Abstract
Somatic mutations in the isocitrate dehydrogenase 1 gene (IDH1) occur at high frequency in gliomas and seem to be a prognostic factor for survival in glioblastoma patients. In our set of 98 glioblastoma patients, IDH1 R132 mutations were associated with improved survival of 1 year on average, after correcting for age and other variables with Cox proportional hazards models. Patients with IDH1 mutations were on average 17 years younger than patients without mutation. Mutated IDH1 has a gain of function to produce 2-hydroxyglutarate by NADPH-dependent reduction of α-ketoglutarate, but it is unknown whether NADPH production in gliomas is affected by IDH1 mutations. We assessed the effect of IDH1 R132 mutations on IDH-mediated NADPH production in glioblastomas in situ. Metabolic mapping and image analysis was applied to 51 glioblastoma samples of which 16 carried an IDH1 R132 mutation. NADP+-dependent IDH activity was determined in comparison with activity of NAD+-dependent IDH and all other NADPH-producing dehydrogenases, glucose-6-phosphate dehydrogenase, 6-phosphogluconate dehydrogenase, malate dehydrogenase, and hexose-6-phosphate dehydrogenase. The occurrence of IDH1 mutations correlated with approx. twofold diminished NADP+-dependent IDH activity, whereas activity of NAD+-dependent IDH and the other NADP+-dependent dehydrogenases was not affected in situ in glioblastoma. The total NADPH production capacity in glioblastoma was provided for 65% by IDH activity and the occurrence of IDH1 R132 mutation reduced this capacity by 38%. It is concluded that NADPH production is hampered in glioblastoma with IDH1 R132 mutation. Moreover, mutated IDH1 consumes rather than produces NADPH, thus likely lowering NADPH levels even further. The low NADPH levels may sensitize glioblastoma to irradiation and chemotherapy, thus explaining the prolonged survival of patients with mutated glioblastoma.
Similar content being viewed by others
Introduction
Primary and secondary glioblastomas display somatic mutations in the IDH1 gene. The mutation is relatively rare in primary glioblastoma (approx. 5% of the tumors harbor the mutation) and frequent in secondary glioblastoma (70–80% of the tumors carry the mutation [3, 5, 10, 12, 19, 21, 24, 25, 32–34, 36]). IDH1 encodes for NADP+-dependent isocitrate dehydrogenase 1, which can be found in cytoplasm, peroxisomes [9] and endoplasmic reticulum [18] and belongs to a gene family encompassing five members [9, 18]. Wild-type IDH1 catalyzes the oxidative decarboxylation of isocitrate to α-ketoglutarate [15] with concomitant production of NADPH. Mutations in IDH1 are tumor specific and have so far been detected in various types of gliomas, especially in those histologically classified as low-grade gliomas and secondary glioblastoma [3, 5, 10, 12, 19, 21, 24, 32, 33, 36] and in a subset of acute myeloid leukemia [17]. Mutations affecting the isocitrate dehydrogenase 2 gene (IDH2), another NADP+-dependent IDH localized in mitochondria, have also been described in gliomas although at lower frequency [10, 25, 36]. The other three members of the IDH family are exclusively localized in mitochondria, depend on NAD+ for their enzymatic activity and play a relevant role in the Krebs cycle [37]. These NAD+-dependent IDHs are not known to be mutated in relation to gliomagenesis.
The mutational profile of IDH1 and IDH2 is peculiar as the mutations affect only single evolutionarily conserved residues (arginines R132 and R172, respectively). The arginines are localized in the substrate binding site of the isozymes, where hydrophilic interactions between the arginine and both α- and β-carboxylate of isocitrate are formed [35]. Interestingly, from a genetic perspective the pattern of IDH1 mutations is consistent with a gain of function (such as those occurring in oncogenes). However, it has been shown that the mutations inactivate the standard enzymatic activity of IDH1 and IDH2 [12, 36]. As a consequence, α-ketoglutarate levels are reduced when IDH1 is mutated. α-Ketoglutarate in the cytoplasm initiates oxygen-dependent degradation of hypoxia-inducible factor subunit HIF-1α [22, 27, 38]. Thus, decreased cytoplasmic levels of α-ketoglutarate increase levels of HIF-1α and the heterodimer HIF-1 consisting of HIF-1α and HIF-1β is transported into the nucleus for transcriptional activity [11, 22, 27]. HIF-1 is the master switch of cellular adaptation to low oxygen tension and induces transcription of genes involved in angiogenesis, cell motility and invasion and energy metabolism [11]. Furthermore, a recent report has shown that mutated IDH1 does not convert isocitrate and NADP+ into α-ketoglutarate and NADPH but rather has a gain of function enabling IDH1 to convert α-ketoglutarate and NADPH into 2-hydroxyglutarate and NADP+ [8]. It was shown that glioma samples with the IDH1 mutation contained high 2-hydroxyglutarate levels [8]. Interestingly, in patients with 2-hydroxyglutarate dehydrogenase deficiency, 2-hydroxyglutarate accumulation is associated with a higher risk of malignant brain tumors [1].
How the IDH1 R132 mutations affect NADPH production in human tumors is presently unknown and is a matter of debate [22, 27]. NADPH plays an important role in detoxification processes and scavenging of oxygen radicals [14] and thus is a protective compound in cancer cells under stress during irradiation or chemotherapy.
In the present study, we correlated the occurrence of IDH1 R132 mutations with overall survival of glioblastoma patients using multivariable analysis. Furthermore, we applied metabolic mapping and image analysis to assess the NADP+-dependent and NAD+-dependent enzymatic activity of IDH in comparison with the activity of all other NADPH-producing dehydrogenases [30] in glioblastoma in situ. This strategy was then exploited to correlate the IDH1 mutational status with its enzymatic activity.
Materials and methods
Tumor samples, isolation of DNA, PCR, sequencing and mutation analysis
DNA samples of 109 frozen glioblastomas, for which the mutational status of IDH1 was previously determined [5], were obtained from the tumor bank maintained by the Departments of Neurosurgery and Neuropathology at the Academic Medical Center (Amsterdam, The Netherlands). In the present study, these glioblastoma samples were analyzed for IDH2 mutations, and a subset of these samples was used for survival analysis and enzyme activity. Use of material was waived by our local ethics committee, as it fell under the Dutch Code of proper secondary use of human tissue. The research was performed on ‘waste’ material, stored in a coded fashion.
Tumor samples were included only if at least 80% of the sample consisted of cancer cells, as verified by H&E staining. Genomic DNA was isolated as previously described [2]. PCR, sequencing and mutation analysis details have been described previously [5].
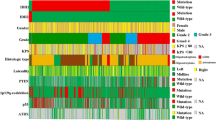
Glioblastoma patient data
A retrospective survival analysis was performed for 98 glioblastoma patients with known follow-up. Both primary (85) and secondary glioblastoma (13), but no recurrent glioblastoma patients were included. These patients underwent brain surgery at the AMC between 1988 and 2006 and were selected, when enough tissue was available to perform the experiments described. Patient characteristics are displayed in Table 1. The primary end point of this analysis was overall survival, calculated as time from surgery to death. Events were censored if the patient was alive at the time of last follow-up. Follow-up for patients ranged from 15 to 2,722 days. The median overall survival was 262 days; the 2-year survival rate was 15%. Patients have been treated with different regimens either in trials or with standard protocols. Other therapies in addition to irradiation included chemoradiation (radiotherapy with concomitant and adjuvant temodal), brachytherapy, gliadel, PCV, temodal, MTX and nicotinamine (an enhancer during irradiation).
Metabolic mapping
Glioblastoma and normal brain tissue were snap-frozen in liquid nitrogen in the operating room, and stored at −80°C until used. Normal brain sections contained both grey and white matter. Six-μm-thick cryostat sections were cut at −25°C on a HM560 cryostat (MICROM, Walldorf, Germany), picked up on glass slides, and stored at −80°C until used [30]. Cryostat sections of glioblastoma tissue were allowed to dry at room temperature for 5 min and were then incubated for the demonstration of IDH, G6PDH, 6PGDH, MDH and H6PDH activity [26, 29]. Incubation media contained 18% polyvinyl alcohol (PVA, average molecular mass 70,000–100,000; Sigma, St. Louis, MO) in 0.1 M phosphate buffer, pH 7.4, 0.32 mM 1-methoxyphenazine methosulfate (Serva, Heidelberg, Germany), 5 mM sodium azide, 5 mM MgCl2, 5 mM nitro BT (Sigma), and either 20 mM d,l-isocitrate (Sigma) or 10 mM glucose-6-phosphate (Serva), or 10 mM 6-phosphogluconate (Sigma), or 100 mM malate (Serva), or 10 mM galactose-6-phosphate (Sigma) to demonstrate activity of IDH, G6PDH, 6PGDH, MDH, or H6PDH, respectively. For NADP+-dependent dehydrogenases, 0.8 mM NADP+ (Roche, Mannheim, Germany) was used as co-enzyme, whereas for the NAD+-dependent IDH activity, 4 mM NAD+ (Roche) was used. The concentrations of the substrates and co-enzymes in the incubation media were sufficiently high to ensure maximum velocity (V max) of the enzyme activities [26, 28]. Negative control reactions were performed in the absence of substrate [6]. The media were freshly prepared just before incubation and nitro BT was added after being dissolved in a heated mixture of dimethylformamide and ethanol (final dilution of each solvent in the medium was 2% v/v). For the demonstration of both NAD+- and NADP+-dependent IDH activity, sections were incubated for 45 min at 37°C. For activity of G6PDH, 6PGDH, MDH and H6PDH sections were incubated for 30, 10, 45, and 45 min, respectively at 37°C. Sections were then rinsed with hot phosphate buffer (0.1 M, pH 5.3, 65°C) to remove the incubation medium and to immediately stop the reaction. Afterwards, sections were embedded in glycerol jelly.
Image analysis
The final reaction product of dehydrogenase activity (nitro BT-formazan) was analyzed with the use of quantitative image analysis, using a Vanox-T photomicroscope with a 10× objective (Olympus, Tokyo, Japan) and a CFW-1312M 1,360 × 1,024 pixel 10-bit monochrome FireWire camera (Scion, Tucson, AZ) mounted on the front port of the Vanox using adapting optics. Sections were illuminated with white light that was filtered by a monochromatic filter of 585 nm and an infrared blocking filter [7] to correctly measure the absorbance of both mono- and di-formazans [26, 29]. Absorbance calibration of the images was performed with the use of a calibrated 10-step density tablet (Stouffer, South Bend, IN). After measuring the step tablet, known absorbance values were related to measured grey values using the built-in calibration function of ImageJ, using the Rodbard function. Density calibrated images were recorded in one single run and stored on disk for analysis. The resolution used prevented distributional errors [7]. All settings were maintained throughout the recording session and at the end of the session verified against the step tablet values. Software used for capturing was swf-image, a Scion proprietary camera driver, as an extension to the image processing application ImageJ, developed by Wayne Rasband [23]. ObjectJ, a plugin for non-destructive image marking and result linking developed by Norbert Vischer and Stelian Nastase at the Department of Biology of the University of Amsterdam [31], was used to indicate regions of interest (ROI) that were measured. Using the ObjectJ plugin, mean absorbance values within the ROI were collected from the test reaction and the control reaction, allowing calculation of specific activity of IDHs, G6PDH, 6PGDH, MDH and H6PDH, respectively [29]. Activity was expressed as micromoles NADPH produced per milliliter of tissue/min. The use of ObjectJ allows a retrospective quality control study of areas measured.
Statistical analysis
Statistical processing of data was performed using Excel 2002 (Microsoft, San Jose, CA) and SPSS 16.02 for Windows (SPSS, Chicago, IL). Associations between the different dehydrogenase activities and IDH1 mutations were assessed by t test. The association between IDH1 mutations or NADP+-dependent IDH activity and survival time was tested with Cox proportional hazard models. After the individual tests, factors with P values less than 0.10 were included in the multivariable Cox model to determine the factors associated with survival time (Table 2).
Results
Mutational profiling of IDH1 and IDH2 in glioblastoma
A panel of 109 glioblastoma (94 primary and 15 secondary) for which the prevalence of IDH1 R132 mutations had already been assessed [5] was also analyzed for IDH2 mutations. No somatic IDH2 mutations were observed in this set of tumors.
Mutation at IDH1 R132 is an independent prognostic factor for improved survival in glioblastoma patients
In a subset of 98 glioblastoma with known follow-up, the overall survival of both primary and secondary glioblastoma was increased for patients whose tumors carried an IDH1 mutation (P = 0.002, log rank test). Moreover, patients without mutation were on average 58 years old, whereas patients with mutation were 41 years old. When corrected for age, Karnofsky performance status (KPS), extent of surgery, received dosage of radiotherapy, additional chemotherapy or treatment other than radiotherapy (Table 2), the mutational status of IDH1 R132 was a strong independent prognostic factor for improved overall survival (P < 0.001; Fig. 1; Table 2). This significant association indicates that the presence of IDH1 mutation correlates with an improved prognosis for glioblastoma patients which is in agreement with other studies [19, 24, 25, 34].
IDH1R132 mutations are associated with diminished in situ NADP+-dependent IDH activity in glioblastoma cells
Activity of NADP+-dependent IDH was determined in glioblastoma cryostat sections of tumor samples of 51 glioblastoma patients (Fig. 2) to evaluate whether and to what extent IDH1 mutations affect the metabolic status of glioblastoma cells. These 51 tumor samples included 15 tumor samples mutated at IDH1 R132, of these, 12 contained the R132H mutation, two the R132C mutation and one sample the R132G mutation (Fig. 3b). Activity was heterogeneous within tumor samples (Fig. 2c). As this could be associated with the presence of necrosis, the regions analyzed were ‘validated’ by H&E staining of adjacent sections to contain vital tumor tissue (Fig. 2b, d). Representative areas with the most uniform activity of each section were selected to measure the enzyme activity. Of note, no activity was observed in regions of necrosis.
NADP+-dependent IDH activity in IDH1 R132 non-mutated (n = 36) and mutated (n = 15) tumors. NADP+-dependent IDH activity staining of IDH1 R132 non-mutated a and mutated c glioblastoma cryostat sections. The amount of blue color (nitro BT-formazan) directly reflects NADP+-dependent IDH activity (production of NADPH). H&E staining of serial sections of non-mutated (b) and mutated (d) samples
Capacity (maximum velocity; V max) of dehydrogenases in IDHR132 non-mutated and mutated tumors expressed as micromoles NADPH or NADH produced/ml of tissue/min, ±SD. NADP+-dependent IDH activity (a); individual values of NADP+-dependent IDH activity (b); NADP+-dependent G6PD activity (c); NAD+-dependent IDH activity (d)
Next, we correlated the mutational status of IDH1 with the quantitative data of NADP+-dependent IDH activity (Fig. 3a). The presence of IDH1 mutations was inversely associated with NADP+-dependent IDH activity (P = 0.001). The individual NADP+-dependent IDH activity values are shown in Fig. 3b. Activity varied strongly among tumors; nevertheless, we observed a twofold reduction in activity.
As a control, the activity of NADP+-dependent G6PDH and NAD+-dependent IDH was assessed on serial sections of the same samples. IDH1 mutations were not associated with NADP+-dependent G6PDH activity (P = 0.60; Fig. 3c) or with NAD+-dependent IDH activity (P = 0.639; Fig. 3d), indicating that the correlation with IDH1 mutations is specific for the NADP+-dependent IDH activity.
Table 3 shows that IDH had the largest capacity to generate NADPH in normal brain, wild-type glioblastoma and IDH1-mutated glioblastoma. Sixty-five % of the NADPH-producing capacity was provided by IDH. The total NADPH-generating capacity was significantly reduced by 38% by the IDH1 R132 mutation (P = 0.02; Table 3). For this experiment, a subset of 13 wild-type tumor samples, 13 tumor samples mutated at IDH1R132 and 5 samples of normal brain were used. Again, the difference between NADP+-dependent IDH activity in non-mutated and mutated tumor samples was significant (P = 0.01).
The combination of our findings indicates that IDH1 mutations are associated with improved survival in glioblastoma and that IDH1 mutated glioblastoma samples have a lower NADPH-producing capacity, thus suggesting that diminished NADPH formation correlates with improved survival. In 43 glioblastoma patients, lower NADP+-dependent IDH activity appeared to be correlated with improved survival. However, the correlation was not significant (hazard ratio: 1.108 μmoles NADPH produced/ml of tissue/min; CI 0.880–1.394; P = 0.38), probably due to the limited size of the examined cohort.
Discussion
A high percentage of human gliomas has been found to harbour mutations in the metabolic enzyme IDH1. We confirm here the previously reported findings that IDH1 mutations are predominantly found in secondary glioblastoma and in younger patients (Table 1) [5, 10, 19, 24, 25, 32, 34] and that IDH1 mutations correlate independently with improved prognosis in glioblastoma patients (Table 2; Fig. 1).
When IDH1 and IDH2 mutations are ectopically (over)expressed in human cells, they reduce NADP+-dependent IDH activity [12, 36]. Thus far, nothing was known about the effect of IDH1 and IDH2 mutations on IDH activity in glioblastoma in situ. In order to shed light on the functional effects of IDH1 mutations, we exploited an integrated approach to measure NADP+-dependent IDH activity in situ on brain tumor samples. Using this strategy, we showed for the first time that IDH1 R132 mutations are associated with on average a twofold decreased NADP+-dependent IDH activity in the tumors. As both IDH1 and IDH2 use NADP+ as a co-factor, we cannot differentiate between the activity of IDH1 and IDH2. However, considering that we did not observe any IDH2 somatic mutations in the samples that we analyzed, our work indicates that the reduced NADP+-dependent IDH activity is associated with the presence of IDH1 mutations. The loss of NADPH production capacity by mutated IDH1 is considerable (38%) because NADP-dependent IDH activity represents 65% of the total capacity (Table 3). As mutated IDH1 consumes rather than produces NADPH [8], the loss of NADPH for scavenging oxygen radicals and detoxification is likely even more profound. It may explain prolonged survival of glioblastoma patients with the IDH1 mutation. NADPH is necessary for biosynthetic processes such as lipogenesis and for detoxification [14]. Low levels of cytoplasmic NADPH result in impaired reduction of glutathione (GSH), which is a major scavenger of oxygen radicals in the cells. Diminished levels of GSH thus lead to oxidative stress that can ultimately cause DNA damage and induce apoptosis [13, 16]. Oxidative stress is generally increased by irradiation and chemotherapy [20], and we speculate that it is further enhanced in the presence of IDH1 mutations. Thus, tumors with the mutation may be less resistant to irradiation and chemotherapy which explains the prolonged survival of patients with mutated tumors. Low levels of cytoplasmic NADPH also affect the thioredoxin system, a family of small redox active proteins that are kept in reduced form by the NADPH-dependent thioredoxin reductase and help to maintain the redox state in cells [4]. Thioredoxins are frequently overexpressed in cancer and play a role in resistance to irradiation and chemotherapy like reduced GSH.
In conclusion, we have shown that IDH1 R132 mutations correlate with diminished NADPH production in situ in glioblastoma and provide an independent survival advantage to glioblastoma patients. This may be explained by a reduced capacity to produce NADPH in combination with NADPH consumption by mutated IDH1 instead of NADPH production by wild-type IDH1. Our data suggest that NADPH metabolism may be therapeutically exploited in gliomas.
References
Aghili M, Zahedi F, Rafiee E (2009) Hydroxyglutaric aciduria and malignant brain tumor: a case report and literature review. J Neurooncol 91:233–236
Balakrishnan A, Bleeker FE, Lamba S et al (2007) Novel somatic and germline mutations in cancer candidate genes in glioblastoma, melanoma, and pancreatic carcinoma. Cancer Res 67:3545–3550
Balss J, Meyer J, Mueller W et al (2008) Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol 116:597–602
Biaglow JE, Miller RA (2005) The thioredoxin reductase/thioredoxin system. Cancer Biol Ther 4:6–13
Bleeker FE, Lamba S, Leenstra S et al (2009) IDH1 mutations at residue p.R132 (IDH1(R132)) occur frequently in high-grade gliomas but not in other solid tumors. Hum Mutat 30:7–11
Butcher RG, Van Noorden CJF (1985) Reaction rate studies of glucose-6-phosphate dehydrogenase activity in sections of rat liver using four tetrazolium salts. Histochem J 17:993–1008
Chieco P, Jonker A, Melchiorri C et al (1994) A user’s guide for avoiding errors in absorbance image cytometry: a review with original experimental observations. Histochem J 26:1–19
Dang L, White DW, Gross S et al (2009) Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 462:739–747
Geisbrecht BV, Gould SJ (1999) The human PICD gene encodes a cytoplasmic and peroxisomal NADP(+)-dependent isocitrate dehydrogenase. J Biol Chem 274:30527–30533
Hartmann C, Meyer J, Balss J et al (2009) Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1,010 diffuse gliomas. Acta Neuropathol 118:469–474
Hughes JM, Groot AJ, Van der Groep P et al (2009) Active HIF-1 in the normal human retina. J Histochem Cytochem PMID 19901273
Ichimura K, Pearson DM, Kocialkowski S et al (2009) IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro Oncol 11:341–347
Kim SY, Lee SM, Tak JK et al (2007) Regulation of singlet oxygen-induced apoptosis by cytosolic NADP+-dependent isocitrate dehydrogenase. Mol Cell Biochem 302:27–34
Koehler A, Van Noorden CJF (2003) Reduced nicotinamide adenine dinucleotide phosphate and the higher incidence of pollution-induced liver cancer in female flounder. Environ Toxicol Chem 22:2703–2710
Koshland DE Jr, Walsh K, LaPorte DC (1985) Sensitivity of metabolic fluxes to covalent control. Curr Top Cell Regul 27:13–22
Lee SM, Park SY, Shin SW et al (2009) Silencing of cytosolic NADP(+)-dependent isocitrate dehydrogenase by small interfering RNA enhances the sensitivity of HeLa cells toward staurosporine. Free Radic Res 43:165–173
Mardis ER, Ding L, Doolong DJ et al (2009) Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med 361:1058–1066
Margittai E, Banhegyi G (2008) Isocitrate dehydrogenase: a NADPH-generating enzyme in the lumen of the endoplasmic reticulum. Arch Biochem Biophys 471:184–190
Nobusawa S, Watanabe T, Kleihues P et al (2009) IDH1 mutations as molecular signature and predictive factor of secondary glioblastomas. Clin Cancer Res 15:6002–6007
Ozben T (2007) Oxidative stress and apoptosis: impact on cancer therapy. J Pharm Sci 96:2181–2196
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321:1807–1812
Pollard PJ, Ratcliffe PJ (2009) Puzzling patterns of predisposition. Science 324:192–194
Rasband WS (2009) ImageJ. http://rsbweb.nih.gov/ij/
Sanson M, Marie Y, Paris S et al (2009) Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol 27:4150–4154
Sonoda Y, Kumabe T, Nakamura T et al (2009) Analysis of IDH1 and IDH2 mutations in Japanese glioma patients. Cancer Sci 100:1996–1998
Stoward P, Van Noorden CJF (1991) Histochemical methods for dehydrogenases. Churchill–Livingstone, Edinburgh
Thompson CB (2009) Metabolic enzymes as oncogenes or tumor suppressors. N Engl J Med 360:813–815
Van Noorden CJF, Butcher RG (1991) Quantitative enzyme histochemistry. Churchill–Livingstone, Edinburgh
Van Noorden CJF, Frederiks WM (1992) Enzyme histochemistry. A laboratory manual of current methods. Oxford Science Publications, Oxford
Van Noorden CJF (2009) Metabolic mapping by enzyme histochemistry in living animals, tissues and cells. J Physiol Pharmacol 60(Suppl 4):125–129
Vischer N, Nastase S (2009) ObjectJ. http://simon.bio.uva.nl/
Watanabe T, Nobusawa S, Kleihues P et al (2009) IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174:1149–1153
Watanabe T, Vital A, Nobusawa S et al (2009) Selective acquisition of IDH1 R132C mutations in astrocytomas associated with Li-Fraumeni syndrome. Acta Neuropathol 117:653–656
Weller M, Felsberg J, Hartmann C et al (2009) Molecular predictors of progression-free and overall survival in patients with newly diagnosed glioblastoma: a prospective translational study of the German glioma network. J Clin Oncol 27:5743–5750
Xu X, Zhao J, Xu Z et al (2004) Structures of human cytosolic NADP-dependent isocitrate dehydrogenase reveal a novel self-regulatory mechanism of activity. J Biol Chem 279:33946–33957
Yan H, Parsons DW, Jin G et al (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360:765–773
Ying W (2008) NAD+/NADH and NADP+/NADPH in cellular functions and cell death: regulation and biological consequences. Antioxid Redox Signal 10:179–206
Zhao S, Lin Y, Xu W et al (2009) Glioma-derived mutations in IDH1 dominantly inhibit IDH1 catalytic activity and induce HIF-1alpha. Science 324:261–265
Acknowledgments
We thank L. Oegema and N. Schmidt for their help with the metabolic mapping and image analysis, A. Zwinderman and N. van Geloven for help with statistical analyses, and F. DiNicolantionio, J. Reijneveld and S. Thorlacius for critical reading of an earlier version of the manuscript. This work was supported by grants from the Italian Association for Cancer Research (AIRC: AB), Italian Ministry of Health, Regione Piemonte (AB), Italian Ministry of University and Research, CRT Progetto Alfieri (AB), and Association for International Cancer Research (AICR-UK: AB) and EU FP6 contract 037297 (AB). F.B. is supported by a Netherlands Genomic Initiative Fellowship.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. E. Bleeker and N. A. Atai contributed equally to the study.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bleeker, F.E., Atai, N.A., Lamba, S. et al. The prognostic IDH1 R132 mutation is associated with reduced NADP+-dependent IDH activity in glioblastoma. Acta Neuropathol 119, 487–494 (2010). https://doi.org/10.1007/s00401-010-0645-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-010-0645-6