Abstract
Recent investigation of the intestine following ischemia and reperfusion (I/R) has revealed that nitric oxide synthase (NOS) neurons are more strongly affected than other neuron types. This implies that NO originating from NOS neurons contributes to neuronal damage. However, there is also evidence of the neuroprotective effects of NO. In this study, we compared the effects of I/R on the intestines of neuronal NOS knockout (nNOS−/−) mice and wild-type mice. I/R caused histological damage to the mucosa and muscle and infiltration of neutrophils into the external muscle layers. Damage to the mucosa and muscle was more severe and greater infiltration by neutrophils occurred in the first 24 h in nNOS−/− mice. Immunohistochemistry for the contractile protein, α-smooth muscle actin, was used to evaluate muscle damage. Smooth muscle actin occurred in the majority of smooth muscle cells in the external musculature of normal mice but was absent from most cells and was reduced in the cytoplasm of other cells following I/R. The loss was greater in nNOS−/− mice. Basal contractile activity of the longitudinal muscle and contractile responses to nerve stimulation or a muscarinic agonist were reduced in regions subjected to I/R and the effects were greater in nNOS−/− mice. Reductions in responsiveness also occurred in regions of operated mice not subjected to I/R. This is attributed to post-operative ileus that is not significantly affected by knockout of nNOS. The results indicate that deleterious effects are greater in regions subjected to I/R in mice lacking nNOS compared with normal mice, implying that NO produced by nNOS has protective effects that outweigh any damaging effect of this free radical produced by enteric neurons.
Similar content being viewed by others
Introduction
Nitric oxide (NO) is a free radical involved in numerous biological functions, including vasodilation, transmission from inhibitory neurons to gut muscle, modulation of neurotransmission, inhibition of platelet aggregation and inhibition of smooth muscle proliferation (Love 1999; Moro et al. 2004). NO is synthesized from L-arginine by the activity of nitric oxide synthases (NOS; Love 1999; Mallick et al. 2004; Moro et al. 2004). All three isoforms of NOS have been identified in the intestine: endothelial NOS (eNOS), neuronal NOS (nNOS) and inducible NOS (iNOS; Torihashi et al. 1996; McCafferty et al. 1999; Mallick et al. 2004). Interestingly, neurons containing eNOS are more susceptible to damage than other enteric neurons in a number of enteric neuropathies, including esophageal achalasia, hypertrophic pyloric stenosis and gastroparesis (Rivera et al. 2011a).
Damage following ischemia and reperfusion (I/R) injury is common in the intestine and can be caused during abdominal surgery, in several disease states and following intestinal transplantation (Granger and Korthuis 1995). I/R results in initial tissue damage and in prolonged changes in motility, most often involving slowed transit, implying that properties of motility-controlling neurons are altered. We have previously reported that a brief period of ischemia followed by reperfusion causes damage selectively to nNOS neurons (Rivera et al. 2009, 2011b). nNOS-immunoreactive neurons, which have been identified as inhibitory motor neurons and descending interneurons in the mammalian enteric nervous system, are significantly swollen and distorted after 24 h of reperfusion following a period of ischemia, with the neuronal changes persisting for at least 4 weeks (Rivera et al. 2009), although changes in the muscle and mucosa are repaired by 1 week (Pontell et al. 2011). A substantial increase of nitrosylated proteins also occurs after I/R (Rivera et al. 2011b). Tyrosine residues in proteins are nitrosylated at position 3 by peroxynitrites that are formed from NO and reactive oxygen species (Ferrer-Sueta and Radi 2009). The nitrosylation compromises protein activity and leads to deficits in cell function. We have found extensive accumulations of nitrosylated proteins in the intestine within 1 h after I/R. The nitrosylated protein is cleared over a period of about 2 days.
Our previous investigation of I/R indicated that NO, probably originating from NOS neurons, contributed to protein degradation and cell damage (Rivera et al. 2011b). However, good evidence has been presented that NO has dual protective and damaging roles when an ischemic challenge is made to the brain (Lipton 1999; Moro et al. 2004; Woodruff et al. 2011) and to the intestine (Miller et al. 1994; Masuda et al. 1995; Pfeiffer and Qiu 1995; McCafferty et al. 1999). The present work has been undertaken to investigate the role of neuronally produced NO in the tissue damage that occurs after I/R, by investigating changes in nNOS knockout (nNOS−/−) mice. We have also investigated changes in neuromuscular function, which has not been previously studied in this model of intestinal I/R.
Materials and methods
Mice homozygous for targeted disruption of the nNOS gene (Huang et al. 1993) from an established colony at the Department of Anatomy and Neuroscience at the University of Melbourne were used. The colony was established by backcrossing nNOS−/− mice, purchased from Jackson Laboratories (Bar Harbor, Me., USA; stock no. 002633) onto a C57BL/6 background. Male and female nNOS−/− and nNOS+/+ littermates (8–12 weeks of age) were used in all experiments. All procedures were conducted according to the National Health and Medical Research Council of Australia guidelines and were approved by the University of Melbourne Animal Experimentation Ethics Committee. We studied at least three mice in each group in experiments leading to histological or immunohistochemical evaluation, whereas six mice per group were examined in the functional studies.
Induction of ischemia
Mice were anesthetized with a mixture of xylazine (20 mg/kg; Troy Laboratories, Sydney, Australia) and ketamine hydrochloride (100 mg/kg; Troy Laboratories) diluted in sterile phosphate-buffered saline (PBS), given subcutaneously. A loop of ileum (approximately 5 cm long) that was supplied by a single branch of the superior mesenteric artery was exteriorized, ligatures were tightly applied to the marginal arteries and veins to prevent blood flow between the segment subjected to I/R and the adjacent regions and the mesenteric artery and vein supplying the segment were occluded for 120 min with an atraumatic vascular clamp. Prompt restoration of flow was achieved by dripping lidocaine (1% in saline; Troy Laboratories) onto the region of occlusion immediately after removing the clamp.
Animals were taken at 3 and 24 h after occlusion. Tissue was sampled from the region subjected to ischemia (occluded region) and from a non-ischemic (non-occluded) region, 4–6 cm oral to the ischemic region. Tissue was also taken from sham-operated mice and from unoperated mice. Sham operations followed the same procedures, except that the ties on marginal vessels were not tightened and the atraumatic vascular clamp was not closed. The sham-occluded and sham-non-occluded regions were taken after 24 h, this being the time point of maximum effect of I/R.
Histology
At the time of taking tissue, animals were killed by cervical dislocation. The occluded and non-occluded regions were removed and placed in PBS (0.15 M NaCl in 0.01 M sodium phosphate buffer, pH 7.2) containing nicardipine (10-6 M; Sigma, Sydney, Australia). The ileum was cleaned of its contents, opened along the mesenteric attachment, pinned (mucosa down) to balsa wood sheets without being stretched and fixed in 2% formaldehyde plus 0.2% picric acid in 0.1 M sodium phosphate buffer, pH 7.2, at 4°C. Each sample was placed in a histology cassette, dehydrated through graded ethanol to histolene and embedded in paraffin. Sections were cut transversely at a thickness of 5 μm and processed for standard hematoxylin and eosin (H&E) staining. Following the staining step, the tissue was mounted by using a permanent mounting medium. Preparations were examined on a Zeiss microscope fitted with an Axio-Cam imaging system.
Immunohistochemistry
Occluded and non-occluded segments of intestine were opened along the mesenteric border and pinned (mucosa down) to balsa wood sheets for fixation in 2% formaldehyde plus 0.2% picric acid in 0.1 M sodium phosphate buffer, pH 7.2, at 4°C. Preparations were cleared of fixative by 3×10 min washes in dimethyl sulfoxide (DMSO) followed by 3×10 min washes in PBS. Fixed tissue was stored at 4°C in PBS containing sodium azide (0.1 %) and 30% sucrose as a cryoprotectant (PBS-sucrose-azide). The following day, tissue was transferred to a mixture of PBS-sucrose-azide and OCT compound (Tissue Tek, Elkhart, Ind., USA) at a ratio of 1:1 for a further 24 h before being embedded in 100% OCT. Sections (12 μm thick) were cut, collected on 1% gelatinized slides, left to dry for 1 h at room temperature and then incubated with rabbit anti-α-smooth muscle actin (SMA; 1;1000; Abcam, Cambridge, UK) or vasoactive intestinal peptide (VIP; 1:400; Furness and Costa 1979) overnight at 4°C. The sections were washed for 3×10 min in PBS prior to the secondary antibody incubation with donkey anti-rabbit 488 (Molecular Probes, Eugene, Ore., USA), diluted 1:500, for 1 h at room temperature. Sections were washed 3×10 min in PBS prior to a 10-min incubation with 4,6-diamidino-2-phenylindole (DAPI; Invitrogen, Melbourne, Australia), diluted 1:1000, at room temperature. Three subsequent 10-min washes in PBS were carried out and sections were then mounted in a S3023 non-fluorescent mounting medium (Dako, Carpinteria, Calif., USA).
SMA-immunoreactive cells were counted in the longitudinal muscle layer. Data are expressed as the number of SMA-immunoreactive cells per section, per length of ileum.
Myeloperoxidase reaction
Segments of intestine were opened along the mesenteric border, pinned (mucosa down) to balsa wood sheets, fixed in 100% ethanol for 10 min, subjected to 3×10 min PBS washes and then stored in PBS-sucrose (PBS containing 30% sucrose) overnight at 4°C. The following day, the tissue was transferred in a solution of 50% OCT, 50% PBS-sucrose-azide. On the next day, the tissue was embedded in OCT, snap-frozen in isopentane that was cooled in liquid nitrogen and stored at −20°C until required. Ileum sections of 12 μm thickness, spaced 12 μm apart, were cut and collected on 1% gelatinized slides and left to dry for 1 h at room temperature before being covered in PBS until ready for staining.
Preparations were stained in Hanker-Yates solution consisting in a 0.6 mg/ml Hanker-Yates reagent (p-phenylenediamine plus pyrocatechol; Polysciences, Warrington, Pa., USA) and 0.003% H2O2 in PBS for 10 min to detect the presence of myeloperoxidase (MPO) in neutrophils (Kalff et al. 1998b). Following 3×5 min washes in PBS, the tissue was counterstained with 2% methylene green for 30 s. Preparations underwent further washes in ethanol and histolene and were then mounted in DPX.
Neutrophils that were localized by using the MPO reaction were counted in three compartments: the longitudinal muscle/myenteric plexus, the circular muscle and the submucosa/intestinal glands. Neutrophils observed in the villi were not counted because of the disruption and loss of villi that occurred at early time points. Data are expressed as the number of MPO-positive cells per section, per length of ileum.
Isometric tension recording
Full-thickness ileal segments (2 cm long) were prepared and mounted longitudinally in 20-ml organ baths containing Krebs’ physiological saline solution of the following composition (in mmol/l): 118 NaCl, 4.8 KCl, 2.5 NaHCO3, 25 NaH2PO4, 1.1 MgSO4, 11.1 D-glucose, 2.5 CaCl2. The physiological saline also contained indomethacin (1 μM, Sigma-Aldrich) to inhibit the production of prostaglandins. The baths were aerated with 95% O2:5% CO2 and maintained at 35-37°C. A resting tension of 1 g was applied to the tissues and isometric responses were recorded with a force transducer and displayed by using the Chart program (ADInstruments, Sydney, Australia). Tissues were allowed to equilibrate for at least 10 min and frequency response curves to electrical field stimulation (EFS; 2, 5, and 20 Hz, 0.5-ms pulse width, 100 pulses, 60 V) were obtained before the addition of drugs. Carbachol (0.1, 1, and 10 μM; Sigma-Aldrich) was also tested cumulatively. Tissues were additionally preincubated with tetrodotoxin (TTX; 1 μM; Alomone Labs, Jerusalem, Israel) for 10 min prior to EFS. All isometric tension recording data were analyzed by using Chart v7.
Imaging
Preparations were analyzed by confocal microscopy on a Zeiss Meta or Zeiss Pascal confocal laser scanning system. Fluorophores were visualized by using a 488-nm excitation filter with a 522/535-nm emission filter for Alexa 488 and by means of 568-nm excitation with 605/632-nm emission filters for Texas Red. Z-series images and single 1024×1024 pixel images (optical sections of 0.5 μm nominal thickness) were captured.
Statistical analysis
Data were evaluated by two-way analysis of variance (ANOVA) followed by the Tukey post-hoc test for multiple comparisons between groups. Analyses were performed with Graph Pad Prism (Graph Pad Software, San Diego, Calif., USA). All data are represented as means ± standard error of the mean (SEM). Differences were considered statistically significant at P<0.05.
Results
General observations
During the period of occlusion, the intestinal region that was deprived of blood flow became purple. After blood flow was restored, the tissue resumed its normal pink color. The animals recovered from anesthesia uneventfully and once they were awake, the mice were active and ate normally. The regions subjected to ischemia were reddened in samples taken at 3 and 24 h, whereas the remainder of the intestine was macroscopically normal.
Histological observations
After 3 h reperfusion
The histological studies showed that damage was more severe in nNOS−/− compared with nNOS+/+ mice (Fig. 1).
Histological changes following ischemia/reperfusion injury in nNOS−/− and nNOS+/+ mice. a In sham-operated animals, the villi and circular and longitudinal muscle had normal structure after 24 h (24hr sham). b After 3 h reperfusion (3hr rep), the stumps of the villi were commonly sealed off with cuboidal epithelium in nNOS+/+ mice (nNOS+/+). c In nNOS−/− mice (nNOS−/−), the ends of the villi were still missing and active bleeding occurred into the lumen following 3 h reperfusion. Tissue debris can be seen in the lumen. d In sham-operated animals, the circular (CM) and longitudinal muscle (LM) exhibited a regular appearance. e After 3 h reperfusion, the CM was relatively intact in nNOS+/+ mice. f In nNOS−/− mice after 3 h reperfusion, the CM was severely affected and contained numerous damaged CM cells. g After 24 h reperfusion (24hr rep), the LM was relatively intact in nNOS+/+ mice. h Severe LM degeneration took place in nNOS−/− mice following 24 h reperfusion and this layer was replaced by numerous nucleated cells that appeared to be a mixture of immune cells and fibroblasts. Bars 100 μM (a), 50 μM (b-h)
In nNOS−/− mice, the ends of the villi were missing and active bleeding was noted from the majority of villi into the lumen (Fig. 1c). Tissue debris was found in the lumen. The bases of the glands were intact and Paneth cell granules were prominent. The circular muscle contained numerous severely damaged muscle cells (Fig. 1f). The surface membranes of the cells could be recognized but the interiors of the cells were almost empty, except for small aggregates of residual cytoplasm that were almost always centrally located (Fig. 1f). Nuclear profiles were seen in some of these clear cells. The severe damage with clear cytoplasm was in the outer component of the circular muscle layer. The inner circular muscle layer, which contains specialized smooth muscle cells (Gabella 1974), was much less affected and cells with clear cytoplasm were not seen in this layer. Muscle cells with clear cytoplasm were also found in the longitudinal layer but these were fewer than those in the circular layer. The myenteric ganglia had a foamy appearance of the neuropil. The clear spaces in the neuropil were commonly larger and more prominent than sometimes occurs following imperfect fixation. The majority of nerve cells were affected and showed various features of nerve cell damage including foamy cytoplasm, irregular shapes, nuclei displaced to the edges of cells and pyknotic nuclei. Damage to submucosal neurons was less obvious but some neurons were swollen. Eosinophils and neutrophils were also present at the level of the myenteric ganglia, whereas in control tissues, none were associated with myenteric ganglia.
In nNOS+/+ mice, the ends of the villi were lost but the prominent micro-hemorrhages were not seen. Some accumulations of blood cells were found in the surviving mucosa. The stumps of the villi were commonly sealed off with cuboidal or low columnar epithelium, indicative of mucosal repair (Fig. 1b). Muscle damage was less than that in nNOS−/− mice. The number of muscle cells with clear cytoplasm in the circular muscle layer was much fewer but the small amount of damage in the longitudinal muscle was similar to that in the nNOS−/− mice (Fig. 1). Little evidence of myenteric neuron damage was evident. Some foaminess of the neuropil was detected but this was less obvious than that in nNOS−/− mice. Slight loss of cytoplasmic integrity in submucosal neurons also occurred. Neutrophils and eosinophils seen in histological sections were few at the level of the myenteric plexus. Neutrophil numbers were quantified by using the MPO histochemical technique (see below).
After 24 h reperfusion
In nNOS−/− mice, the mucosal surface epithelium was restored, although the villous tips were sometimes irregular. Swelling of the central lacteals and of the surrounding lamina propria was seen and was present in all or nearly all villi. The villi were shorter than normal and some trapped hemorrhagic foci were detected in the villi. The residual circular muscle was thin, generally being only 2–3 cells thick (Fig. 1h). This might have been surviving internal circular muscle. The longitudinal muscle contained few cells that could be recognized as smooth muscle cells (Fig. 1h) but exhibited numerous nucleated cells with little cytoplasmic staining. These appeared to be a mixture of fibroblasts, lymphocytes and other immune cells. The myenteric nerve cells that survived at 24 h had normal nuclei and a clearer than normal cytoplasm.
In nNOS+/+ mice, the villi had regrown, were covered in epithelium and were longer than in nNOS−/− mice but some distortion was noted at the tips. Few micro-hemorrhages were observed. The muscle layers were thicker (especially the circular muscle) than in the nNOS−/− mice and were relatively intact (Fig. 1g). Enteric neurons had normal nuclei but some had a clearer than usual cytoplasm. Some lymphocytes were also found at the serosal surface.
Neutrophil Infiltration
Neutrophils were revealed by the MPO reaction and were counted in three compartments: (1) the longitudinal muscle plus the myenteric plexus, (2) the circular muscle, (3) the submucosal plexus plus the base of the mucosa. Neutrophils were not counted in the villi because of the loss of this part of the ileal wall at 3 h (Fig. 1). In animals that had been subjected to no treatments (absolute controls), no neutrophils were found attached to the serosa, in the longitudinal muscle, associated with myenteric ganglia, or in the circular muscle. In the regions subjected to I/R, numerous neutrophils were associated with the longitudinal and circular muscle at 24 h (Fig. 2). The numbers of neutrophils were significantly higher in nNOS−/− compared with nNOS+/+ mice (P<0.05). These occurred at the serosal surface, through the thickness of the muscle layer and close to the myenteric ganglia (Fig. 2). No indication of preferential targeting of the ganglia or muscle was detected. Small numbers of neutrophils were also found in the longitudinal and circular muscle layers of non-occluded segments of ileum, 5 cm proximal to the site subjected to I/R injury and in segments of ileum from sham-operated animals (Fig. 3). Neutrophil also infiltrated the submucosa and mucosa after surgery, in the regions subjected to I/R, oral to this region and in the sham controls. This infiltration appeared to be distributed randomly in the mucosa and submucosa compartment (Figs. 2, 3).
Neutrophils revealed by myeloperoxidase (MPO) histochemistry (dark brown cells). a, d In sham-operated mice, neutrophils were confined to the mucosa and submucosa; few or none were present in the circular or longitudinal muscle but they occurred adjacent to mucosal glands. b, e After 3 h reperfusion, neutrophils were common in the mucosa from occluded and non-occluded regions of nNOS−/− and nNOS+/+ mice. c, f After 24 h reperfusion, neutrophils were common in both the mucosa and muscle of occluded regions in both nNOS−/− and nNOS+/+ mice. However, more neutrophils were apparent in nNOS−/− mice. Bar 50 μM
Numbers of neutrophils per millimetre length of intestine. Neutrophil numbers in the longitudinal (a) and circular muscle (b) layers following 24 h reperfusion were significantly increased in the occluded regions (occ) when compared with the absolute control (Absolute Control) and sham-operated (sham) animals (*). Neutrophil numbers were also significantly higher in nNOS−/− compared with nNOS+/+ mice (*) in the occluded regions at 24 h following reperfusion in the longitudinal and circular layers. Neutrophil infiltration appeared to be distributed randomly in the mucosa and submucosa (c) compartments
SMA immunohistochemistry
SMA immunoreactivity is an excellent smooth muscle cell marker: it is highly selective for smooth muscle cells in adult animals and its expression is suppressed when smooth muscle is phenotypically changed when the muscle is damaged (Owens et al. 2004; Knowles et al. 2009). In absolute control and sham-operated animals, SMA-immunoreactive smooth muscle cells were well-defined and organized in regular bundles (Fig. 4). The majority of cell profiles in the muscle layers were SMA-immunoreactive. Following 3 h and 24 h reperfusion, significantly fewer of the cells in the external muscle layers of both nNOS−/− and nNOS+/+ mice had SMA immunoreactivity and immunoreactivity was commonly confined to a peri-nuclear ring (Fig. 4). To provide quantitative data, we counted the number of SMA-immunoreactive cells per millimetre length of intestine (Fig. 5). No significant differences were noted in the numbers of smooth muscle cells with SMA immunoreactivity between absolute control, sham and non-occluded regions. In the occluded regions, a significant reduction was found in the number of SMA-immunoreactive cells in nNOS−/− and nNOS+/+ mice compared with sham-operated animals following 3 h reperfusion (P<0.001; Fig. 5). At 24 h of reperfusion, the number of SMA-immunoreactive cells in nNOS−/− and nNOS+/+ mice was further reduced (P<0.001). Furthermore, the number of SMA-immunoreactive cells was significantly lower in nNOS−/− mice compared with nNOS+/+ mice at 3 and 24 h of reperfusion (P<0.001; Fig. 5).
α-Smooth muscle actin (SMA) immunoreactivity in nNOS knockout (nNOS −/−) and wild-type (nNOS +/+) mice following ischemia/reperfusion injury. a, d In nNOS+/+ and nNOS−/− sham-operated animals, SMA-immunoreactive cells are well defined and organized (LM longitudinal muscle, CM circular muscle). b, e Following 3 h reperfusion, fewer SMA immunoreactive cells can be detected. In the longitudinal muscle, many of the cells identified by DAPI nuclear staining have no SMA immunoreactivity. c, f SMA immunoreactivity is lost from many cells after 24 h reperfusion and cells in the longitudinal muscle from nNOS−/− animals have little cytoplasmic SMA (green SMA, red DAPI). Bars 20 μM
Number of α-smooth muscle actin (SMA)-immunoreactive (-IR) cells per millimetre length of intestine. No significant differences are present in the number of SMA-immunoreactive cells between absolute control, sham and non-occluded (non-occ) regions. Following 3 and 24 h reperfusion, a significant reduction occurs in the number of SMA-immunoreactive cells in both nNOS−/− and nNOS+/+ mice (P<0.001). Furthermore, the number of SMA-immunoreactive cells is significantly fewer in nNOS−/− compared with nNOS+/+ mice at both time points (*)
Immunoreactivity for nNOS and VIP
In the small intestine from normal mice, nNOS is co-localized with VIP in the terminals of enteric inhibitory neurons that innervate the circular muscle. In the nNOS−/− mice, nNOS could no longer be detected. However, the innervation of the circular muscle by VIP-immunoreactive nerve fibres was the same in the intestines from nNOS+/+ and nNOS−/− mice (Fig. 6), indicating that the knockout of nNOS did not detectably change the pattern of innervation of the muscle.
Vasoactive intestinal peptide (VIP) immunoreactivity in nNOS+/+ and nNOS−/− mice. The innervation of the circular muscle by VIP-immunoreactive nerve fibres was the same in the intestines from nNOS+/+ (a) and nNOS−/− (b), indicating the lack of effect of the knocking out of nNOS on the pattern of innervation of the muscle. Bar 20 μM
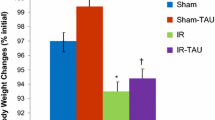
Contractions of the longitudinal muscle
The muscle of the small intestine from control mice exhibited regular rhythmic tension changes (Fig. 7). The contractions were of smaller amplitude in segments of intestine from sham-operated mice (Fig. 7) and were of even lower amplitude in segments from nNOS−/− and nNOS+/+ mice that were subjected to I/R. To quantify changes in basal contractile activity of the longitudinal muscle, we determined the motility index (frequency of contractions × average contraction amplitude) from occluded, non-occluded and sham-operated regions (Fig. 7). No significant differences were measured in the motility index in absolute control mice compared with sham-non-occluded regions (Fig. 7). Following 3 h of reperfusion, the motility index was significantly reduced in the occluded and non-occluded regions subjected to I/R compared with absolute control animals (P<0.001; Fig. 7). This reduction was even greater and the contractions were almost abolished in the occluded regions following 24 h reperfusion (P<0.001; Fig. 5). Moreover, a significant reduction was recorded in the sham-occluded regions when compared with absolute control samples (P<0.001; Fig. 7).
Examples of contractile activity and motility index in absolute control, sham, occluded and non-occluded regions of nNOS−/− and nNOS+/+ mice. a Typical tracings of longitudinal muscle contractions from the mouse distal ileum showing basal spontaneous activity. b Quantitative data of the changes in the motility index following I/R. Note the significant reduction in the motility index in the occluded and non-occluded regions of nNOS−/− and nNOS+/+ mice compared with absolute control animals following 3 h reperfusion (P<0.001). This reduction was greater in the occluded regions subjected to I/R after 24 h reperfusion (P<0.001). The sham-occluded regions were also significantly affected (P<0.001)
In small intestine from absolute control, occluded, non-occluded and sham-operated animals, EFS (2, 5, 10 Hz) induced frequency-dependent transient longitudinal muscle contractions (Fig. 8). These contractions to EFS were abolished by TTX (1 μM) indicating that they were of neuronal origin in all regions. For all of the frequencies tested, no significant differences were found in the amplitudes of contractions between absolute control and sham-operated mice. Moreover, no significant differences were observed in any of the groups when stimulated at 2 Hz (Fig. 8b). At 3 h of reperfusion, a significant reduction occurred in the amplitude of contraction of preparations from both nNOS−/− and nNOS+/+ mice when stimulated at 5 Hz compared with sham-operated mice (P<0.05). Following 24 h reperfusion, the amplitudes of contractions were significantly lower in tissue from nNOS−/− and nNOS+/+ mice when stimulated at 5 Hz and 20 Hz when compared with those of sham-operated mice (P<0.05). Additionally, the occluded regions from nNOS−/− mice were significantly less responsive compared with those from nNOS+/+ mice following 24 h reperfusion (P<0.05).
Responses to electrical field stimulation (EFS; 2, 5, 20 Hz) following I/R. a Typical tracings showing the contractions elicited in response to EFS at 5 Hz. b No significant differences are found in the amplitudes of contraction following 2 Hz stimulation. At 5 Hz (c) and 20 Hz (d), the amplitudes of contractions were significantly lower in the occluded regions of nNOS−/− and nNOS+/+ compared with those of sham-operated mice following 24 h reperfusion (P<0.05). Furthermore, the occluded regions from nNOS−/− mice were significantly less responsive compared with those of nNOS+/+ animals following 24 h reperfusion (*)
The muscarinic receptor agonist carbachol (0.1, 1, 10 μM) induced concentration-dependent sustained contractions in all samples. No significant differences were seen in any of the groups when 0.1 μM of carbachol was added (Fig. 9) or in the amplitude of contractions in response to carbachol (1 and 10 μM) between absolute control, non-occluded and sham-operated mice. In the occluded regions, the amplitude was significantly lower in tissue from nNOS−/− and nNOS+/+ mice following 3 and 24 h reperfusion when compared with sham-operated mice (P<0.05). In addition, the occluded regions from nNOS−/− mice were significantly less responsive compared with those of nNOS+/+ mice following 24 h reperfusion (P<0.05).
Responses to carbachol (0.1, 1, 10 μM) following I/R. a No significant differences are observed in the amplitudes of contraction following the addition of 0.1 μM carbachol in any of the groups. At 1 μM (c) and 10 μM (d), the amplitude of contractions are significantly lower in occluded regions from nNOS−/− and nNOS+/+ mice compared with sham-operated mice at 24 h following reperfusion (P<0.01). In addition, the occluded regions from nNOS−/− mice were significantly less responsive compared with those of nNOS+/+ mice following 24 h reperfusion (*)
Discussion
The present study has revealed that the deletion of nNOS results in markedly greater I/R-induced damage to the small intestine than occurs in normal animals, suggesting that NO produced by nNOS plays a protective role following intestinal I/R. nNOS−/− mice exhibit severe damage to the external muscle, increased neutrophil infiltration, fewer SMA-immunoreactive muscle cells, lowered contractile activity and reduced muscle responsiveness to nerve stimulation or a muscarinic agonist in comparison with nNOS+/+ mice.
Other animal experiments also indicate that NO has protective roles in the intestine, consistent with the present result with the knockout of nNOS. Inhibition of all NOS isoforms by using the broad spectrum NOS inhibitor, l-NAME, in drinking water causes ileitis (Miller et al. 1994) suggesting that the net effect of NO in the intestine is protective, even in animals that are not artificially challenged. However, the intestine is always under a low level of challenge; foreign material is always present in the lumen, large numbers of immune cells occur in the mucosa and inducible NOS is constitutively present (Hoffman et al. 1997; Furness et al. 1999; McCafferty et al. 1999). In animals challenged by gastrointestinal inflammation, the inhibition of NOS, with l-NNA or l-NAME, increases alcohol-induced gastric damage (Masuda et al. 1995) and exacerbates trinitrobenzenesulfonate-induced colitis in rats (Pfeiffer and Qiu 1995).
NO donors reduce the intestinal permeability increase that occurs after I/R (Payne and Kubes 1993). Consistent with this result, the injection of L-NAME prior to I/R increases dextran leakage across the intestinal mucosa, compared with I/R alone (Luo et al. 2001). These studies have not examined mucosal structure. However, our histological investigation indicates that greater mucosal damage occurs in nNOS−/− mice suggesting that the results of Payne and Kubes (1993) and Luo et al. (2001) can be explained by the influence of NO on the physical breakdown of the mucosal barrier. These findings suggest a role for the nNOS that has been reported to be expressed by mucosal epithelial cells in the intestine (Torihashi et al. 1996) in mucosal protection.
Results obtained in the intestine subjected to I/R by Taha et al. (2010), who have used a pharmacological block of NOS, are in apparent contrast to our data. Taha et al. (2010) reported that the reduction in contractions of the isolated rabbit jejunum, caused by ischemia for 1 h plus reperfusion for 2 h before the jejunum was removed, was less after the blocking of all NOS isoforms, whereas we observed an increased deficit with nNOS knockout. They gave L-NAME prior to applying the vascular clamp and during reperfusion. Contractions were elicited by transmural stimulation or KCl. This suggests that the blocking of all NOS isoforms (Taha et al. 2010) has a different outcome compared with merely inactivating nNOS (present study). The results of our study and that of Taha et al. (2010) support the hypothesis that nNOS is involved in normal physiological control in the intestine and that its role is protective, whereas iNOS is capable of producing large amounts of NO, which causes tissue damage (Kubes and McCafferty 2000; Kobayashi 2010). Consistent with this hypothesis, Beck et al. (2004) have found that the knockout of nNOS causes a more severe dextran-sodium-sulfate-induced colitis, whereas dextran-sodium-sulfate is less damaging in iNOS knockouts.
Cytoprotective roles of NO
Several mechanisms through which NO could have protective actions in the intestine are feasible, including inhibition of neutrophil extravasation, inhibition of vascular permeability increases, vasodilation increasing local blood flow and inhibition of cytokine production or action. Kubes et al. (1991) have reported that NOS inhibitors increase leukocyte adhesion to the vascular endothelium and enhance extravasation. Essentially similar results have been found by Kurose et al. (1993) who have used direct observation to view leukocyte adhesion and extravasation from mesenteric vessels in vivo. Moreover, NO and NO-releasing compounds inhibit neutrophil adhesion to endothelial cells (Grisham et al. 1998; Kosonen et al. 1999). During intestinal reperfusion, neutrophils rapidly infiltrate the external musculature and secrete molecules, including MPO and elastase that can damage the tissue (Massberg and Messmer 1998; Hierholzer et al. 1999). As we have confirmed in mice (Pontell et al. 2011), I/R injury to human tissue triggers neutrophil invasion of the external muscle and also activates macrophages (Türler et al. 2002). In the current study, we have found that the infiltration of neutrophils into the muscle layers of the region that is subjected to ischemia is greater in nNOS−/− mice compared with nNOS+/+ mice.
Evidence has also been presented that NO produced by 1nNOS suppresses nuclear factor kappa B (NF-қB) activation and subsequently reduces iNOS expression in cultured astrocytes (Togashi et al. 1997). In the intestine, the inhibition of nNOS with the selective inhibitor 7-nitroindazole increases the levels of NF-қB (Qu et al. 2001). NO might also have a cytoprotective role in the intestine during and immediately after ischemia by promoting vasodilation (Pique et al. 1989).
Ileus
After almost all abdominal surgery, a period of intestinal hypomotility referred to as post-operative ileus commonly occurs (Bauer and Boeckxstaens 2004; Lubbers et al. 2010). Ileus generally lasts 1–5 days but can persist for several weeks in some patients (Livingston and Passaro 1990; Lubbers et al. 2010). An inflammatory cascade is initiated when the intestine is handled, most notably the muscular layers of the intestine (Kalff et al. 1998a, 1999). This prominent inflammation is thought to initiate the hypomotility in the manipulated areas and can also lead to generalized stasis in the gastrointestinal tract (Lubbers et al. 2010). In the present study, we have observed a depression of motility in sham-operated animals and found neutrophils in the external muscle, although none are present in the control. Thus, we attribute the hypomotility in sham-operated animals to post-operative ileus. This indicates that, after I/R in the current study, both a post-operative ileus and an effect of I/R on motility occur. The muscle damage observed after I/R is not observed in sham-operated rats.
References
Bauer AJ, Boeckxstaens GE (2004) Mechanisms of postoperative ileus. Neurogastroenterol Motil 16:54–60
Beck PL, Xavier R, Wong J, Ezedi I, Mashimo H, Mizoguchi A, Mizoguchi E, Bhan AK, Podolsky DK (2004) Paradoxical roles of different nitric oxide synthase isoforms in colonic injury. Am J Physiol 286:G137–G147
Ferrer-Sueta G, Radi R (2009) Chemical biology of peroxynitrite: kinetics, diffusion, and radicals. ACS Chem Biol 4:161–177
Furness JB, Costa M (1979) Projections of intestinal neurons showing immunoreactivity for vasoactive intestinal polypeptide are consistent with these neurons being the enteric inhibitory neurons. Neurosci Lett 15:199–204
Furness JB, Kunze WAA, Clerc N (1999) Nutrient tasting and signaling mechanisms in the gut. II. The intestine as a sensory organ: neural, endocrine, and immune responses. Am J Physiol 277:G922–G928
Gabella G (1974) Special muscle cells and their innervation in the mammalian small intestine. Cell Tissue Res 153:63–77
Granger N, Korthuis RJ (1995) Physiologic mechanisms of postischemic tissue injury. Annu Rev Physiol 57:311–332
Grisham MB, Granger DN, Lefer DJ (1998) Modulation of leukocyte-endothelial interactions by reactive metabolites of oxygen and nitrogen: relevance to ischemic heart disease. Free Radic Biol Med 25:404–433
Hierholzer C, Kalff JC, Audolfsson G, Billiar TR, Tweardy DJ, Bauer AJ (1999) Molecular and functional contractile sequelae of rat intestinal ischemia/reperfusion injury. Transplantation 68:1244–1254
Hoffman RA, Zhang G, Nussler NC, Gleixner SL, Ford HR, Simmons RL, Watkins SC (1997) Constitutive expression of inducible nitric oxide synthase in the mouse ileal mucosa. Am J Physiol Gastrointest Liver Physiol 272:G383–G392
Huang PL, Dawson TM, Bredt DS, Snyder SH, Fishman MC (1993) Targeted disruption of the neuronal nitric oxide synthase gene. Cell 75:1273–1286
Kalff JC, Schraut WH, Simmons RL, Bauer AJ (1998a) Surgical manipulation of the gut elicits an intestinal muscularis inflammatory response resulting in postsurgical ileus. Ann Surg 228:652–663
Kalff JC, Schwarz NT, Walgenbach KJ, Schraut WH, Bauer AJ (1998b) Leukocytes of the intestinal muscularis: their phenotype and isolation. J Leukoc Biol 63:683–691
Kalff JC, Carlos TM, Schraut WH, Billiar TR, Simmons RL, Bauer AJ (1999) Surgically induced leukocytic infiltrates within the rat intestinal muscularis mediate postoperative ileus. Gastroenterology 117:378–387
Knowles CH, De Giorgio R, Kapur RP, Bruder E, Farrugia G, Geboes K, Gershon MD, Hutson J, Lindberg G, Martin JE, Meier-Ruge WA, Milla PJ, Smith VV, Vandervinden JM, Veress B, Wedel T (2009) Gastrointestinal neuromuscular pathology: guidelines for histological techniques and reporting on behalf of the Gastro 2009 International Working Group. Acta Neuropathol 118:271–301
Kobayashi Y (2010) The regulatory role of nitric oxide in proinflammatory cytokine expression during the induction and resolution of inflammation. J Leukoc Biol 88:1157–1162
Kosonen O, Kankaanranta H, Malo-Ranta U, Moilanen E (1999) Nitric oxide-releasing compounds inhibit neutrophil adhesion to endothelial cells. Eur J Pharmacol 382:111–117
Kubes P, McCafferty DM (2000) Nitric oxide and intestinal inflammation. Am J Med 109:150–158
Kubes P, Suzuki M, Granger DN (1991) Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci USA 88:4651–4655
Kurose I, Kubes P, Wolf R, Anderson DC, Paulson J, Miyasada M, Granger DN (1993) Inhibition of nitric oxide production. Mechanisms of vascular albumin leakage. Circ Res 73:164–171
Lipton P (1999) Ischemic cell death in brain neurons. Physiol Rev 79:1431–1568
Livingston EH, Passaro EP Jr (1990) Postoperative ileus. Dig Dis Sci 35:121–132
Love S (1999) Oxidative stress in brain ischemia. Brain Pathol 9:119–131
Lubbers T, Buurman W, Luyer M (2010) Controlling postoperative ileus by vagal activation. World J Gastroenterol 16:1683–1687
Luo CC, Chen HM, Chiu CH, Lin JN, Chen JC (2001) Effect of NG-nitro-L-arginine methyl ester on intestinal permeability following intestinal ischemia-reperfusion injury in a rat model. Biol Neonate 80:60–63
Mallick IH, Yang W, Winslet MC, Seifalian AM (2004) Ischemia—reperfusion injury of the intestine and protective strategies against injury. Dig Dis Sci 49:1359–1377
Massberg S, Messmer K (1998) The nature of ischemia/reperfusion injury. Transplant Proc 30:4217–4223
Masuda E, Kawano S, Nagano K, Tsuji S, Takei Y, Tsujii M, Oshita M, Michida T, Kobayashi I, Nakama A, Fusamoto H, Kamada T (1995) Endogenous nitric oxide modulates ethanol-induced gastric mucosal injury in rats. Gastroenterology 108:58–64
McCafferty DM, Miampamba M, Sihota E, Sharkey KA, Kubes P (1999) Role of inducible nitric oxide synthase in trinitrobenzene sulphonic acid induced colitis in mice. Gut 45:864–873
Miller MJS, Munshi UK, Sadowska Krowicka H, Kakkis JL, Zhang XJ, Eloby-Childress S, Clark DA (1994) Inhibition of calcium-dependent nitric oxide synthase causes ileitis and leukocytosis in guinea pigs. Dig Dis Sci 39:1185–1192
Moro MA, Cárdenas A, Hurtado O, Leza JC, Lizasoain I (2004) Role of nitric oxide after brain ischaemia. Cell Calcium 36:265–275
Owens GK, Kumar MS, Wamhoff BR (2004) Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev 84:767–801
Payne D, Kubes P (1993) Nitric oxide donors reduce the rise in reperfusion-induced intestinal mucosal permeability. Am J Physiol Gastrointest Liver Physiol 265:G189–G195
Pfeiffer CJ, Qiu BS (1995) Effects of chronic nitric oxide synthase inhibition on TNB-induced colitis in rats. J Pharm Pharmacol 47:827–832
Pique JM, Whittle BJR, Esplugues JV (1989) The vasodilator role of endogenous nitric oxide in the rat gastric microcirculation. Eur J Pharmacol 174:293–296
Pontell L, Sharma P, Rivera LR, Thacker M, Tan YH, Brock JA, Furness JB (2011) Damaging effects of ischemia/reperfusion on intestinal muscle. Cell Tissue Res 343:411–419
Qu X-W, Wang H, De Plaen IG, Rozenfeld RA, Hsueh W (2001) Neuronal nitric oxide synthase (NOS) regulates the expression of inducible NOS in rat small intestine via modulation of nuclear factor kappa B. FASEB J 15:439–446
Rivera LR, Thacker M, Castelucci P, Bron R, Furness JB (2009) The reactions of specific neuron types to intestinal ischemia in the guinea pig enteric nervous system. Acta Neuropathol 118:261–270
Rivera LR, Poole DP, Thacker M, Furness JB (2011a) The involvement of nitric oxide synthase neurons in enteric neuropathies. Neurogastroenterol Motil 23:980–988
Rivera LR, Thacker M, Pontell L, Cho H-J, Furness JB (2011b) Deleterious effects of intestinal ischemia/reperfusion injury in the mouse enteric nervous system are associated with protein nitrosylation. Cell Tissue Res 344:111–123
Taha MO, Miranda-Ferreira R, Fagundes AL, Fagundes DJ, Simões RS, Santos JM, Souza PDF, Júnior ISO, Marchini A, Gomes IT, Monteiro HP, Mendonça LO, Caricati-Neto A (2010) Effects of L-nitro-arginine methyl ester, an inhibitor of nitric oxide biosynthesis, on intestinal ischemia/reperfusion injury in rabbits. Transplant Proc 42:457–460
Togashi H, Sasaki M, Frohman E, Taira E, Ratan RR, Dawson TM, Dawson VL (1997) Neuronal (type I) nitric oxide synthase regulates nuclear factor κB activity and immunologic (type II) nitric oxide synthase expression. Proc Natl Acad Sci USA 94:2676–2680
Torihashi S, Horowitz B, Pollock JS, Ward SM, Xue C, Kobayashi S, Sanders KM (1996) Expression of nitric oxide synthase in mucosal cells of the canine colon. Histochem Cell Biol 105:33–41
Türler A, Kalff JC, Heeckt P, Abu-Elmagd KM, Schraut WH, Bond GJ, Moore BA, Brünagel G, Bauer AJ (2002) Molecular and functional observations on the donor intestinal muscularis during human small bowel transplantation. Gastroenterology 122:1886–1897
Woodruff TM, Thundyil J, Tang S-C, Sobey CG, Taylor SM, Arumugam TV (2011) Pathophysiology, treatment, and animal and cellular models of human ischemic stroke. Mol Neurodegener 6:1–19
Acknowledgments
We thank Associate Professor James Brock and Ms. Dorota Ferens for their helpful advice on the isometric tension recording experiments, Dr. Trung Nguyen for statistical advice and Mr. Gene Venables for his assistance in surgery and genotyping.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by a grant from the National Health and Medical Research Council of Australia (grant 1006035).
Rights and permissions
About this article
Cite this article
Rivera, L.R., Pontell, L., Cho, HJ. et al. Knock out of neuronal nitric oxide synthase exacerbates intestinal ischemia/reperfusion injury in mice. Cell Tissue Res 349, 565–576 (2012). https://doi.org/10.1007/s00441-012-1451-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-012-1451-3