002) Anterior lumbar interbody fusion using rhBMP-2 with tapered interbody cages. J Spinal Disord Tech 15:337–349
Cook SD, Rueger DC (2002) Preclinical models of recombinant BMP induced healing of orthopedic defects. In: Vukicevic S, Sampath K (eds) Bone morphogenetic proteins: from laboratory to clinical practice. Birkhäuser, Basel, pp 121–144
Djapic T, Kusec V, Jelic M, Vukicevic S, Pecina M (2003) Compressed homologous cancellous bone and bone morphogenetic protein (BMP)-7 or bone marrow accelerate healing of long-bone critical defects. Int Orthop 27:326–330
Fisk GR (1984) The wrist. J Bone Joint Surg Br 66:396–407
Friedlaender GE, Perry CR, Cole JD, Cook SD, Cierny G, Muschler GF et al (2001) Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am 83:S151–S158
Green DP (1985) The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg [Am] 10:597–605
Inoue G, Shionoya K, Kuwahata Y (1997) Ununited proximal pole scaphoid fractures. Treatment with Herbert screw in 16 cases followed for 0.5–8 years. Acta Orthop Scand 68:124–127
Kujala S, Raatikainen T, Ryhänen J, Kaarela O, Jalovaara P (2002) Composite implant of native bovine bone morphogenetic protein (BMP) and biocoral in the treatment of scaphoid nonunions—a preliminary study. Scand J Surg 91:186–190
Lieberman JR, Daluiski A, Einhorn TA (2002) The role of growth factors in the repair of bone: biology and clinical applications. J Bone Joint Surg Am 84:1032–1044
Martinovic S, Simic P, Borovecki F, Vukicevic S (2004) Biology of bone morphogenetic proteins. In: Vukicevic S, Sampath K (eds) Bone morphogenetic proteins: regeneration of bone and beyond. Birkhäuser, Basel, pp 45–72
Merrell GA, Wolfe SW, Slade JF III (2002) Treatment of scaphoid nonunions: quantitative meta-analysis of the literature. J Hand Surg [Am] 27:685–691
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Pecina M, Giltaij LR, Vukicevic S (2001) Orthopaedic applications of osteogenic protein-1 (BMP-7). Int Orthop 25:203–208
Sanders WE (1988) Evaluation of the humpback scaphoid by computed tomography in the longitudinal axial plane of the scaphoid. J Hand Surg [Am] 13:182–187
Sherman SB, Greenspan SB, Norman A (1983) Osteonecrosis of the distal pole of the carpal scaphoid following fracture—a rare complication. Skeletal Radiol 9:189–191
Stark A, Brostrom LA, Svartengren G (1987) Scaphoid nonunion treated with the Matti-Russe technique. Long-term results. Clin Orthop 214:175–180
Tambe AD, Cutler L, Stilwell J, Murali SR, Trail IA, Stanley JK (2005) Scaphoid non-union: the role of vascularized grafting in recalcitrant non-unions of the scaphoid. J Hand Surg [Br] http://www.dx.doi.org/10.1006.2005.09.09.012
Trezies AJ, Davis TR, Barton NJ (2000) Factors influencing the outcome of bone grafting surgery for scaphoid fracture non-union. Injury 31:605–607
Vukicevic S, Stavljenic A, Pecina M (1995) Discovery and clinical applications of bone morphogenetic proteins. Eur J Chem Clin Biochem 33:661–671
Warren-Smith CD, Barton NJ (1988) Non-union of the scaphoid: Russe graft vs Herbert screw. J Hand Surg 13B:83–86
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bilic, R., Simic, P., Jelic, M. et al. Osteogenic protein-1 (BMP-7) accelerates healing of scaphoid non-union with proximal pole sclerosis. International Orthopaedics (SICO 30, 128–134 (2006). https://doi.org/10.1007/s00264-005-0045-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-005-0045-z