Abstract
Chronic alcohol abuse leads to morphological changes of the brain. We investigated if these volumetric changes are reversible after a period of abstinence. For this reason 41 male and 15 female alcohol patients underwent MRI-scanning after in-patient detoxification (baseline) entering alcoholism treatment programs, and between 6 and 9 months later (follow-up), in a phase of convalescence. Additionally, 29 male and 16 female control subjects were examined. The MRI-scans were delineated and the resulting regions of interest, volumes of lateral ventricles and prefrontal lobes were expressed relatively to total brain volume. Compared to control subjects alcohol patients showed bilaterally decreased prefrontal lobes (11% reduction) and increased lateral ventricles (up to 42% enlargement). The extent of the ventricular increase was depending on patient’s additional psychiatric diagnosis, showing smaller lateral ventricles in patients with additional personality disorder. While at follow-up the size of prefrontal lobes remained unchanged, volumes of the lateral ventricles decreased (5–6% reduction) in alcohol patients with abstinence and improved drinking behavior, especially in patients that underwent only one detoxification. The extent of the ventricular enlargement correlated with the elevation of alcohol related laboratory measures (mean corpuscular volume, gamma-glutamyl transpeptidase). In conclusion this study confirms the hypothesis that alcoholism causes brain damages that are partially reversible. It should be analyzed in further studies with larger sample sizes, if complete brain regeneration is possible maintaining abstinence over a longer period.
Similar content being viewed by others
Introduction
There is some evidence that alcoholism causes changes in brain morphology. The most prominent finding is an enlargement of the ventricular system, where the third ventricle [18, 23, 33] seems to be more affected than the lateral ventricles [10, 16, 27]. An increasing number of studies reports a shrinkage of prefrontal and frontal regions [22, 26, 29, 32] and of other brain structures such as the hippocampus [24, 31]. There is a controversial discussion if gray or white matter changes predominate [8, 17, 21, 26]. More recent studies could demonstrate an association of early age at first drinking and the extent of decreased gray matter volumes in the cerebellum, brainstem and frontal regions using voxel-based morphometry (e.g. [11]). Some authors report that brain damages in alcohol patients are sex- and age-related [19, 21, 22, 27]. In follow-up studies it was observed that these brain structure changes are at least partially reversible [9, 20, 33]. However, some studies found that after a long period of abstinence the recovery was still incomplete [23].
The aims of the presented study were twofold. Firstly, it was intended to confirm the brain morphological changes of alcohol patients in different key regions, the lateral ventricles, third ventricle, prefrontal lobes and amygdala-hippocampus-complex. Secondly, the analysis should discover which of these structures is affected most and where the brain damages start to regress after a period of abstinence. The influence of sex, age, duration of illness and other sociodemographic variables on the brain lesions should be considered as well as clinical intervening variables such as drinking status, the number of stationary detoxifications or additional psychiatric diagnosis.
The following basic hypotheses were set up:
-
patients in an acute phase of alcohol abuse show an intense ventricular enlargement and a moderate reduction of the prefrontal lobe compared to control subjects.
-
After a period of abstinence the brain damages are partially reversible.
Methods
Patients and control subjects
A total of 110 patients between 25 and 60 years of age meeting DSM III-R/ICD-10 criteria for alcohol dependence and consuming alcohol in an addictive manner for at least 6 months up to the admission to in-patient detoxification took part in a study comparing three alcoholism treatment programs with regard to drinking status [6, 7], neuropsychological performance [36] and structural magnetic resonance imaging (MRI). Exclusion criteria were other forms of addiction (except nicotine dependency), schizophrenia, mental retardation or severe cognitive impairments and somatic diseases which precluded participation in out-patient psychotherapy.
The participants were recruited from patients of a specialized ward for the detoxification and acute treatment of alcoholics between 1995 and 1996 and then treated as outpatients at the psychiatric clinic of the Heinrich-Heine-University Düsseldorf. After a complete description of the study, written informed consent was obtained from each subject. The local ethic committee reviewed and approved the study protocol, which is in accordance with the Declaration of Helsinki.
During the study blood examinations including assessment of red blood mean corpuscular volume (MCV), gamma-glutamyl transpeptidase (gamma-GT) and carbohydrate deficient transferrin (CDT) were carried out at each examination point. If the data on drinking behaviour were inconsistent, evaluation took place according to a worst-case-model meaning that in doubtful cases patients were classified as ‹relapsed’. Outcome criteria were defined according to the classification proposed by Feuerlein and Kuefner [15]:
-
1.
abstinent: no subjective reports or objective indications of alcohol consumption; CDT < 30 U/l during the last 6 months, 2. improved: during the last 6 months no more than three drinking periods lasting for less than a week (lapses) or less than 30 (in women) or 60 g (in male patients) alcohol per day on a regular basis, no signs of pathological drinking, neither physical nor psychiatric disorders nor in-patient treatments because of alcohol consumption, and 3. relapsed: more than three lapses or regular consumption of more than 30/60 g alcohol per day, alcohol-related disorders or in-patient treatments during the last 6 months.
The initial examination was performed between the 10th and 12th day of in-patient detoxification treatment (baseline, T 0). MRI-scans were taken at baseline (T 0) and between six and nine months later (T 1), in a phase of convalescence, the examinations were repeated. At that second time 56 alcohol patients remained in the study, while 54 patients dropped out the treatment program. The presented MRI-results are based on the data of patients with valid data at baseline and follow-up (56 patients).
A total of 41 of these patients were males (mean age: 42.0 years; mean disease duration: 21.9 years; mean age of onset: 20.4 years) and 15 females (mean age: 44.9 years; mean disease duration: 16.6 years; mean age of onset: 28.4 years).
Additionally, 45 healthy control subjects consisting of 29 males (mean age: 32.9 years) and 16 females (mean age: 39.4 years) were examined. Alcohol patients were significantly older than control subjects (F = 14.2; df = 1, 99, P < 0.001).
In alcohol patients sociodemographic variables, e.g. marital status, education, profession, medicament and smoking influences and clinical variables such as drinking status, the number of stationary detoxifications or additional psychiatric diagnosis other than disorders due to alcohol dependence were examined systematically.
A total of 13 of the 56 patients were married. 26 subjects left school with secondary school or higher graduate, 29 had lower education. 26 patients were employees, 10 were workers and 11 unemployed. 11 patients were treated with psychotropic medicaments before baseline MRI-assessment (T 0). A total of 13 patients were heavy smokers and 43 showed no noticeable nicotine abuse. At follow-up (T 1) 30 of the alcohol patients were abstinent, 13 patients showed an improved drinking behavior and in 13 patients the drinking status has not been essentially improved. The majority of the patients (40 subjects) took part only in one stationary detoxification. 21 of the alcohol patients had no additional psychiatric diagnosis according to ICD-10, 5 had an F3 diagnosis (affective disorder) and 30 patients had an F6 diagnosis (disorder of adult personality or behavior). Basic sociodemographic data and disease characteristics are presented in Table 1.
MRI acquisition and volumetric measurement
MRI-scans were taken at a radiological practice in Düsseldorf on a 1.5 Tesla Siemens-Magnetom, using the Inversion Recovery technique. Each MRI consisted of 19 coronal slices of 6.0 mm thickness and 1.2 mm distance (image matrix: 180 × 256; pixel size 0.8 mm × 0.8 mm; field of view: 173 mm × 230 mm).
From all MRI-scans hardcopies were taken. Manual outline of all MRI-slices was processed using an overhead projector. The areas of the whole brain, the lateral ventricles, the third ventricle, the prefrontal lobe and the amygdala-hippocampus-complex were determined on a planimeter considering the following criteria.
The prefrontal lobe was outlined from the first slice in caudal view to the first slice, where the corpus callosum was visible. The lateral ventricles and the third ventricle could be separated well from the brain tissue. Nevertheless, in some brains the first and the last slices of the ventricles were difficult to determinate. Because of the lack of clear boundaries between hippocampus and amygdala, both limbic nuclei were measured as one structure consisting of a posterior and an anterior portion using the mamillary bodies as anatomical landmarks (for details see [5]).
To obtain the volume of the whole brain and the outlined brain structures the integral of all areas was calculated (as described in [12]). Objective of the study was to detect local rather than global brain structural deficits in alcohol patients. Therefore, the structure volumes were expressed as percentage of the total brain volume.
Quotients between the two repeated measurements (T 1/T 0- quotients) were calculated to determinate volume changes in the phase of convalescence compared to the acute phase of alcohol drinking.
To test for reliability, volumetric measurement of 8 brains were performed twice by the same rater and by an independent person. Intraclass correlation (ICC) [30] were computed to determine the reliability. For volumes of the lateral ventricles measurements were reliable (left: retest: ICC = 0.99; interrater: ICC = 0.92; right: retest: ICC = 0.98; interrater: ICC = 0.93). In the prefrontal lobe, there was a good retest (left: ICC = 0.81; right: ICC = 0.81), but a weaker interrater reliability. (left: ICC = 0.52; right: ICC = 0.52). For the third ventricle (retest: ICC = 0.74; interrater: ICC = 0.35) and for the amygdala-hippocampus-complex (left: retest: ICC = 0.12; interrater: ICC = −0.83; right: retest: ICC = 0.17; interrater: ICC = −0.34) the reliability was insufficient. Since the measurements could not have been improved, third ventricle and amygdala-hippocampus-complex had to be excluded from the analysis.
Statistical analysis
Statistical analyses were performed with SPSS for Windows [25], all tests were two-tailed. Boxplots were examined to identify extreme values.
Dependent variables were bilateral relative volumes of lateral ventricles and prefrontal lobes and the corresponding T 1/T 0-quotients as a measure of change between T 0 and T 1. For these variables no significant sex differences resulted from one-way ANOVA. Since there were significant correlations between age and lateral ventricles, and on the other hand, the mean age was significantly different between alcohol patients and control subjects, for relative lateral ventricle volumes a one-way ANCOVA with independent factor diagnosis and covariate age was calculated. For comparison of prefrontal lobe volumes between alcohol patients and control subjects a one-way ANOVA with independent factor diagnosis was performed. Additionally, an age-matched subsample consisting of 40 alcohol patients and 40 healthy controls was analyzed on diagnosis differences using ANCOVA (factor diagnosis, covariate age).
Objective of the study was mainly to compare the brain structures at baseline (T 0) when still drinking excessive alcohol and at follow-up (T 1), in convalescence. Therefore, the main analysis for all dependent variables was performed with ANOVA with repeated measures, comparing the relative volumes between T 0 and T 1.
Brain structure volume intercorrelations were calculated between T 0 and T 1, right and left side, such as between lateral ventricles and prefrontal lobes. The influence of the intervening variables was analyzed systematically with one-way ANOVA or with Pearson product moment correlations/Spearman rank correlations, respectively.
From boxplots one patient with extremely large lateral ventricles was identified (more than three standard deviations above mean volume). This patient was excluded from the analysis for lateral ventricles, but nor for the prefrontal lobes.
Results
Alcohol patients compared to control subjects
Numerically, there was a large increase of relative lateral ventricle volumes in alcohol patients (right: +32%; left: +42%). However, taking the age structure of the sample into account, mean differences were only significant on the left side (df = 1, 97; F = 6.4; P = 0.013), revealing just a trend on the right (df = 1, 97; F = 3.7; P = 0.057).
The prefrontal lobe was significantly smaller in alcohol patients compared to control subjects (left: −11%; df = 1, 99; F = 7.6; P = 0.007; right: −11%; df = 1, 99; F = 8.5; P = 0.004).
The results are summarized in Table 2 .
To rule out the possibility that age accounted for the volumetric differences between control subjects and alcohol patients found at baseline, an analysis of an age-matched subsample has been undertaken. This subsample consisted of 40 healthy control subjects (26 male: mean age = 34.31, SD = 7.55; 14 female: mean age = 42.29, SD = 11.08) and 40 alcohol patients (30 male: mean age = 38.73, SD = 5.0; 10 female: mean age = 41.20, SD = 6.01). We observed similar significant volumetric differences in the age-matched subsample comparing alcohol patients vs. controls for left lateral ventricle (+27%; F = 4.83, df = 1.77, P = 0.031), right lateral ventricle (+20%; F = 2.42, df = 1.77, P = 0.12), and left prefrontal lobe (–8%; F = 4.99, df = 1.77, P = 0.028). We could find a trend for the reduction of the right prefrontal lobe (–7%; F = 2.91, df = 1.77, P = 0.092) in alcohol patients compared to age-matched healthy control subjects.
Volumetric MRI changes in alcohol patients
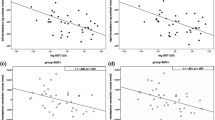
In alcohol patients, there was a bilateral reduction of relative lateral ventricle volumes at follow-up, in the phase of convalescence (T 1), compared to baseline (T 0) (left side: −6%; df = 1, 54; F = 11.4; P = 0.001; right side: −5%; df = 1, 54; F = 5.4; P = 0.024). In Fig. 1, a scatterplot of the relative ventricle volumes in T 1 × T 0 is shown. Data points above the regression line indicate a reduction below average and points under the regression line indicate a reduction above average.
Relative volumes of lateral ventricles in T 1 and T 0. A scatterplot of the relative ventricle volumes as percentage of the total brain volume in T 1 × T 0 is shown (x-axis: relative ventricular volume at T 0, y-axis: relative ventricular volume at T 1). Mean values of the volumes at T 0 are visualized as vertical lines, mean values of the volumes at T 1 are visualized as horizontal lines. A regression line from linear least square regression is added. Data points above the regression line indicate a volume reduction below average or even a volume increase and points under the regression line indicate a volume reduction above average
The detailed results of volumetric changes at follow-up are summarized in Table 3.
There was no significant difference of mean prefrontal lobe volumes between T 1 and T 0 (left: −1%; df = 1, 55; F = 0.1; P = 0.77; right: +1%; df = 1, 55; F = 0.2; P = 0.70).
For volumes of the lateral ventricles, there were strongly positive correlations between the measurements in T 1 and T 0 (left: r = 0.95, df = 54, P < 0.0005; right: r = 0.93, df = 54, P < 0.0005). For prefrontal lobe volumes, correlations between T 1 and T 0 were significantly positive as well (left: r = 0.37, df = 55, P = 0.005; right: r = 0.40, df = 55, P = 0.002), but not to such a high degree. There were negative correlations between the volumes of lateral ventricles and prefrontal lobes (left: T 0: r = −0.24, df = 54, P = 0.083; T 1: r = −0.31, df = 54, P = 0.021; right: T 0: r = −0.41, df = 54, P = 0.002; T 1: r = −0.24, df = 54, P = 0.080).
Correlations with intervening variables
Correlations between age of the patients and ventricular volumes were positive (left: T 0: r = 0.33, df = 54, P = 0.014; T 1: r = 0.32, df = 54, P = 0.017; right: T 0: r = 0.22, df = 54, P = 0.12; T 1: r = 0.18, df = 54, P = 0.18), reaching the level of significance only on the left side. There was no significant influence of other sociodemographic variables, such as sex, duration of illness, age at onset of the disease, education, marital status, profession or chronic cigarette smoking. The recovery of the lateral ventricles, expressed through the T 1/T 0-quotient, was associated with the drinking status at follow-up (T 1) and the number of detoxifications. While in patients with success in their drinking behavior (outcome criteria abstinent or improved drinking behavior) ventricular enlargement decreased significantly on the left side (left: T 1/T 0 = 0.93; right: T 1/T 0 = 0.96; left: df = 1, 53; F = 5.2; P = 0.027; right: df = 1, 53; F = 1.2; P = 0.28), relapsing patients showed no ventricular regression (left: T 1/T 0 = 1.03; right: T 1/T 0 = 1.02).
Interestingly, in patients that underwent at least two previous detoxifications ventricular enlargement proceeded (left: T 0 = 1.07, T 1 = 1.06, T 1/T 0 = 1.02; right: T 0 = 0.97, T 1 = 0.96, T 1/T 0 = 1.03), in contrast to patients with only one detoxification (left: T 0 = 1.32, T 1 = 1.19, T 1/T 0 = 0.92; right: T 0 = 1.16, T 1 = 1.07, T 1/T 0 = 0.94), showing a significant regress on the left (df = 1, 53; F = 6.0; P = 0.018) and a trend on the right side (df = 1, 53; F = 2.9; P = 0.097).
The daily average alcohol consumption at baseline (T 0) did neither correlate significantly with the ventricular enlargement or the prefrontal volume reduction at baseline nor with the recovery of these volumetric findings at follow-up (T 1/T 0). Nevertheless the alcohol dependent changes of laboratory parameters, elevated MCV (mean corpuscular volume) and gamma-GT (gamma-glutamyl transpeptidase), were significantly associated with the brain abnormalities. MCV at baseline (T 0) showed a significant positive correlation with lateral ventricle volume at T 0 (right: r = 0.291, P = 0.031; left: r = 0.369, P = 0.006; Pearson rank correlations), and MCV at follow-up (T 1) correlated significantly with the volume of the left lateral ventricle at T 1 (r = 0.313, P = 0.027; Pearson correlations) and moreover, comparing the ratios T 1/T 0 as a measure of change between T 0 and T 1, there was a significant correlation between MCV and both lateral ventricles as well (right: r = 0.537, P < 0.001; left: r = 0.454, P = 0.001; Pearson correlations). Gamma-GT at follow-up (T 1) demonstrated a significant positive correlation with the volumes of the lateral ventricles at T 1 (right: rho = 0.279, P = 0.050; left: rho = 0.302, P = 0.033; Spearman rank correlations, while normality distribution for gamma-GT was not fulfilled) and for the ratio T 1/T 0 (right: rho = 0.479, P < 0.001; left: rho = 0.466, P = 0.001; Spearman rank correlations).
Alcohol patients with personality or behavior disorder (according to ICD-10 F6-diagnosis) had smaller lateral ventricles compared to patients without additional psychiatric ICD-10 diagnosis (left: T 0: −30%, df = 2, 52; F = 4.8, P = 0.012; T 1: −26%, df = 2, 52; F = 4.2, P = 0.021; right: T 0: −19%, df = 2, 52; F = 1.5, P = 0.23; T 1: −14%, df = 2, 52; F = 1.1, P = 0.36).
In the prefrontal lobe there was no significant influence of sex, age, duration of illness or age at onset. Correlations between education and the T 1/T 0-quotient were negative (left: r = −0.29, df = 54, P = 0.034; right: r = −0.26, df = 54, P = 0.052), indicating a lower increase of prefrontal brain volume in patients with higher education during the convalescence period. There were no other variables showing a significant influence on the brain morphology of the prefrontal lobe.
Discussion
This study supports the hypothesis that chronic alcohol abuse affects different parts of the brain. In outpatients with chronic alcoholism lateral ventricles were enlarged more than 30% compared to control subjects. These results are in line with studies showing an enlargement of lateral ventricles of severely dependent alcohol patients compared to their non alcoholic twins [16, 27]. In the present study, after a period of convalescence a significant regress of about 5% of the ventricular enlargement could be shown. Other authors reported on a regeneration of the ventricular system as well [20, 33], however, objective of these studies was mainly the third ventricle.
The prefrontal lobe volume in alcohol patients was reduced for more than 10% compared to control subjects. This fits to the results of other studies reporting lesions of the prefrontal brain regions [26, 29]. Especially in older alcohol patients frontal deficits could be observed in these studies. In contrast to the ventricular enlargement, not even partially regeneration of the prefrontal lobes could be demonstrated after 6 months of convalescence for the present sample.
The results of our study suggest that excessive alcohol drinking causes brain volumetric deficits that could be partially reversible if patients reduce their alcohol consumption or stay abstinent. Probably, in the affected cortical regions the brain regeneration may take a longer time than needed for the ventricular system. However, it is unclear if a complete recovery of the brain damages is possible at all [23].
It was shown that long-term abstinent alcoholics still present reduced gray matter density within the amygdala [14], which may be the result of long-term alcohol abuse or dependence, but may also reflect a pre-existing factor that predisposes to severe alcoholism. Alcohol patients may also have a disposition for brain deficits such as ventricular enlargement or decrease of frontal lobes before beginning with excessive alcohol consumption. This assumption was supported by studies investigating high-risk subjects for alcohol dependence reporting significantly smaller volumes of superior frontal, cingulate and parahippocampal gyri, amygdyla, thalamus and cerebellum compared to matched low-risk subjects [2].
Then, these brain deficits would be a possible cause of the disease and on the other hand the disease would deteriorate the brain deficits. Following this explanation, which is supported by the finding that in our study there were no significant correlations between duration of illness and brain structure volumes, it could not be expected that mean volumes of alcohol patients reach the level of control subjects, not even after long periods of abstinence. In contrast other studies could demonstrate an association of early age at first drinking and the extent of decreased gray matter volumes in the cerebellum, brainstem and frontal regions using voxel-based morphometry [11].
Comparing baseline to follow-up, lateral ventricle enlargement only decreased in patients with treatment success. One plausible explanation for this finding is, that in patients showing no essential improvement of their drinking behavior and relapsing, chronic toxicity of alcohol on the brain still persists and therefore ventricular regeneration could not be expected. A recent study investigating recovering alcohol patients with deformation tensor morphometry, a new MRI processing method suggested to be more sensitive to focal effects on brain structure, showed significantly faster recovery in the frontal and temporal lobe in abstainers than in light drinkers [9]. In abstainers compared to relapsing patients significantly greater recovery was observed in temporal lobe, thalamus, brainstem, cerebellum, corpus callosum, anterior cingulated, insula, and subcortical white matter [9]. This underlines the effect of maintaining sobriety on the recovery of different brain structures and fits to our results, although there are relevant methodological differences between the studies.
Regeneration of the ventricular enlargement could only be observed in patients having not more than one detoxification in their disease course. This finding might be explained by the observation that the ventricular enlargement of subjects with only one detoxification was above average at baseline (T 0), suggesting the first alcohol excess might have the strongest negative effect on the ventricular system, especially when the elevated alcohol consumption continues over many years. Patients with multiple detoxifications may have experienced certain periods of previous abstinence and recovery of the brain from alcohol toxic effects before entering the study.
We could observe a significant correlation between alcohol dependent changes of liver function (elevated gamma-GT) as well as blood chemistry (elevated MCV), and brain abnormalities (increased ventricular enlargement). Decreased gamma-GT and MCV at follow-up were associated with recovery of ventricular enlargement. Our findings were supported though the literature, e.g. one study reporting a correlation between lower red blood cell count, hemoglobin level, and hematocrit with higher ventricular volumes in alcoholic men [28].
There is much evidence that lateral ventricles are enlarged in certain psychiatric diseases, e.g. schizophrenia [13, 37]. On this background it amazes that the lateral ventricles of alcohol patients without additional psychiatric ICD-10 diagnosis were increased compared to patients with personality or behavior disorder (ICD-10: F6). This might be a sample artifact. On the other hand persons with small ventricles might dispose to personality or behavior disorders.
The precise neurobiological pathophysiology of the volume recovery during abstinence is not known. Proposed explanations have been rehydration (vasopressin secretion may be suppressed during alcohol intoxication), regeneration (augmented dendritic growth) or changes in perfusion (vascularization) [34]. The rehydration hypothesis has not been confirmed by the majority of investigators using post-mortem examination. It has been demonstrated that, during high-dose alcohol ingestion and acute withdrawal, there is a significant but transient reduction in perfusion of the brain as shown by single photon emission tomography (SPECT), PET and measures of regional cerebral blood flow using Xenon 133 (133Xe-rCBF) investigations [3, 4, 35]. This reduction was thought to lead to atrophic brain changes, as it is known for other chronic hypoperfusion states. Therefore increased perfusion after sobriety could be responsible for the volume recovery. However, more recent studies reveal evidence for neuronal and white matter regeneration (glial and neuronal regrowth) in alcohol patients after abstinence [12], e.g. using additionally proton MR spectroscopy in follow-up investigations and showing elevation of N-acteyl-aspartate, a neuronal marker, in frontomesial regions and choline, a marker for myeline, in the cerebellum [1].
There are some limitations of our study. One shortcoming of this study is the method of MRI-processing. A semi-computerized procedure would have been preferred to the manual delineation using hardcopies and overhead projection. In the latter method, which was used for this study, there are more sources of error probably being responsible for the weak reliability in brain structures that were difficult to delineate such as the amygdala-hippocampus-complex or the third ventricle. Unfortunately the technical requirements for computer supported MRI-processing were not available in this study. Nevertheless, for the analyzed regions the data show sufficient high reliability, comparable to the other cited studies. Another limitation of our study is that we did not evaluate the exactly amount of alcoholic drinks taken during the follow-up period. So, we could not estimate a dose-dependent influence of the target brain structures at follow-up.
However, there are some strengths of our study. We were able to follow a relatively large sample of patients and could perform brain imaging 6–9 months after baseline. There are not many studies available using the region of interest approach investigating large sample sizes during longer time periods. Most studies consist of small sample sizes and short time intervals for rescanning after obtaining sobriety.
In summary, our hypotheses of differences in key brain structures for the disease between alcoholic patients and healthy controls as well as the reversibility of ventricular enlargement after reducing drinking behavior were essentially confirmed. Further follow-up studies might be useful to answer the question if brain damages caused by alcohol abuse are completely reversible. However, such studies should be designed over a period of 10 years or more and because of a high expected rate of relapsing patients and drop-outs they would require a very large sample size at baseline.
References
Bartsch AJ, Homola G, Biller A, Smith SM, Weijers HG, Wiesbeck GA, Jenkinson M, Stefano N, Solymosi L, Bendszus M (2007) Manifestation of early brain recovery associated with abstinence from alcoholism. Brain 130(Pt 1):36–47
Benegal V, Antony G, Venkatasubramanian G, Jayakumar PN (2007) Gray matter volume abnormalities and externalizing symptoms in subjects at high risk for alcohol dependence. Addict Biol 12(1):122–132
Berglund M, Risberg J (1981) Regional cerebral blood flow during alcohol withdrawal. Arch Gen Psychiatry 38:351–355
Berglund M, Hagstadius S, Risberg J, Johanson TM, Bliding Å, Mubrin Z (1987) Normalization of regional cerebral blood flow in alcoholics during the first 7 weeks of abstinence. Acta Psychiatr Scand 75:202–208
Bogerts B, Ashtari M, Degreef G, Alvir JM, Bilder RM, Lieberman JA (1990) Reduced temporal limbic structure volumes on magnetic resonance images in first episode schizophrenia. Psychiatry Res (Neuroimaging) 35:1–13
Burtscheidt W, Wölwer W, Schwarz R, Strauss W, Loll A, Lüthcke H, Redner C, Gaebel W (2001) Out-patient behaviour therapy in alcoholism: relapse rates after 6 months. Acta Psychiatr Scand 103(1):24–29
Burtscheidt W, Wölwer W, Schwarz R, Strauss W, Gaebel W (2002) Outpatient behaviour therapy in alcoholism: treatment outcome after 2 years. Acta Psychiatr Scand 106:227–232
Cardenas VA, Studholme C, Meyerhoff DJ, Song E, Weiner MW (2005) Chronic active heavy drinking and family history of problem drinking modulate regional brain tissue volumes. Psychiatry Res 138(2):115–130
Cardenas VA, Studholme C, Gazdzinski S, Durazzo TC, Meyerhoff DJ (2007) Deformation-based morphometry of brain changes in alcohol dependence and abstinence. Neuroimage 34(3):879–887
Cascella NG, Pearlson G, Wong DF, Broussolle E, Nagoshi C, Margolin RA, London ED (1991) Effects of substance abuse on ventricular and sulcal measures assessed by computerised tomography. Br J Psychiatry 159:217–221
Chanraud S, Martelli C, Delain F, Kostogianni N, Douaud G, Aubin HJ, Reynaud M, Martinot JL (2007) Brain morphometry and cognitive performance in detoxified alcohol-dependents with preserved psychosocial functioning. Neuropsychopharmacology 32(2):429–438
Crews FT, Buckley T, Dodd PR, Ende G, Foley N, Harper C, He J, Innes D, Loh EW, Pfefferbaum A, Zou J, Sullivan EV (2005) Alcoholic neurobiology: changes in dependence and recovery. Alcohol Clin Exp Res 29(8):1504–1513
Falkai P, Bogerts B, Schneider T, Greve B, Pfeiffer U, Pilz K, Gonsiorzcyk C, Majtenyi C, Ovary I (1995) Disturbed planum temporale asymmetry in schizophrenia. A quantitative post-mortem study. Schizophr Res 14:161–176
Fein G, Landman B, Tran H, McGillivray S, Finn P, Barakos J, Moon K (2006) Brain atrophy in long-term abstinent alcoholics who demonstrate impairment on a simulated gambling task. Neuroimage 32(2):1465–1471
Feuerlein W, Küfner H (1989) A prospective multicenter study on inpatient treatment for alcoholics: 18- and 48-months follow-up. Eur Arch Psychiatry Neurol Sci 239:144–157
Gurling HM, Reveley MA, Murray RM (1984) Increased cerebral ventricular volume in monozygotic twins discordant for alcoholism. Lancet 1(8384):986–988
Harper C, Kril J (1991) If you drink your brain will shrink. Neuropathological considerations. Alcohol Alcohol Suppl 1:375–380
Kato A, Tsuji M, Nakamura M, Nakajima T (1991) Computerized tomographic study on the brain of patients with alcohol dependence. Jpn J Psychiatry Neurol 45(1):27–35
Mann K, Batra A, Guenthner A, Schroth G (1992) Do women develop alcoholic brain damage more readily than men? Alcohol Clin Exp Res 16(6):1052–1056
Mann K, Mundle G, Strayle M, Wakat P (1995) Neuroimaging in alcoholism: CT and MRI results and clinical correlates. J Neural Transm Gen Sect 99(1–3):145–155
Mann K, Widmann U (1995) The neurobiology of alcoholism. Neuropathology and CT/NMR findings. Fortschr Neurol Psychiatr 63(6):238–247
Medina KL, McQueeny T, Nagel BJ, Hanson KL, Schweinsburg AD, Tapert SF (2008) Prefrontal cortex volumes in adolescents with alcohol use disorders: unique gender effects. Alcohol Clin Exp Res 32(3):386–394
Muuronen A, Bergman H, Hindmarsh T, Telakivi T (1989) Influence of improved drinking habits on brain atrophy and cognitive performance in alcoholic patients: a 5-year follow-up study. Alcohol Clin Exp Res 13(1):137–141
Nagel BJ, Schweinsburg AD, Phan V, Tapert SF (2005) Reduced hippocampal volume among adolescents with alcohol use disorders without psychiatric comorbidity. Psychiatry Res 139(3):181–190
Norusis MJ (2000) SPSS 10.0 guide to data analysis. Prentice Hall, New Jersey
Pfefferbaum A, Sullivan EV, Mathalon DH, Lim KO (1997) Frontal lobe volume loss observed with magnetic resonance imaging in older chronic alcoholics. Alcohol Clin Exp Res 21(3):521–529
Pfefferbaum A, Rosenbloom M, Deshmukh A, Sullivan EV (2001) Sex differences in the effects of alcohol on brain Structure. Am J Psychiatry 158(2):188–197
Pfefferbaum A, Rosenbloom MJ, Serventi KL, Sullivan EV (2004) Brain volumes, RBC status, and hepatic function in alcoholics after 1 and 4 weeks of sobriety: predictors of outcome. Am J Psychiatry 161(7):1190–1196
Ratti MT, Soragna D, Sibilla L, Giardini A, Albergati A, Savoldi F, Bo P (1999) Cognitive impairment and cerebral atrophy in “heavy drinkers”. Prog Neuropsychopharmacol Biol Psychiatry 23(2):243–258
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Sullivan EV, Marsh L, Mathalon DH, Lim KO, Pfefferbaum A (1995) Anterior hippocampal volume deficits in nonamnesic, aging chronic alcoholics. Alcohol Clin Exp Res 19(1):110–122
Sullivan EV, Marsh L, Mathalon DH, Lim KO, Pfefferbaum A (1996) Relationship between alcohol withdrawal seizures and temporal lobe white matter volume deficits. Alcohol Clin Exp Res 20(2):348–354
Sullivan EV, Rosenbloom MJ, Lim KO, Pfefferbaum A (2000) Longitudinal changes in cognition, gait, and balance in abstinent and relapsed alcoholic men: relationships to changes in brain structure. Neuropsychology 14(2):178–188
Trabert W, Betz T, Niewald M, Huber G (1995) Significant reversibility of alcohol brain shrinkage within 3 weeks of abstinence. Acta Psychiatr Scand 92:87–90
Tutus K, Kugu N, Sofuoglu S, Simsek A, Karaaslan F, Gonul AS (1998) Transient frontal hypoperfusion in Tc-99 hexamethylpropyleneamineoxime single photon emission tomography imaging during alcohol withdrawal. Biol Psychiatry 15:923–928
Wölwer W, Burtscheidt W, Redner C, Schwarz R, Gaebel W (2001) Out-patient behaviour therapy in alcoholism: impact of personality disorders and cognitive impairments. Acta Psychiatr Scand 103(1):30–37
Wright IC, Rabe-Hesketh S, Woodruff PW, David AS, Murray RM, Bullmore ET (2000) Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry 157(1):16–25
Acknowledgment
Supported by the BMBF; Grant no.: 01 EB 9408.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Wobrock, T., Falkai, P., Schneider-Axmann, T. et al. Effects of abstinence on brain morphology in alcoholism. Eur Arch Psychiatry Clin Neurosci 259, 143–150 (2009). https://doi.org/10.1007/s00406-008-0846-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-008-0846-3