Abstract
Background and aims
The aim of this study was to determine the incidence of bleeding complications from various laparoscopic procedures in a nationwide prospective multicentre study in Switzerland from 1995 to 2001 following an initial learning curve.
Patients and methods
Since 1989, the Swiss Association of Laparoscopic and Thoracoscopic Surgery (SALTS) has prospectively collected data from patients undergoing laparoscopic or thoracoscopic surgery at 114 surgical institutions (university, county and district hospitals, private practice). More than 130 items of data, including indication for surgery, intraoperative course, local as well as general postoperative complications, mortality and follow-up were recorded on a computerised data sheet.
Results
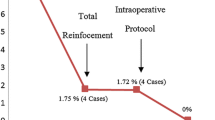
Some 43,028 procedures were assessed and analysed. Local morbidity (e.g. wound infections) occurred in 0.05% of the whole patient group, whereas 3.3% developed general postoperative complications. The overall mortality rate was 0.2%. In 1.7% of the cases, the intraoperative course was complicated by internal bleeding or haematoma of the abdominal wall. In the postoperative course, 1.5% of the patients presented with internal bleeding or bleeding of the abdominal wall. Major vascular injury occurred in 0.09%. This patient group with bleeding complications was analysed in the context of the operator’s experience, instrumental lesions (Veress needle or trocar) and conversion incidence. Furthermore, a trend analysis of the complication rate from 1995 to 2001 was performed.
Conclusion
Although the initial learning curve of laparoscopic procedures is probably finished, the rate of bleeding complications is still substantial. These results demonstrate that the collection of data in the form of multicentre studies is essential for quality control. It permits recognition and understanding of the current problems in laparoscopic surgery in order to improve the quality of daily surgical practice. The fact that the operator’s experience seems to play an important role shows that improvement in learning and teaching programmes is still necessary and should be coordinated on a national basis.


Similar content being viewed by others
References
Shea JA, Healey M, Berlin J, Clarke J, Malet P, Staroscik R, Schartz S, Williams S (1998) Mortality and complications associated with laparoscopic cholecystectomy: a metaanlaysis. Ann Surg 224:609–620
Hashizume H, Sugimachi K (1997) Study group on endoscopic surgery needle and trocar injury during laparoscopic surgery in Japan. Surg Endosc 11:1198–1201
Champault G, Cazacu F, Taffinder N (1996) Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc 6:367–370
Deziel DJ, Millikan WK, Economou SG, Doolas A, Ko ST, Airan MC (1993) Complications of laparoscopic cholecystectomy: a national survey of 4292 hospitals and an analysis of 77,604 cases. Am J Surg 165:9–14
Roviaro GC, Varoli F, Saguatti L, Vergani C, Maciocco M, Scarduelli A (2002) Major vascular injuries in laparoscopic surgery. Still of interest? Surg Endosc 16:1192–1196
Sigman HH, Fried GM, Garzon J, Hinchey EJ, Wexler MJ, Meakins Barkun JS (1993) Risks of blind versus open approach to celiotomy for laparoscopic surgery. Surg Laparosc Endosc 3:296–299
Fruhwirth J, Koch G, Mischinger HJ, Werkgartner G, Tesch NP (1997) Vascular complications in minimally invasive surgery. Surg Laparosc Endosc 7:251–254
Usal H, Sayad P, Hayek N, Hallak A, Huie F, Ferzli G (1998) Major vascular injuries during laparoscopic cholecystectomy. Surg Endosc 12:960–962
Geers J, Holden C (1996) Major vascular injury as a complication of laparoscopic surgery: a report of three cases and review of the literature. Am Surg 62:377–379
Härkki-Siren P, Kurki T (1997) A nationwide analysis of laparoscopic complications. Obstet Gynecol 89:108–112
Cogliandolo A, Manganaro T, Saitta FP, Micali B (1998) Blind versus open approach to laparoscopic cholecystectomy: a randomized study. Laparosc Endosc Surg 8:353–355
Mayol J, Garcia Aguilar J, Ortiz Oshiro E, De Diego Carmona JA, Fernandez Represa JA (1997) Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg 21:529–533
Scheidbach H, Schneider C, Huegel O, Bärlehner R, Konradt K, Wittekind C, Köckerling F (2002) Laparoscopic sigmoid resection for cancer. Curative resection and preliminary medium-term results. Dis Colon Rectum 45:1641–1647
Merlin TL, Hiller JE, Maddern GJ, Jamieson GG, Brown AR, Kolbe A (2003) Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg 90:668–679
Schäfer M, Lauper M, Krähenbühl L (2000) A nation’s experience of bleeding complications during laparoscopy. Am J Surg 180:73–77
Wherry DC, Marohn MR, Malanoski MP, Hetz SP, Rich NM (1996) An external audit of laparoscopic cholecystectomy in the steady state performed in medical treatment facilities of the Department of Defense. Ann Surg 224:145–154
Loffler FD, Pent D (1975) Indication, contraindications, and complications of laparoscopy. Obstet Gynecol Surg 30:407–427
McDonald PT, Rich NM, Collins GJ, Anderson CA, Kozloff L (1978) Vascular trauma secondary to diagnostic and therapeutic procedures: laparoscopy. Am J Surg 135:651–655
Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson J (1997) Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg 185:461–465
Penfield AJ (1997) Trocar and needle injury. In: Philips JM (ed) Laparoscopy. Williams and Wilkins, Baltimore, pp 236–241
Bonjer HJ, Hazebroek EJ, Kazemier G, Giuffrida MC, Meijer WS, Lange JF (1997) Open versus closed establishment of pneumoperitoneum in laparoscopic surgery. Br J Surg 84:599–602
Balzer KM, Witte H, Recknagel S, Kozinaka J, Waleczek H (1999) Anatomic guidelines for the prevention of abdominal wall hematoma induced by trocar placement. Surg Radiol Anat 21:87–89
Hanney RM, Carmalt HL, Merret N, Tait N (1999) Use of the Hasson cannula producing major vascular injury at laparoscopy. Surg Endosc 13:1238–1240
Hulka J, Peterson H, Phillips J, Surrey M (1995) Operative laparoscopy: American Association of Gynecologic Laparoscopists’ 1993 Membership Survey. J Am Assoc Gynecol Laparosc 2:133–136
Sutton C (1992) Operative laparoscopy. Curr Opin Obstet Gynecol 4:430–438
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Opitz, I., Gantert, W., Giger, U. et al. Bleeding remains a major complication during laparoscopic surgery: analysis of the SALTS database. Langenbecks Arch Surg 390, 128–133 (2005). https://doi.org/10.1007/s00423-004-0538-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-004-0538-z