Abstract
Objective
To investigate the psychosocial impact of having an implantable cardioverter defibrillator (ICD) in adults with Tetralogy of Fallot (ToF).
Methods
Included were 26 ToF-patients with an ICD (age 44 ± 12 years), and two control groups consisting of 28 ToF-patients without an ICD (age 40 ± 10 years) and a group of 35 ICD-patients of older age without ToF (age 72.0 ± 8 years). This last control group was chosen to represent the “older general ICD population” with acquired heart disease seen at the out-patient clinic. Psychosocial functioning encompassed daily functioning, subjective health status, quality of life, anxiety, depression, coping and social support.
Results
ToF-patients with ICD showed diminished psychosocial functioning in comparison to ToF-patients without ICD. This was reflected by diminished subjectively perceived physical functioning (p = 0.01), general health perception (p < 0.01) and a lower satisfaction with life (p = 0.02). In comparison to older ICD-patients, ToF-patients with ICD showed less satisfaction with life (p = 0.03), experienced more anxiety (p = 0.01) and showed less favourable coping styles, although physical functioning was better for ToF-patients with ICD than for older ICD-patients (p = 0.01). More inappropriate shocks were found in ToF-patients with ICD compared to the older ICD-patients.
Conclusion
In patients with ToF, ICD implantation had a major impact on psychosocial functioning which should be taken into account when considering ICD implantation in these young patients. To help improve psychosocial functioning, psychological counselling attuned to the specific needs of these patients may be useful.
Similar content being viewed by others
Introduction
The leading cause of mortality in adult patients with congenital heart disease (ConHD) is sudden cardiac death (SCD) [1]. In comparison with the general population, an adult patient with ConHD has a 25–100 fold increased risk to die as a result of SCD [2]. Implantable cardioverter defibrillators (ICDs) are being used as therapy for patients that are at high risk for developing, or have survived a life-threatening cardiac arrhythmia [3]. However, the indication of ICD therapy in patients with ConHD is still a matter of debate. A recent publication from our group investigating the efficacy of ICD therapy in ConHD patients demonstrated that 23% of all patients received an appropriate shock, and 41% of the investigated patients received at least one inappropriate shock [4]. This inappropriate shock rate is higher than in other patient groups. Other studies reported an inappropriate shock rate of around 25%, and an appropriate shock rate of around 22–30% in ConHD patients [3].
Congenital heart disease patients not only have to cope with an increased risk to die as a result of SCD [2]. In addition, the implantation of an ICD with associated inappropriate shocks, which occur when the patient is fully conscious, may cause anxiety for shock, anxiety for premature death and stress, hereby worsening the psychological problems [6, 7]. Patients receiving ICD therapy may show reduced quality of life, subjective health status and diminished social functioning. Anxiety and fear for ICD discharge does not only affect the patient, it can also influence the behaviour of relatives and friends surrounding the patient. Sometimes these “significant others” experience fear and anxiety, which may have a cumulative anxiety arousing effect on the patient [8]. The aim of this study was to investigate the psychosocial impact that ICD therapy has in (young) adults with Tetralogy of Fallot (ToF). We chose patients with ToF because most of the ICD implantations in the ConHD population occur in these patients [3].
Two control groups were selected; the first control group consisted of ToF-patients without an ICD. We selected these patients to investigate the impact of the ICD while holding the groups comparable on cardiac diagnosis and hemodynamic burden. The second control group consisted of older acquired heart disease ICD patients. This group represents the “general” ICD population as seen in an outpatient clinic. By choosing this group, we could make a comparison with a “general” average ICD patient. Age may be a factor in acceptance of an ICD. Also, knowledge about the psychosocial functioning of patients with an ICD comes from studies focusing on these “regular ICD-patients”. These patients are older and have acquired heart disease. The psychosocial problems seen in these older patients may be quite different than those seen in younger ConHD patients receiving ICD therapy. Young patients do not only experience the problems associated with the ICD but also carry the burden of having grown-up with a congenital heart defect. They also experience more inappropriate shocks than non-ConHD patients [4]. These shocks may lead to anxiety, psychosocial problems and avoidance behaviour, limiting patients in social contacts, and leisure time activities. In addition, overprotective parents of ConHD patients may be a limiting factor as well. Therefore, we hypothesized that the psychosocial impact of receiving ICD therapy in young ConHD patients may be more substantial.
Finally, we wanted to compare whether styles of coping and adjustment to ICD therapy differed between younger ConHD patients with an ICD (ToF + ICD) and older patients with acquired heart disease receiving ICD therapy (ICD), when adjusted for the time-period of receiving ICD therapy.
Methods
Study design and population
This is a cross-sectional, multicentre study.
Inclusion criteria
Our database consisted of three groups. The first group consisted of Fallot-patients with ICD (ToF + ICD). This population was selected using the CONCOR [9] registry in The Netherlands and a Belgian tertiary care centre adult ConHD database. The CONCOR registry is a nationwide database consisting of adult patients with ConHD, including medical history. The selection of this patient sample is described in detail in the paper of Yap et al. [4]. This group was used as the study population. The second group consisted of Fallot-patients without ICD (ToF) and was also identified using the CONCOR registry. This ToF group consisted of 28 patients without significant differences in age, sex and NYHA class compared to the study group ToF + ICD. We used this group as our first control group. The third group (ICD) consisted of 35 older ICD-patients with another form of heart disease, mainly ischaemic heart disease. These patients did not have ConHD. This group was identified using the Erasmus MC ICD registry, and did not show significant differences regarding gender compared to the ToF + ICD group. We used this last group as our second control group. For all selected patients, data were collected form medical records, with permission of the patients and physicians.
This study was approved by the institutional ethical committees. All patients provided informed consent before participating in this study.
Patient sample
Of the 44 eligible patients from the ToF + ICD group, 13 were lost to follow-up and 3 patients died before inclusion in this study. The present patient sample consisted of the remaining 28 adults of whom two refused to participate, resulting in a response rate of 93% for the ToF + ICD group. The mean age of this group was 44 years (±12 years).
There were no differences between participants and non-participants on age, age at Fallot correction, shunt before correction, reoperations, age at ICD implantation, follow-up time, indication for ICD implantation, NYHA class or the amount of shocks.
In order to ensure that ICDs of patients are programed optimally, patients visited the outpatient clinic every 6 months, or sooner if they had complaints. The functionality of the ICD device was assessed by skilled technicians and adapted if necessary. All appropriate and inappropriate shocks were recorded.
Indications for ICD implantation in ToF-patients
The index event before ICD implantation was spontaneous sustained ventricular tachycardia (VT) in 14 patients (54%), cardiac arrest in 5 patients (19%), (pre) syncope in 5 patients (19%) and other in 2 patients (8%).
Assessment procedure
All patients were approached uniformly and signed an informed consent before participating. All patients completed the questionnaires at home and returned them by mail. Missing items were retrieved by means of a telephone call.
Instruments
The psychological examination consisted of the following questionnaires.
Biographical characteristics
A semi-structured questionnaire was designed to assess biographical variables such as nationality, living conditions, marital-, educational- and occupational status [10]. The educational attainments were evaluated excluding two patients living in institutions because of psychosocial problems.
Subjective health status
The subjective health status was assessed by the SF-36 Health Survey [11]. Good reliability and validity for the Dutch version of the SF-36 has been reported [12].
Satisfaction with Life Scale
The Satisfaction with Life Scale (SWLS) was used as an indicator of the satisfaction with life. This scale has been proven psychometrically sound to be used in ConHD patients [13].
Linear Analogue Scale Quality of Life
The Linear Analogue Scale (LAS) was used to measure self-perceived quality of life. The LAS has been proven valid, reliable and responsive for the ConHD population [13].
Hospital Anxiety and Depression Scale (HADS)
This scale measures the presence and severity of anxiety and depression in patients. The HADS has been validated for the general Dutch population and is stable across medical settings and age groups [14, 15].
Utrecht Coping List
The Utrecht Coping List (UCL) is a reliable and standardised self-report questionnaire of coping styles. The satisfactory validity of the UCL has been described elsewhere [16]. Construct validity and predictive validity has been examined for the UCL.
Implanted Devices Adjustment Scale
The Implanted Device Adjustment Scale (IDAS) measures the psychological adjustment of a patient to an implanted (ICD) pacemaker. The IDAS has been described valid, reliable and responsive [17].
Perceived Social Support Scale
The Perceived Social Support Scale 12 item version (PSSS12) measures the interactions and discrepancies that people experience in receiving social support from their direct environment [18].
Statistical methods
Biographical characteristics were analysed using Chi-Square tests. Because of the skewed nature of the data, Mann–Whitney U tests were used to test for differences between the ToF + ICD group versus both control groups on all questionnaires. Comparison with normative data was made using Students’ t tests, since raw data for the norm groups were not available, and only mean and standard deviations were available. Descriptive statistics of continuous variables are expressed as medians with quartiles. Stepwise multiple regression was used to correct for age at implantation, and the higher age in the ICD group. The data were analysed using the statistical package SPSS PSAW 17.0.2 ENG for Windows, Release 17.0.2 (Mar 11, 2009).
Results
Population characteristics
Biographical characteristics
The main biographical and medical characteristics for the three groups are outlined in Table 1. No differences in gender were found between the three groups. Patients from the ToF + ICD group were living significantly less often on their own compared to patients from the ICD group. Patients in the ToF + ICD group more often had no relationship and were less often widowed than the older ICD patients. After adjusting for higher age at implantation in the ICD group, it appeared that this variable did not have an effect on the SF-36 results.
No significant differences were found between the three groups with respect to occupational level or educational attainment. In all three groups, the majority had an average educational attainment.
Medical characteristics
No significant difference was found regarding age, the amount of surgical procedures or re-operations between the ToF + ICD and the ToF group. As we selected older ICD patients to represent the “normal” ICD population as our second control group, the patients in the ToF + ICD group were younger than those in the ICD group. Also, patients in the ToF + ICD group were (as planned) significantly older at the time of surgical Fallot correction than patients from the ToF group. Both indication for ICD implantation (primary and secondary) and follow-up time after ICD did not differ between the two groups. The majority of patients in the ICD group were NYHA class II resulting in a significant difference with regard to the ToF + ICD group and the ToF group (majority NYHA class I). When comparing QRS duration, a significant difference was found between all three groups. Group ToF + ICD had the highest QRS duration (176 ms) followed by the ToF group (150 ms) and the ICD group (138 ms). No difference was found between the ToF + ICD and ToF groups when comparing right ventricular dilatation. Right ventricular function was significantly worse in the ToF + ICD group compared to the ToF group (p < 0.01). Remarkably, patients from the ToF + ICD group less often had severe pulmonary regurgitation compared to patients form the ToF group. When analyzing the occurrence of appropriate and inappropriate shocks, a significantly higher incidence of inappropriate shocks was observed in the ToF + ICD group versus the ICD group (p = 0.03). Also, the absolute number of inappropriate shocks was higher in the ToF + ICD group (p = 0.03) and also the amount of appropriate shocks was higher in the ToF + ICD group (p = 0.03).
Scores on instruments (see Table 2)
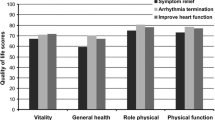
Subjective health status (SF36)
On all SF-36 scales except for one, the median for the ToF + ICD group was lower, indicating more unfavourable outcomes, than for the ToF group. Two significant group effects between the ToF + ICD group versus the ToF group were found: patients from the ToF + ICD group scored significantly lower on physical functioning compared to the ToF group (p = 0.01) and also on general health perceptions patients from the ToF + ICD group scored significantly lower than the ToF group (p < 0.01). When comparing the ToF + ICD versus the ICD group, one significant group effect was found. On physical functioning the ToF + ICD group obtained a higher, more favourable mean score than the ICD group (p = 0.01). No other significant differences were found between the three groups.
Satisfaction with Life Scale
Patients of the ToF + ICD group scored significantly lower compared to patients from the ToF group (p = 0.02). Also, a significantly lower score was found in the ToF + ICD group compared to the ICD group (p = 0.03).
Linear Analogue Scale Quality of Life
The ToF + ICD group showed a trend towards a less favourable result than the ToF group (p = 0.06).
Hospital Anxiety and Depression Scale
Patients from the ToF + ICD group reported significantly more anxiety than patients from the ICD group (p = 0.01). No other significant differences were found on the anxiety and depression scale between the three groups.
Utrecht Coping List
Patients from the ToF + ICD group scored significantly higher on Palliative reactions (i.e. seeking diversion in unhealthy manners) compared to patients from the ICD group (p < 0.01). Also significantly higher scores were found on seeking social support in the ToF + ICD group compared to the ICD group (p < 0.0001). Patients from the ToF + ICD group also scored higher on expressions of (negative) emotions compared to the ICD-patients group (p = 0.01). No differences in scores were found between the ToF + ICD and the ToF group. No other significant differences were found on the other scales of the UCL.
Implanted Devices Adjustment Scale
No significant differences were found between the two ICD groups on any of the IDAS domains.
Perceived Social Support Scale
No significant differences were found between the three groups on any of the PSSS12 domains.
Primary versus secondary indication for ICD implantation
In order to assess whether the indication for ICD implantation had effect on the outcomes, we compared the scores on different scales of patients with a primary indication versus a secondary indication for ICD implantation.
In the ToF + ICD group, no significant differences were found between the two indication groups.
In the ICD group, no significant differences were found between the two indication groups, except for the body awareness scale of the IDAS. Here, patients with a secondary indication showed less favourable outcome.
When combining the ToF + ICD group with the ICD group, a less favourable outcome on the UCL scale in palliative reactions was observed for patients with secondary indication for ICD.
Normative data
When comparing the ToF + ICD group with normative data, the following results were obtained.
Subjective health status (SF36)
Normative data for the Dutch population were obtained from Aaronson et al. [12]. Patients from the ToF + ICD group obtained significantly lower results on physical functioning, social functioning, role limitations due to physical functioning, general mental health, vitality and general health perceptions. No significant difference on the SF-36 scales bodily pain and role limitations due to emotional functioning were found.
Satisfaction with Life Scale
Normative data were obtained from Moons et al. [13]. Patients from the ToF + ICD group obtained significantly less favourable outcomes compared to the general Belgium population.
Linear Analogue Scale Quality of Life
Normative data were obtained from Moons et al. [13]. No significant differences were found between the ToF + ICD group compared to the normative data.
Hospital Anxiety and Depression Scale
Normative data for the HADS have been obtained from Spinhoven et al. [14]. When comparing the ToF + ICD group with normative data, no significant differences were found.
Utrecht Coping List
Normative data for the Dutch population were obtained from Schreurs et al. [16]. Patients from the ToF + ICD group obtained significantly less favourable outcomes on palliative reactions and seeking social support.
Discussion
The main finding of this study is that ToF-patients with an ICD show less favourable psychosocial functioning compared to ToF-patients without ICD and to the older acquired heart disease ICD-patients.
To our knowledge, this is the first psychosocial study carried out in this specific group, Fallot-patients with ICD. Data were compared with two control groups: Fallot-patients without ICD and older “regular” ICD-patients without ConHD. Clinically relevant areas of psychosocial functioning together with medical correlates for psychosocial outcomes were investigated, using standardized and validated questionnaires.
Psychosocial functioning and ICD therapy
Despite a younger age (40 vs. 72 years) and lower NYHA class (I vs. II), Fallot-patients with ICD scored less favourable on instruments assessing subjective health status, anxiety, satisfaction with life and coping (more negative emotions, more palliative reactions such as smoking and drinking and less seeking of social support) compared to older ICD-patients. After correction for the higher age in the ICD group using stepwise multiple regression, all conclusions drawn remained the same.
In contrast to the overall good quality of life reported before [13], in our study we found that Fallot-patients with ICD showed a less favourable quality of life outcome than Fallot-patients without ICD. Our findings, together with the findings from literature indicate that the ConHD background of these ICD-patients cannot be the sole reason for the lower quality of life observed in this study. In fact, they confirm our hypothesis that ICD therapy in young ConHD patients is associated with worse psychosocial functioning. Between the study of Yap et al. [4] and the start of our own study, patients with less favourable medical outcome have died in the ToF + ICD group. This means that it might even be possible that our present outcomes could have been worse as we face a positive selection of patients.
Anxiety in Fallot-patients receiving ICD therapy
We found anxiety to be a problematic psychosocial reaction for young Fallot-patients receiving ICD therapy. This is in line with the review of Sears et al. 2009 [19]. Our results on anxiety were statistically significant and in addition clear trends were observed in the other data, also pointing towards the same direction of a less favourable psychological outcome for Fallot-patients with ICD compared to both control groups. In addition, patients reported a lower satisfaction with life.
In literature [20], a clinical cut-off value of 8 is considered clinically significant on the anxiety scale of the HADS. Our ToF + ICD group obtained a median score of 6 and did not show a significant difference on anxiety level compared to normative data. This finding might be explained by assuming that the HADS instrument may not be sensitive enough to screen for disease-specific anxiety in this unique ConHD population. We assume that using a clinical interview, high levels of anxiety might have been found, as in the article of Bromberg et al. [21].
Role of appropriate and inappropriate ICD shocks
The present data show that Fallot-patients receiving ICD therapy have a higher rate of inappropriate ICD discharges compared to “regular” ICD-patients. Despite optimal programing, 39% of the Fallot-patients with ICD suffered from one or more inappropriate ICD shocks. The inappropriate shock rate was higher than reported in previous studies in non-ConHD patients [3, 5]. Since Fallot-patients are known to have a high arrhythmia burden, the inappropriate shocks we found may be due to atrial arrhythmias [4, 22–24].
Furthermore, ToF ICD-patients are in general younger than the traditional ICD-patient group and tend to lead more active lives, practising sports and other leisure activities. These activities inducing sinus tachycardia may result in inappropriate ICD therapy. Not only the inappropriate shock rate in ToF + ICD patients was higher than that in the older ICD group but also the number of inappropriate shocks per patient was significantly higher. As most inappropriate shocks occur when the patient is fully conscious, this may have serious psychosocial consequences and it may lead to serious anxiety and stress, possibly resulting in avoidance behaviour. Our findings are in line with Vasquez et al. [7], who showed that ICD patients who had a history of more inappropriate shocks with age below 50 and female gender were at higher risk for developing psychosocial problems. Moreover, avoidance behaviour has been reported for ICD patients, which may be a limiting factor in social and sexual activities, but also in practising sports. Out of fear for an ICD discharge, 39% of the ICD-patients avoid physical exertion [25], even though physical exercise is well known to have a beneficial effect on health and can be effective in preventing depression.
Although there is lack of evidence in mortality benefit, the threshold for using ICD therapy in ConHD patients seems to have lowered over time. The guidelines for ICD implantation in this patient population are based on limited data. With the high rate of inappropriate shocks, balancing the benefit-risk ratio for ICD implantation remains difficult, especially taking psychosocial problems into account.
Medical background
The differences in QRS duration as seen in Table 1 could be explained by the ConHD background in combination with pacemaker therapy differences between groups. ToF-patients have a higher QRS duration as a result of right ventricular dilatation, diminished function, or post-surgery for their ConHD background. Some of the patients in the ToF + ICD group also received constant pacing therapy next to the ICD therapy which may also have resulted into a longer QRS duration. The long QRS duration seen in the ToF + ICD group can also be the result of selection, as a QRS duration >180 ms is a predictor for SCD and may have been used as a criterium for ICD implantation [26]. Despite the diminished RV function, patients in the ToF + ICD group were in good clinical condition with the majority being in NYHA class I.
Clinical implications
When considering ICD therapy in young patients, the psychosocial impact should be taken into account. The findings in this study provide a solid argument for careful assessment and counselling in patients with Tetralogy of Fallot. The threshold for ICD implantation should be high, especially in case of primary prevention. In patients needing an ICD, routinely applied comprehensive and multidisciplinary psychosocial aftercare is advised. We see an opportunity for a shared decision-making model in this situation. In this way, patients can become well informed about all possible consequences of ICD therapy, and can decide the best treatment option together with the clinician.
In order to facilitate acceptance of ICD therapy, we recommend cognitive behavioural techniques such as psycho-education, cognitive re-appraisal and relaxation techniques to improve quality of life of these patients. These techniques have been found to improve the quality of life in the “general” older ICD population [7, 27, 28].
Limitations
The patients included in this study were all followed in a tertiary (academic) medical centre. Therefore, this study may not be representative for all Fallot-patients. In addition, although we tried to create comparable groups, some differences were present. Furthermore, because of the small sample size, often encountered in these patient groups, several nearly significant trends were observed. With a larger sample size these trends might have become significant.
Although no significant differences were found between the three groups, a trend was visible in which the older ICD patients more often had male gender.
Unfortunately, data regarding psychosocial interventions (so called “medical consumption” or “psychotherapeutic counselling”) are not systematically available.
Furthermore, as could be expected, a significant age difference was found between the ToF + ICD and the—by definition—older ICD group, which resulted in a later age at implantation in the ICD group. In addition, patients with the Belgian nationality (N = 8) were only found in the ToF + ICD group. To which extent these inter-group differences have influenced our results is unknown.
Despite the fact that patients in the ICD group were more often in NYHA class II compared to the ToF and the ToF + ICD group, we remarkably found that our younger NYHA class I ToF + ICD patients obtained less favourable results than the other ICD group with worse NYHA class. This noteworthy finding reflects the psychosocial importance of our results in the ToF + ICD group.
Future research
Future research should investigate the role of inappropriate shocks on psychosocial outcome in a larger cohort, as the current cohort was not large enough to perform further subanalyses. In addition, the impact of ICD therapy in young adults with ConHD on activities such as practising sports, sexuality and driving a car [29] should be studied. We recommend using a semi-structured clinical interview to assess these points, as questionnaires may not be specific enough.
Different programing strategies, such as the application of antitachycardia pacing therapy and higher rate cut-offs for arrhythmia detection, may prevent inappropriate ICD therapy and may have a beneficial effect on psychosocial functioning.
Recently, the subcutane ICD (sICD) has been introduced for patients requiring ICD therapy [30, 31]. In this study, sICD therapy appeared to have a very low rate of inappropriate shocks. This therefore may be a good alternative for ConHD patients who require ICD therapy and suffer from a lot of inappropriate shocks. The sICD is relatively easy to implant, and because the leads are subcutaneous, replacement and complication rates appear to be lower as well. Future research could concentrate on the application and psychosocial impact of having an sICD in ConHD patients.
Conclusion
Implantable cardioverter defibrillators implantation has a major psychosocial impact in young adults with ToF. This group shows clinically significant psychosocial problems that have to be recognized and treated appropriately. The information obtained from this study can be used to guide adequate counselling and development of interventions aimed at enhancing psychosocial functioning and improving quality of life. Our results provided information that is not readily apparent from routine clinical investigations.
References
Oechslin EN, Harrison DA, Connelly MS, Webb GD, Siu SC (2000) Mode of death in adults with congenital heart disease. Am J Cardiol 86(10):1111–1116
Silka MJ, Hardy BG, Menashe VD, Morris CD (1998) A population-based prospective evaluation of risk of sudden cardiac death after operation for common congenital heart defects. J Am Coll Cardiol 32(1):245–251
Khairy P, Harris L, Landzberg MJ, Viswanathan S, Barlow A, Gatzoulis MA, Fernandes SM, Beauchesne L, Therrien J, Chetaille P, Gordon E, Vonder Muhll I, Cecchin F (2008) Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation 117(3):363–370
Yap SC, Roos-Hesselink JW, Hoendermis ES, Budts W, Vliegen HW, Mulder BJ, van Dijk AP, Schalij MJ, Drenthen W (2007) Outcome of implantable cardioverter defibrillators in adults with congenital heart disease: a multi-centre study. Eur Heart J 28(15):1854–1861
Alexander ME, Cecchin F, Walsh EP, Triedman JK, Bevilacqua LM, Berul CI (2004) Implications of implantable cardioverter defibrillator therapy in congenital heart disease and pediatrics. J Cardiovasc Electrophysiol 15(1):72–76
Sears SF Jr, Todaro JF, Lewis TS, Sotile W, Conti JB (1999) Examining the psychosocial impact of implantable cardioverter defibrillators: a literature review. Clin Cardiol 22(7):481–489
Vazquez LD, Conti JB, Sears SF (2010) Female-specific education, management, and lifestyle enhancement for implantable cardioverter defibrillator patients: the FEMALE-ICD study. Pacing Clin Electrophysiol 33(9):1131–1140
Sowell LV, Sears SF Jr, Walker RL, Kuhl EA, Conti JB (2007) Anxiety and marital adjustment in patients with implantable cardioverter defibrillator and their spouses. J Cardiopulm Rehabil Prev 27(1):46–49
van der Velde ET, Vriend JW, Mannens MM, Uiterwaal CS, Brand R, Mulder BJ (2005) CONCOR, an initiative towards a national registry and DNA-bank of patients with congenital heart disease in the Netherlands: rationale, design, and first results. Eur J Epidemiol 20(6):549–557
Utens EMWJ, van Rijen EHM, Erdman RAM, Verhulst FC 2000. Rotterdams Kwaliteit van Leven—Interview
Ware JE Jr (1992) Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MA, te Velde A, Verrips E (1998) Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 51(11):1055–1068
Moons P, Van Deyk K, De Bleser L, Marquet K, Raes E, De Geest S, Budts W (2006) Quality of life and health status in adults with congenital heart disease: a direct comparison with healthy counterparts. Eur J Cardiovasc Prev Rehabil 13(3):407–413
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM (1997) A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 27(2):363–370
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Schreurs PJG, van de Willige G, Brosschot JF, Tellegen B, Graus GMH (1993) De Utrechtse Coping Lijst: UCL, omgaan met problemen en gebeurtenissen, herziene handleiding 1993
Beery TA, Baas LS, Matthews H, Burroughs J, Henthorn R (2005) Development of the implanted devices adjustment scale. Dimens Crit Care Nurs 24(5):242–248
Pedersen SS, van Domburg RT, Theuns DA, Jordaens L, Erdman RA (2004) Type D personality is associated with increased anxiety and depressive symptoms in patients with an implantable cardioverter defibrillator and their partners. Psychosom Med 66(5):714–719
Sears SF, Matchett M, Conti JB (2009) Effective management of ICD patient psychosocial issues and patient critical events. J Cardiovasc Electrophysiol 20(11):1297–1304
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 52(2):69–77
Bromberg JI, Beasley PJ, D’Angelo EJ, Landzberg M, DeMaso DR (2003) Depression and anxiety in adults with congenital heart disease: a pilot study. Heart Lung 32(2):105–110
Khairy P, Aboulhosn J, Gurvitz MZ, Opotowsky AR, Mongeon FP, Kay J, Valente AM, Earing MG, Lui G, Gersony DR, Cook S, Ting JG, Nickolaus MJ, Webb G, Landzberg MJ, Broberg CS (2010) Arrhythmia burden in adults with surgically repaired tetralogy of Fallot: a multi-institutional study. Circulation 122(9):868–875
Roos-Hesselink J, Perlroth MG, McGhie J, Spitaels S (1995) Atrial arrhythmias in adults after repair of tetralogy of Fallot. Correlations with clinical, exercise, and echocardiographic findings. Circulation 91(8):2214–2219
Magnin-Poull I, De Chillou C, Miljoen H, Andronache M, Aliot E (2005) Mechanisms of right atrial tachycardia occurring late after surgical closure of atrial septal defects. J Cardiovasc Electrophysiol 16(7):681–687
Lemon J, Edelman S, Kirkness A (2004) Avoidance behaviors in patients with implantable cardioverter defibrillators. Heart Lung 33(3):176–182
Gatzoulis MA, Till JA, Somerville J, Redington AN (1995) Mechanoelectrical interaction in tetralogy of Fallot. QRS prolongation relates to right ventricular size and predicts malignant ventricular arrhythmias and sudden death. Circulation 92(2):231–237
Pedersen SS, van den Broek KC, Sears SF Jr (2007) Psychological intervention following implantation of an implantable defibrillator: a review and future recommendations. Pacing Clin Electrophysiol 30(12):1546–1554
Irvine J, Firestone J, Ong L, Cribbie R, Dorian P, Harris L, Ritvo P, Katz J, Newman D, Cameron D, Johnson S, Bilanovic A, Hill A, O’Donnell S, Sears S Jr (2011) A randomized controlled trial of cognitive behavior therapy tailored to psychological adaptation to an implantable cardioverter defibrillator. Psychosom Med 73(3):226–233
Groeneveld PW, Matta MA, Suh JJ, Yang F, Shea JA (2007) Quality of life among implantable cardioverter-defibrillator recipients in the primary prevention therapeutic era. Pacing Clin Electrophysiol 30(4):463–471
Bardy GH, Smith WM, Hood MA, Crozier IG, Melton IC, Jordaens L, Theuns D, Park RE, Wright DJ, Connelly DT, Fynn SP, Murgatroyd FD, Sperzel J, Neuzner J, Spitzer SG, Ardashev AV, Oduro A, Boersma L, Maass AH, Van Gelder IC, Wilde AA, van Dessel PF, Knops RE, Barr CS, Lupo P, Cappato R, Grace AA (2010) An entirely subcutaneous implantable cardioverter-defibrillator. N Engl J Med 363(1):36–44
Dabiri Abkenari L, Theuns DA, Valk SD, Van Belle Y, de Groot NM, Haitsma D, Muskens-Heemskerk A, Szili-Torok T, Jordaens L (2011) Clinical experience with a novel subcutaneous implantable defibrillator system in a single center. Clin Res Cardiol 100(9):737–744
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Opić, P., Utens, E.M.W.J., Moons, P. et al. Psychosocial impact of implantable cardioverter defibrillators (ICD) in young adults with Tetralogy of Fallot. Clin Res Cardiol 101, 509–519 (2012). https://doi.org/10.1007/s00392-012-0420-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0420-x