Abstract
Human metapneumovirus (hMPV) and respiratory syncytial virus (RSV) are important respiratory pathogens with similar symptomatology. The aim of this prospective birth cohort study was to identify risk factors for an hMPV or RSV infection during the first year of life in unselected healthy children. We followed 217 children from birth to 1 year of age. Nasal swabs and symptom diaries were collected monthly. Anti-hMPV and anti-RSV IgG antibodies by age 1 year were detected by ELISA, and nasal swabs were analysed for hMPV and RSV by RT-PCR. Logistic regression was used for risk factor analysis. Anti-hMPV IgG was found in 38 children (17.5%), and anti-RSV IgG in 172 children (79%). Risk factors for being anti-hMPV IgG-positive were: (1) being born in the spring (OR = 2.36; 95% CI:1.06–5.27), and (2) having older siblings (OR = 3.82; 95% CI:1.75–8.34). Risk factors for being anti-RSV IgG-positive were: (1) gestational age <38 weeks (OR = 3.39; 95% CI:1.42–8.05), (2) increasing paternal age (OR = 1.85 per 5 yrs; 95% CI:1.28–2.68), and (3) wall-to-wall carpeting (OR = 3.15; 95% CI:1.29–7.68). Being born in the spring was associated with decreased odds of being anti-RSV IgG-positive (OR = 0.27, 95% CI:0.09–0.85). Risk factors for RSV hospitalisation (n = 11) were: (1) older siblings (OR = 4.49; 95% CI: 1.08–18.73) and (2) smoking in the household (OR = 5.06; 95% CI: 1.36–18.76). Exclusive breastfeeding for the first 14 days of life protected against hospitalisation (OR = 0.21; 95% CI:0.06–0.79). In conclusion, this study identifies risk factors for mild and asymptomatic hMPV infections in infancy.
Similar content being viewed by others
Introduction
Since its discovery by Dutch researchers in 2001, human metapneumovirus (hMPV) has been found in all age groups worldwide [15]. A number of studies have compared the clinical symptoms associated with hMPV infection in hospitalised children with those associated with respiratory syncytial virus (RSV) infections [1, 3, 12, 27, 28, 36, 37, 39, 42]. Although hMPV infections in many studies tend to be slightly milder than RSV infections, a statistically significant difference was not observed. Few studies have reported longer hospital stays for hMPV-infected children than for RSV-infected children [25, 28].
Most studies have shown that around 20% of children acquire hMPV infection during their first year of life [22, 35, 43], while approximately 70% acquire RSV infection [13]. One to 3 percent of RSV-infected children get hospitalised, and several studies have identified a number of risk factors for severe RSV infection [2, 5, 20, 26, 32]. A recent study suggests that risk factors for hMPV hospitalisation appear to be similar to risk factors for RSV hospitalisation [30]. However, risk factors leading to hospitalisation in high-risk groups are not necessarily identical to risk factors for infection in the general population. Little is known about factors protecting against hospitalisation for hMPV infection. As both hMPV and RSV infection have been associated with subsequent wheezing [11, 19, 21, 33], it is important to investigate risk factors for early infection in order to prevent or postpone infection in predisposed individuals.
In the present study we followed a cohort of healthy infants from birth to 1 year of age. The aim of the study was to identify risk factors for an early hMPV or RSV infection in otherwise healthy children in the community. This information will help recognize children at risk of an early infection who might benefit from preventive intervention strategies.
Materials and methods
Study population
Children were enrolled from the post-natal ward at Copenhagen University Hospital, Hvidovre, Denmark. To ensure that children were sampled equally throughout the year, we aimed at including a predetermined number of 20 children each month during a 12-month period from May 2004 to May 2005. The inclusion criteria for participation in the study were: (1) infants free of obvious health problems and (2) for practical purposes living within a radius of 11 km from the hospital. Exclusion criteria were: (1) infants whose parents did not understand or speak Danish or English, (2) infants whose mothers had a serious psychiatric disorder, (3) infants with congenital diseases, and (4) if change of address to outside the area of Hvidovre Hospital was planned within 12 months of enrolment. Written informed consent was obtained from the parents of the infant after they had been informed about the study and before performance of any study procedure. Study approval was obtained from the Ethics Committee of Frederiksberg, Copenhagen, Denmark.
Sample size calculation
We assumed that 75% and 25% of the children became infected with RSV and hMPV, respectively, during the first year of life. With a chosen sample size of 200 subjects, it would be possible to detect risk factors for RSV or hMPV infection during the first year of life, with relative risks of 1.3 and 2.1 respectively. Differences in symptoms related to RSV and hMPV infection could be detected with an odds ratio (OR) of 2.8, under the assumption of 5% significance level and 80% strength. Power calculations were made in EpiInfo 2000.
Clinical data
Parents were provided monthly with a health diary displaying 12 different symptoms and clinical signs: nasal discharge, cough, fever/feels hot, conjunctivitis, fast breathing, wheezing, hoarseness, skin rash, reduced appetite, vomiting, diarrhoea (>3 watery stools/day), general malaise and space to provide information about doctor’s visits, hospital admissions and medicine. Parents were encouraged to complete the diary every day. Children were monitored through monthly home visits by a paediatrician (MLL), a study nurse or a study physician. At every home visit, children had a nasal swab taken, the symptom diary from the preceding month was collected and any queries were rectified.
At the first home visit, the parents were interviewed about household contacts, parents’ education and employment, ethnicity, birth weight of the child, breastfeeding, dispositions (hay fever, asthma and atopic dermatitis) and exposures (smoking in homes, smoking during pregnancy, pets, moisture, carpets, drying clothes inside). Questions concerning factors that could change over time were repeated every second month. Socioeconomic status was classified according to the Danish social classification system, choosing the social group which comes first in the order 1 to 5 in families where the mother and father were classified in two different categories [16].
Definition of illness episode
An hMPV and RSV illness episode included the day of the hMPV or RSV-positive test, and was defined as time from first day with symptoms to last day with symptoms without symptom-free days in the period. All symptoms occurring during the episode were considered associated with the hMPV or RSV infection. If symptoms persisted for more than 1 month, and an hMPV or RSV-negative nasal swab specimen was available from the month before or the month after the positive test, the episode was considered terminated on the dates of collecting the negative samples.
Specimen collection
Nasal swabs were obtained from both nostrils in children younger than 6 months of age, and from one nostril in older children. Samples were collected from a depth of 2 to 3 cm by using a sterile thin cotton swab on an aluminium shaft that was then placed into a vial containing 1 ml of viral transport medium (bovine serum albumin and antibiotics in phosphate-buffered saline [PBS]). Approximately 80% of specimens were frozen at −80°C within 7 hours. On some occasions the parents were instructed in sampling technique, and sent the samples by mail to the laboratory. On arrival, these samples were initially stored at +4°C and frozen at −80°C within 1 day of collection. We evaluated the sensitivity of the nasal swabs compared with nasopharyngeal aspirates (NPA) in 20 children hospitalised with RSV infection. We found RSV RNA in all samples by reverse transcription-polymerase chain reaction (RT-PCR), although most nasal swabs contained lower amounts of viral RNA.
Blood samples were collected from the mothers as soon as their child was enrolled in the study, and from children at age 5 days and 12 months. Samples were centrifuged at 3000 rpm for 10 min, and divided into cells and plasma.
RSV enzyme-linked immunosorbent assay (ELISA)
ELISA was used to determine anti-RSV IgG in plasma from mothers shortly after delivery and from 1-year-old children. Ninety-six-microwell, high-binding, half-area ELISA plates (Corning) were coated with 50 μl of 2 μg/ml purified RSV antigen (8RSV79, HyTest, Finland) in 50 mM carbonate buffer (pH 9.6), and incubated overnight at +4°C. The plates were washed two times with PBS containing 0.05% Tween-20 (Merck KGaA), and blocked for 75 min at room temperature (RT) with PBS containing 2% skim milk powder (M-PBS). Plates were washed, and serial dilutions of the positive control (3.86 mg/ml) were added, together with plasma samples diluted 1:1000 (maternal samples) or 1:100 (children’s samples) in M-PBS and a negative control (M-PBS). Samples were measured in duplicate. Plates were incubated for 1 h at RT. Next, plates were washed four times and incubated for 1 h at RT with horseradish peroxidase (HRP)-conjugated goat-anti-human IgG (Star 106P, AbD Serotec, UK) diluted 1:3000 in M-PBS. The plates were washed again four times, and antibodies were detected by adding 50 μl of 3,3′, 5,5′- tetramethyl benzidine (TMB) substrate (AdB Serotec, UK). After 10 min, the reaction was stopped using 50 μl of 1 M H2SO4. The extinction was measured at 450 nm.
Logarithmic standard curves were generated for the RSV ELISA with a coefficient of regression of 0.98 and an interassay variation ranging from 0 to 25%, with a mean coefficient of variation (CV) of 10%. Intraassay repeatability was measured on duplicate samples with a mean CV of 6.3%.
hMPV ELISA
hMPV antigen was prepared by sonicating infected LLC-MK2 cells in 50 mM carbonate buffer (pH 9.6). Sonicated cell pellet from the same cell line negative for hMPV was prepared the same way and used as negative control antigen. As positive and negative controls, we used sera from two anti-hMPV IgG-positive persons and two anti-hMPV IgG-negative persons respectively. ELISA plates were coated in every second well with 50 μl of hMPV antigen and 50 μl of negative control antigen respectively, diluted 1:200 in 50 mM carbonate buffer (pH 9.6) and incubated overnight at +4°C. The plates were washed three times with PBS containing 0.25% Tween-20. Plasma samples and negative controls, diluted 1:100 in M-PBS, were added in addition with serial dilutions of the positive control, and plates were incubated for 1 h at RT. Next, plates were washed four times and incubated for 1 h at RT with HRP-conjugated goat-anti-human IgG. The plates were washed again four times, and the presence of hMPV antibodies were detected by adding 50 μl of TMB substrate and then 50 μl of 1 M H2SO4 to stop the reaction. The extinction was measured at 450 nm with a reference filter at 630 nm. Net optical density (OD) values were calculated as OD values for the antigen minus OD values for the control antigen. hMPV inter- and intraassay variation were 7.4% and 3.8% respectively, based on OD values.
The cut-off value of each hMPV and RSV assay was defined by adding 2 standard deviations (SD) to the mean OD of all negative sera.
Real-time RT-PCR analysis of hMPV and RSV
Nucleic acid purification was carried out using the Total Nucleic Acid Isolation Kit (Roche Applied Science, Mannheim, Germany) in combination with the Total NA Variable Elution Volume protocol on a MagNA Pure LC Instrument (Roche Applied Science) according to the instructions of the manufacturer. We used 190 μl of material for purification, which was eluted into a final volume of 100 μl. Prior to purification, 10 μl of phocine distemper virus (PDV) were added to the sample as an internal control, in a concentration titrated to yield a threshold cycle (Ct) value of approximately 32 upon real-time RT-PCR analysis. Positive and negative controls were included in purification and PCR procedures. Real-time RT-PCR analyses of hMPV, RSV-A, RSV-B and PDV from each sample were carried out in four separate reactions using the TaqMan EZ RT-PCR Kit (Applied Biosystems, Foster City, CA, USA). The sequences of hMPV primers and probes were as previously published [24]. The PCR analysis was performed on a 7500 Real-Time PCR System (Applied Biosystems). To confirm a successful purification and amplification and to assess any presence of PCR inhibitors in the sample, the actual Ct value of the PDV reaction for each sample was compared with the expected Ct value. Comparisons of PDV Ct values were made using the MedLab QC freeware programme.
All hMPV and RSV-positive samples were tested for co-infection with rhinoviruses, adenovirus, influenzaviruses A and B, parainfluenzaviruses 1–3, coronaviruses OC43, 229E, and NL63, by real-time PCR using a protocol, primer/probe mixes, and positive controls obtained from Bert Niesters, Erasmus Medical Centre, Rotterdam, The Netherlands. Analyses for coronavirus HKU1 and human bocavirus were performed by an in-house PCR at the Department of Microbiology, Hvidovre Hospital, Copenhagen, Denmark, by using the same system as described above.
Statistical methods
For comparisons between symptoms of the hMPV and RSV-positive children, Fisher’s exact test was used for discrete variables (number of children), and the non-parametric Mann-Whitney U-test for continuous variables (duration of symptoms and episodes).
Univariate logistic regression analysis was used to assess potential risk factors for the presence of anti-hMPV and anti-RSV IgG antibodies at age 1 year. Predictors with a p-value ≤0.1 were entered into a multiple logistic regression analysis. To reduce problems with co-linearity, only one or two variables from each group of covariates (social variables, smoking parameters, atopic dispositions, breastfeeding, siblings, crowding factors, and indoor environment) were included. From these common logistic regression models, backwards elimination of non-significant variables was performed using the Likelihood Ratio statistics until a p-level of less than 0.1 for all variables was reached. All analyses were adjusted for sex. To test for significant effect modifications between the effect of any significant variable and that of any other significant variable on the outcome, we performed formal statistical tests for primary interaction by generating interaction terms and using them as covariates in addition to the main effects on the independent variable. A p-value <0.05 was considered significant. Data were analysed by using the SPSS software version 13.0 for Windows.
Results
Study population
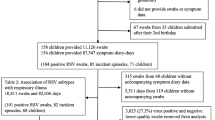
Of 336 children whose parents were invited to participate in the study, 242 were accepted, of whom 217 were followed throughout 1 year. Fourteen families dropped out within the first month, and 11 children dropped out during the year. Participating infants included eight pairs of twins. One child born in week 30 was treated in the neonatal intensive care unit with nasal-continuous positive airway pressure and tube feeding. This child remained in the study as no complications emerged. Characteristics of the study population are given in Table 1.
Anti-hMPV and anti-RSV IgG antibodies in children and mothers
To identify children who had experienced an hMPV or an RSV infection in the first year of life, we assumed that infected children developed an antibody response, which was measurable at age 12 months. Specific anti-hMPV and anti-RSV IgG was measured in plasma from the 217 children, who were followed throughout 1 year. Anti-RSV IgG antibodies were detected in 172 children (79%) (median 491 ng/ml, range 158–60.000 ng/ml) and anti-hMPV IgG was found in 38 children (17.5%) (median OD 0.44, range 0.094–1.216).
Blood samples were available from 241 mothers. All had detectable anti-RSV IgG (median 4106 ng/ml, range 1120–65.522 ng/ml) and anti-hMPV IgG (median OD 0.787, range 0.122–2.312).
Risk factors for hMPV infection
Dates of birth were divided into four quartiles according to seasonality. In both univariate and multiple logistic regression analyses, being born in the spring (March-May) compared to the rest of the year and having older siblings were significantly associated with increased risk of detectable anti-hMPV IgG at age 12 months, while drying clothes inside during the first 6 months of life protected against infection (Table 2).
Risk factors for RSV infection and hospitalisation
Risk factors for having detectable anti-RSV IgG by age 1 year differed from those associated with hMPV infection. In univariate analysis, gestational age <38 weeks, being born in the fall (September-November), increasing paternal age, and wall-to-wall carpeting were significantly associated with RSV infection, while being born in the spring protected against infection (Table 2). In multiple analysis, gestational age <38 weeks, increasing paternal age, wall-to-wall carpeting, and being born in the spring remained significant. The effect of increasing paternal age was not explained by an increasing number of older siblings. Maternal age was not significantly associated with RSV infection (OR = 1.4 per 5 yrs; 95% CI:0.96–2.05).
As a measure of severity, we looked specifically at risk factors for RSV hospitalisation (n = 11, 5.1%). In univariate analysis, smoking parameters (smoking during pregnancy, smoking in the household, number of cigarettes, number of smokers, maternal smoking, and paternal smoking) were significantly associated with increased risk of RSV hospitalisation, as were the number of children in the home and having older siblings. Full breastfeeding during the first 14 days protected against hospitalisation. In multiple analysis, breastfeeding for 14 days, having older siblings, and smoking in the household remained statistically significant (Table 2). Similar findings were observed when looking specifically at risk of hospitalisation among the anti-RSV IgG-positive children.
Clinical symptoms
Clinical symptoms associated with hMPV or RSV infection were evaluated using nasal swabs. Due to resource constraints, and as 89% of anti-hMPV IgG-positive children were also anti-RSV IgG-positive, we chose to analyse nasal swabs from the anti-hMPV IgG-positive children only to detect the time of primary hMPV or RSV infection. Of 474 samples from these children, 155 were taken within 3 days of respiratory symptoms. These 155 samples were in addition to 31 control specimens, taken at a time when the child had been free of respiratory symptoms and fever for at least 3 weeks prior to collection to 1 week after the sample was taken, analysed for RSV A, RSV B, and hMPV by RT-PCR.
We detected ten hMPV-positive and 15 RSV-positive nasal swabs from 24 different children, corresponding to 26.3% (ten out of 38) of the hMPV infections and 8.7% (15 out of 172) of the RSV infections. RSV-positive samples were identified from children down to 26 days of age, while primary hMPV infection was only seen in children older than 6 months. One hMPV-infected infant was asymptomatic. Co-infection with other respiratory viruses, primarily rhinovirus and human bocavirus, occurred in nine cases (Table 3). Information on clinical symptoms associated with single hMPV and RSV infections was obtained from the health diaries, and is illustrated in Table 4. The groups were too small to detect any statistically significant differences in distribution and duration of symptoms.
Discussion
The present study identifies risk factors for mild and asymptomatic hMPV infections within the first year of life in unselected healthy infants. We found that risk factors for hMPV and RSV infection were different, as were risk factors for mild and severe RSV infection. The prospective design of the study and the close contact to participating families through monthly home visits resulted in low drop-out rates, and ensured a high quality of information on risk factors and symptoms during infection.
Our population consists of healthy infants, and the risk factors found are valid for normal children. Children with high-risk conditions, such as bronchopulmonary dysplasia, prematurity, cystic fibrosis, and congenital heart diseases are more prone to severe infections, and the risk factors found in this study cannot be extrapolated to such children.
The risk of attracting hMPV infection was mainly determined by the presence of older siblings, who bring the virus to the family, but also by birth in the spring. Most studies on seasonality of hMPV have found that hMPV infection peaks during late winter/early spring (January-April) [1, 12, 27, 30], although some studies report that hMPV hospitalisation peaks in the early winter [9]. These studies also find that most children are infected after 6 months of age. Children born during spring in this cohort may mainly contract their hMPV infection at late ages (>10 months), explaining this finding. No other studies are directly comparable with ours, but studies including children with underlying pathologies have found prematurity, male gender, congenital heart disease, and gastrointestinal reflux and aspiration to be risk factors for hMPV hospitalisation [30]. In our study, gender was not a risk factor for hMPV infection.
Prematurity is a known risk factor for severe RSV infection, and even though we only included 19 babies born prematurely (weeks 30–37), we found that gestational age less than 38 weeks was associated with RSV infection, but not with hospitalisation. The effect of increasing paternal age on risk of RSV infection was new to us. The paternal age span ranged from 20–53 years, and the effect was especially noticeable among fathers older than 38 years. Young adults usually have the highest amounts of antibodies to respiratory viruses. With increasing age, antibody levels decline, making the individual more susceptible to new infections. An explanation could be that older fathers, due to low levels of RSV antibodies, become infected and transmit the virus to the child. However, we did not collect plasma samples from the fathers for antibody detection to confirm this theory. The same effect was not noticed for mother’s age, probably due to a smaller age span.
Birth into the RSV season increased infection rates, which has been reported by others [5, 20, 32]. However, this finding disappeared in multiple regression analysis, as the protective effect of being born in the spring was more pronounced. To our knowledge, the association between carpeting and RSV infection has not been described previously. It is not known whether the survival of RSV is greater on carpets than on smooth floors, but young children spend much time lying and crawling on the floor, and transmission from surfaces contaminated with RSV-infected nasal secretions is possible [14]. Maybe parents are more inclined to place their child directly on a carpet rather than on a cold floor, and maybe cleaning is easier achieved on the floor through rubbing. Factors highly associated with RSV hospitalisation were passive smoking and the presence of older siblings, while exclusive breastfeeding in the first 2 weeks of life was protective. This is in accordance with other studies of severe RSV infection [17, 26, 29].
The identification of children with a previous hMPV or RSV infection was based on IgG detection in plasma by age 1 year. In most children, maternal antibodies disappear within 6 months [4, 6, 7], and IgG detected after that age will be the result of natural infection. Some studies report that infants <6 months of age have poor serum antibody responses against RSV infection, making the use of seroepidemiological diagnosis difficult [4, 10, 41]. Other studies have found that almost all children <1 year of age generate an antibody response after their first RSV infection [31]. The seroprevalence of anti-RSV IgG in our cohort is at the higher end of what is usually reported, and seven children with proven RSV infection before 2 months of age all had detectable low levels of anti-RSV IgG by age 12 months, making the possibility of an underestimation unlikely. The seroprevalence of anti-hMPV IgG correlates well with the results of other studies [22].
The present study has certain limitations that need to be taken into account when considering the study and its contributions. The study was first and foremost designed to detect risk factors for hMPV and RSV infection in infancy. The sample size calculation for detection of differences in symptoms related to hMPV and RSV infection was based on the assumption that all hMPV and RSV infections were identified during the study period. However, we did not identify time of infection for the majority of IgG-positive children. The clinical symptoms related to hMPV and RSV infection in young children in the community in this study is therefore descriptive in nature. Shedding durations of RSV and hMPV in nasal secretions after an acute infection have been reported to be 11.5 and 5 days respectively [38]. Therefore, nasal swab specimens taken more often than once a month would be preferable to identify the time of primary infection. However, for ethical and practical reasons, this was not possible in the present study. Collecting nasal swabs at regular monthly intervals made it possible to identify a quarter of the hMPV infections. We used this method to avoid the risk of bias and underreporting by parents if they actively had to contact us for every respiratory episode, which has been the case in other studies [8].
Nasal swabs may not be as sensitive as NPA in detecting RSV [18, 23, 34]. However, a recent study reports that when a sensitive amplification method like RT-PCR is used for RSV analysis, the sensitivity of nasal swabs is comparable to that of NPA [40]. The swabs were chosen, as they were sensitive in our own test of RSV in hospitalised infants, and as they were much more appropriate for this epidemiological survey collecting 13 samples from each child’s nose.
In conclusion, this study provides information on risk factors for mild and asymptomatic hMPV infections in unselected healthy infants, and helps identify children at risk of an early infection.
Abbreviations
- hMPV:
-
human metapneumovirus
- RSV:
-
respiratory syncytial virus
- OR:
-
odds ratio
- PBS:
-
phosphate-buffered saline
- NPA:
-
nasopharyngeal aspirate
- RT-PCR:
-
reverse transcription-polymerase chain reaction
- ELISA:
-
enzyme-linked immunosorbent assay
- RT:
-
room temperature
- M-PBS:
-
PBS with 2% skim-milk powder
- HRP:
-
horseradish peroxidase
- TMB:
-
tetramethyl benzidine
- OD:
-
optical density
- SD:
-
standard deviation
- PDV:
-
Phocine Distemper Virus
- Ct:
-
threshold cycle
- CV:
-
coefficient of variation
- CI:
-
confidence interval
References
Al-Sonboli N, Hart CA, Al-Aeryani A, Banajeh SM, Al-Aghbari N, Dove W, Cuevas LE (2005) Respiratory syncytial virus and human metapneumovirus in children with acute respiratory infections in Yemen. Pediatr Infect Dis J 24:734–736
Aujard Y, Fauroux B (2002) Risk factors for severe respiratory syncytial virus infection in infants. Respir Med 96 Suppl B:S9–14
Boivin G, De Serras G, Côté S, Gilca R, Abed Y, Rochette L, Bergeron MG, Déry P (2003) Human metapneumovirus infections in hospitalized children. Emerg Infect Dis 9:634–640
Brandenburg AH, Groen J, van Steensel-Moll HA, Claas EC, Rothbarth PH, Neijens HJ, Osterhaus AD (1997) Respiratory syncytial virus specific serum antibodies in infants under six months of age: limited serological response upon infection. J Med Virol 52:97–104
Cilla G, Sarasua A, Montes M, Arostegui N, Vicente D, Perez-Yarza E, Perez-Trallero E (2006) Risk factors for hospitalization due to respiratory syncytial virus infection among infants in the Basque Country, Spain. Epidemiol Infect 134:506–513
Cox MJ, Azevedo RS, Cane PA, Massad E, Medley GF (1998) Seroepidemiological study of respiratory syncytial virus in Sao Paulo state. Brazil J Med Virol 55:234–239
Crowe Jr JE, Williams JV (2003) Immunology of viral respiratory tract infection in infancy. Paediatr Respir Rev 4:112–119
de Waal L, Koopman LP, van Benten IJ, Brandenburg AH, Mulder PG, de Swart RL, Fokkens WJ, Neijens HJ, Osterhaus AD (2003) Moderate local and systemic respiratory syncytial virus-specific T-cell responses upon mild or subclinical RSV infection. J Med Virol 70:309–318
Døllner H, Risnes K, Radtke A, Nordbø SA (2004) Outbreak of human metapneumovirus infection in norwegian children. Pediatr Infect Dis J 23:436–440
Forster J, Streckert HJ, Werchau H (1995) The humoral immune response of children and infants to an RSV infection: its maturation and association with illness. Klin Padiatr 207:313–316
Garcia-Garcia ML, Calvo C, Casas I, Bracamonte T, Rellan A, Gozalo F, Tenorio T, Perez-Brena P (2007) Human metapneumovirus bronchiolitis in infancy is an important risk factor for asthma at age 5. Pediatr Pulmonol 42:458–464
Garcia-Garcia ML, Calvo C, Martin F, Perez-Brena P, Acosta B, Casas I (2006) Human metapneumovirus infections in hospitalised infants in Spain. Arch Dis Child 91:290–295
Glezen WP, Taber LH, Frank AL, Kasel JA (1986) Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child 140:543–546
Hall CB (1977) The shedding and spreading of respiratory syncytial virus. Pediatr Res 11:236–239
Hamelin ME, Abed Y, Boivin G (2004) Human metapneumovirus: a new player among respiratory viruses. Clin Infect Dis 38:983–990
Hansen EJ (1984) [Socialgrupper i Danmark] (Danish). Socialforskningsinstituttet. Studie 48.
Hayes EB, Hurwitz ES, Schonberger LB, Anderson LJ (1989) Respiratory syncytial virus outbreak on American Samoa. Evaluation of risk factors. Am J Dis Child 143:316–321
Heikkinen T, Marttila J, Salmi AA, Ruuskanen O (2002) Nasal swab versus nasopharyngeal aspirate for isolation of respiratory viruses. J Clin Microbiol 40:4337–4339
Henderson J, Hilliard TN, Sherriff A, Stalker D, Al Shammari N, Thomas HM (2005) Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol 16:386–392
Holberg CJ, Wright AL, Martinez FD, Ray CG, Taussig LM, Lebowitz MD (1991) Risk factors for respiratory syncytial virus-associated lower respiratory illnesses in the first year of life. Am J Epidemiol 133:1135–1151
Lemanske RF (2004) Viral infections and asthma inception. J Allergy Clin Immunol 114:1023–1026
Ljubin SS, Vilibic CT, Falsey AR, Walsh EE, Mlinaric GG (2006) Serosurvey of human metapneumovirus infection in Croatia. Croat Med J 47:878–881
Macfarlane P, Denham J, Assous J, Hughes C (2005) RSV testing in bronchiolitis: which nasal sampling method is best? Arch Dis Child 90:634–635
Maertzdorf J, Wang CK, Brown JB, Quinto JD, Chu M, de Graaf M, van den Hoogen BG, Spaete R, Osterhaus AD, Fouchier RA (2004) Real-time reverse transcriptase PCR assay for detection of human metapneumoviruses from all known genetic lineages. J Clin Microbiol 42:981–986
Morrow BM, Hatherill M, Smuts HE, Yeats J, Pitcher R, Argent AC (2006) Clinical course of hospitalised children infected with human metapneumovirus and respiratory syncytial virus. J Paediatr Child Health 42:174–178
Nielsen HE, Siersma V, Andersen S, Gahrn-Hansen B, Mordhorst CH, Norgaard-Pedersen B, Roder B, Sorensen TL, Temme R, Vestergaard BF (2003) Respiratory syncytial virus infection - risk factors for hospital admission: a case-control study. Acta Paediatr 92:1314–1321
Ordás J, Boga JA, Alvarez-Argüelles M, Villa L, Rodriguez-Dehli C, de Oña M, Rodríguez J, Melón S (2006) Role of metapneumovirus in viral respiratory infections in young children. J Clin Microbiol 44:2739–2742
Peiris JS, Tang WH, Chan KH, Khong PL, Guan Y, Lau YL, Chiu SS (2003) Children with respiratory disease associated with metapneumovirus in Hong Kong. Emerg Infect Dis 9:628–633
Pullan CR, Toms GL, Martin AJ, Gardner PS, Webb JK, Appleton DR (1980) Breast-feeding and respiratory syncytial virus infection. Br Med J 281:1034–1036
Robinson JL, Lee BE, Bastien N, Li Y (2005) Seasonality and clinical features of human metapneumovirus infection in children in Northern Alberta. J Med Virol 76:98–105
Roca A, Quinto L, Abacassamo F, Loscertales MP, Gomez-Olive FX, Fenwick F, Cane PA, Saiz JC, Toms G, Alonso PL (2003) Antibody response after RSV infection in children younger than 1 year of age living in a rural area of Mozambique. J Med Virol 69:579–587
Rossi GA, Medici MC, Arcangeletti MC, Lanari M, Merolla R, Paparatti UD, Silvestri M, Pistorio A, Chezzi C (2007) Risk factors for severe RSV-induced lower respiratory tract infection over four consecutive epidemics. Eur J Pediatr 166:1267–1272
Schauer U, Hoffjan S, Bittscheidt J, Kochling A, Hemmis S, Bongartz S, Stephan V (2002) RSV bronchiolitis and risk of wheeze and allergic sensitisation in the first year of life. Eur Respir J 20:1277–1283
Stensballe LG, Trautner S, Kofoed PE, Nante E, Hedegaard K, Jensen IP, Aaby P (2002) Comparison of nasopharyngeal aspirate and nasal swab specimens for detection of respiratory syncytial virus in different settings in a developing country. Trop Med Int Health 7:317–321
van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, Osterhaus AD (2001) A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med 7:719–724
van den Hoogen BG, van Doornum GJ, Fockens JC, Cornelissen JJ, Beyer WE, de Groot R, Osterhaus AD, Fouchier RA (2003) Prevalence and clinical symptoms of human metapneumovirus infection in hospitalized patients. J Infect Dis 188:1571–1577
Viazov S, Ratjen F, Scheidhauer R, Fiedler M, Roggendorf M (2003) High prevalence of human metapneumovirus infection in young children and genetic heterogeneity of the viral isolates. J Clin Microbiol 41:3043–3045
von Linstow ML, Eugen-Olsen J, Koch A, Winther TN, Westh H, Høgh B (2006) Excretion patterns of human metapneumovirus and respiratory syncytial virus among young children. Eur J Med Res 11:329–335
von Linstow ML, Larsen HH, Eugen-Olsen J, Koch A, Winther TN, Meyer AM, Westh H, Lundgren B, Melbye M, Høgh B (2004) Human metapneumovirus and respiratory syncytial virus in hospitalized danish children with acute respiratory tract infection. Scand J Infect Dis 36:578–584
Waris M, Heikkinen T, Osterback R, Jartti T, Ruuskanen O (2007) Nasal swabs for detection of respiratory syncytial virus RNA in children. Arch Dis Child 92:1046–1047
Wilczynski J, Lukasik B, Torbicka E, Tranda I, Brzozowska-Binda A (1994) The immune response of small children by antibodies of different classes to respiratory syncytial virus (RSV) proteins. Acta Microbiol Pol 43:369–379
Wilkesmann A, Schildgen O, Eis-Hubinger AM, Geikowski T, Glatzel T, Lentze MJ, Bode U, Simon A (2006) Human metapneumovirus infections cause similar symptoms and clinical severity as respiratory syncytial virus infections. Eur J Pediatr 165:467–475
Wolf DG, Zakay-Rones Z, Fadeela A, Greenberg D, Dagan R (2003) High seroprevalence of human metapneumovirus among young children in Israel. J Infect Dis 188:1865–1867
Acknowledgements
We are grateful to the participating children and parents. We thank Karina Larsen and Nanna Lietmann who assisted in collecting the samples, Bodil Landt and Anne-Marie Meyer for performing the nucleic acid extractions and the RT-PCR assays, and Klaus Larsen for useful discussions on the statistical analyses. Johan Lantto, Symphogen A/S, Denmark graciously provided the RSV ELISA protocol and positive and negative controls, and primer/probe mixes for the PCR analyses were kindly provided by Bert Niesters, Erasmus Medical Centre, Rotterdam, The Netherlands. This research was funded by grants from the Pharmacists’ Foundation, Rosalie Petersen’s Foundation, Ebba Celinder’s Foundation, Aase and Ejnar Danielsen’s Foundation, Hvidovre Hospital’s Research Fund, the Research Fund of Queen Louise’s Children’s Hospital, and the Gangsted Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
von Linstow, ML., Høgh, M., Nordbø, S.A. et al. A community study of clinical traits and risk factors for human metapneumovirus and respiratory syncytial virus infection during the first year of life. Eur J Pediatr 167, 1125–1133 (2008). https://doi.org/10.1007/s00431-007-0643-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0643-4