Abstract
Purpose
The aim of this study was to compare the risk of chemotherapy-induced nausea and vomiting (CINV) events for various 5-HT3 RAs in patients who received moderately (MEC) or highly emetogenic chemotherapy (HEC) by evaluating hospital or emergency department (ED) admissions.
Methods
PharMetrics claims database was used to identify patients diagnosed with breast cancer (BC) who were initiated on cyclophosphamide-based adjuvant chemotherapy or with lung cancer (LC) initiated on carboplatin-based or cisplatin-based chemotherapy between 2005 and 2008. Patients were stratified in two groups: those initiated and maintained on palonosetron versus those treated with any other 5-HT3 RA regimens in the 6-month post first chemotherapy. Risk for CINV events, identified by ICD-9-CM for nausea, vomiting, and/or dehydration, were estimated using logistic regressions, controlling for age, gender, comorbidity, and total chemotherapy doses or days.
Results
Of the 4,868 cyclophosphamide-treated BC, 5,414 carboplatin-treated LC, and 1,692 cisplatin-treated LC identified, there were 1,864 BC (38.5%), 1,806 carboplatin-treated LC (33.4%), and 390 cisplatin-treated LC (23.0%) in the palonosetron-only group. Palonosetron-only group had significantly lower probability of CINV events associated with ED/hospital admissions in all three cohorts (3.5% vs. 6.3% in BC, 9.5% vs. 13.8% in carboplatin-treated LC, and 16.4% vs. 22.6% in cisplatin-treated LC, all at p < 0.05). Logistic regressions found palonosetron-only group had significantly lower risk of CINV events (odds ratios = 0.550, 0.653, and 0.689 in BC, carboplatin-treated LC and cisplatin-treated LC, respectively, p < 0.05).
Conclusion
Patients with lung or breast cancer receiving MEC or HEC had significantly lower risk of CINV events associated with hospital/ED admissions if initiated and maintained on palonosetron relative to patients receiving 5-HT3 RA regimens.
Similar content being viewed by others
Introduction
Antiemetics including the 5-hydroxytryptamine receptor antagonists (5-HT3 RAs) have been used predominantly to improve the prophylaxis of chemotherapy-induced nausea and vomiting (CINV) in patients placed on moderately (MEC) or highly emetogenic (HEC) chemotherapy [1, 2]. Palonosetron (Aloxi®), a newer 5-HT3 RA, was approved in the USA in 2003 for the prevention of acute and delayed CINV in patients with cancer receiving MEC or HEC [3]. Palonosetron is a potent and highly selective 5-HT3 RA with strong binding affinity to the receptor and a longer plasma elimination half-life of about 40 h as compared to the older 5-HT3 RAs [3]. Palonosetron also exhibits allosteric interactions, triggers receptor internalization, differentially inhibits “crosstalk” between NK-1 receptors and 5-HT3 signaling pathways, and exhibits prolonged inhibition of receptor function [4, 5]. Palonosetron is the first and the only agent in the class that is approved for preventing both delayed and acute emesis induced in patients receiving MEC [6, 7].
In four phase III trials, palonosetron was reported to have improved efficacy relative to the older 5-HT3 RAs in the prevention of nausea and vomiting associated with initial and repeat courses of MEC or HEC [2, 8–10]. Gralla and colleagues evaluated patients randomized to receive single intravenous (i.v.) palonosetron doses of 0.25 or 0.75 mg, or ondansetron (32 mg), before initiating MEC. Palonosetron at 0.25 mg was significantly superior to ondansetron in the prevention of acute and delayed CINV events. Complete response rates were significantly higher for palonosetron-treated patients during the acute phase (81.0% vs. 68.6%), the delayed phase (74.1% vs. 55.1%), and the overall phase (69.3% vs. 50.3%) [8]. In the second MEC trial, Eisenberg et al. reported on a multicenter, double-blind, phase III study in patients who were randomized to receive i.v. palonosetron doses of 0.25 or 0.75 mg, or dolasetron (100 mg) before initiating MEC [9]. Complete response rates were significantly higher for palonosetron during the acute phase (63.0% and 52.9% for 0.25 mg palonosetron and dolasetron, respectively), the delayed phase (54.0% and 38.7%, respectively), and the overall phase (46.0% and 34.0%, respectively).
The Aapro et al. study [2] was one of the two phase III trials that studied the efficacy and safety of palonosetron in preventing CINV following HEC. Single-dose palonosetron was found as efficacious as ondansetron in preventing acute CINV. Moreover, palonosetron was significantly more efficacious than ondansetron during the delayed (42.0% vs. 28.6%) and the overall phases (40.7% vs. 25.2%) when patients were pre-treated with dexamethasone [2]. In a second phase III HEC trial carried out in Japan, patients with cancer and treated with HEC were randomly assigned to either single-dose palonosetron (0.75 mg) or granisetron (40 mcg/kg) given 30 min before HEC on day 1. Reported results indicated that when palonosetron was administered with dexamethasone before HEC, it exerted efficacy against CINV which was non-inferior to that of granisetron in the acute phase and better than that of granisetron in the delayed phase, with a comparable safety profile for the two treatments [10].
While the efficacy of palonosetron in preventing CINV events has been well documented in clinical trials, its effectiveness in the real-world clinical practice has not been systematically reported. Hence, the present study was performed with a large claims database to investigate the comparative effectiveness of palonosetron versus other 5-HT3 RAs as prophylaxis for resource-intensive CINV events associated with hospital and/or emergency department (ED) admissions in patients with breast or lung cancer receiving MEC or HEC. The secondary objective was to compare the effectiveness results reported in this study with the efficacy data previously reported in phase III clinical trials.
Study patients and methods
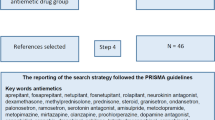
The study population was selected from PharMetrics database, which compiles integrated managed care pharmacy and medical claims of over 2 billion inpatient and outpatient transactions from 60 million members nationwide. The study included one cohort of patients diagnosed with breast cancer who received adjuvant chemotherapy with cyclophosphamide within 4 months after surgery. The other two cohorts included patients diagnosed with lung cancer who were initiated on either carboplatin or cisplatin-based chemotherapy within the study time frame (January 1, 2005 and June 30, 2008). Figures 1 and 2 depict the selection process for patients with breast cancer and lung cancer. Based on doses used and/or the published literature, the breast cancer and the carboplatin-treated lung cancer cohorts were considered MEC-treated. The cisplatin-treated lung cancer cohort was considered as HEC-treated.
The study index date was defined as the date of breast cancer diagnosis for the breast cancer cohort or the first date of chemotherapy with carboplatin/cisplatin for the lung cancer cohorts. The index chemotherapy was the first chemotherapy treatment cycle, while the index chemotherapy date was marked as the first date of the index chemotherapy.
Patients with breast cancer were identified using the International Classification of Diseases-Clinical Modification, 9th Revision (ICD-9-CM) codes (174.xx), while those with lung cancer were identified by ICD-9-CM codes of 162.xx. National Drug Codes and Healthcare Common Procedure Coding System (HCPCS) codes were used to identify chemotherapeutic agents. Selected patients were ≥18 years of age with records of claims for ≥6 months prior to study index date. Patients who received cyclophosphamide, carboplatin, or cisplatin within 6 months prior to index chemotherapy were excluded. Additional inclusion criteria consisted of no prior history of vomiting, nausea, or dehydration identified by ICD-9-CM codes for 6 months prior to the index chemotherapy date and that patients must have had ≥6-month follow-up period after the index chemotherapy date. Study duration was defined as 6 months from the index chemotherapy.
Investigated antiemetics included dolasetron, granisetron and ondansetron, palonosetron, aprepitant, and dexamethasone. Patients were stratified into two groups, with one consisting of patients initiated and maintained on palonosetron as the only 5-HT3 RA antiemetic (palonosetron-only group). The other group included patients who were initiated on one of the older 5-HT3 RAs and maintained on the same agent or alternated throughout the study duration between the older 5-HT3 RAs and palonosetron, either as single agents or in combinations. The use of aprepitant and dexamethasone was accounted for in both study groups.
Comorbidities for the 6-month baseline period prior to the study index date were calculated using the Charlson Comorbidity Index (CCI) [11, 12]. CINV events associated with hospital/ED admissions were extracted using claims with ICD-9-CM codes for nausea, vomiting, and/or dehydration (787.0, 787.01, 787.02, 787.03, 276.5, 276.50, 276.51, and 276.52). Cyclophosphamide doses per square meter per cycle, or total cisplatin/carboplatin treatment days for the study duration, were calculated. Age and gender of patients were also considered.
Statistical analyses
Means and standard deviations were calculated for continuous variables with t tests performed to compare the palonosetron-only to the other 5-HT3 RA regimen-treated groups. Sample sizes and frequency distributions were reported for categorical variables with chi-square results. Separate multivariate logistic regressions were performed for the three cancer cohorts to compare the risk of experiencing hospital/ED-associated CINV events (dependent variable) between the two study groups, controlling for differences in age, CCI score, gender (lung cancer), cyclophosphamide dose per square meter per cycle (breast cancer), and cisplatin/carboplatin treatment days (lung cancer).
To compare the clinical effectiveness of palonosetron estimated from the current study and efficacy estimated from previous clinical trials, the relative risks, absolute risk reductions, and relative risk reductions of CINV events were computed. Moreover, the adjusted relative risks and relative risk reductions were computed based on odds ratios (ORs) from multiple logistic regression models and baseline incidences of outcome estimated in the current study [13]. All statistical analyses were carried out using SAS 9.0 statistical software (SAS Institute, Inc, Cary, NC, USA).
Results
Characteristics of the study cohorts
A total of 4,868 female patients with breast cancer were identified. For the study duration, 43.1% were treated with 5-HT3 RA antiemetic prophylaxis only, 25.0% were treated with 5-HT3 RAs in combination with dexamethasone, 11.8% were treated with 5-HT3 RAs in combination with aprepitant, and 20.1% were treated with combination of a 5-HT3 RA, dexamethasone, and aprepitant. The average age (mean ± SD) of the breast cancer cohort was 53.2 ± 9.8 years. The average cyclophosphamide dose per square meter per chemotherapy cycle was 414.1 ± 343.3 mg, and the average CCI score was 0.5 ± 1.0. The average number of claims of all antiemetics was 9.8 ± 5.4 and was 7.7 ± 4.1 when only the 5-HT3 RAs were counted. In the 6-month post-index date study duration, most patients with breast cancer received either four (71.9%) or six chemotherapy cycles (13.0%).
Among the breast cancer cohort, 1,864 (38.3%) belonged to the palonosetron-only group. As compared to the other 5-HT3 RA group, the palonosetron-only group was significantly older (53.7 ± 10.0 years vs. 53.0 ± 9.7 years), received a higher average cyclophosphamide dose (milligrams per square meter per cycle, 430.8 ± 335.5 vs. 403.7 ± 347.6), with fewer antiemetic claims (8.3 ± 4.6 vs. 10.8 ± 5.6) or 5-HT3 RA-only claims (6.2 ± 3.4 vs. 8.5 ± 4.4); all differences were statistically significant (p < 0.05; Table 1). The two comparison groups had comparable CCI score (0.5 ± 1.0 vs. 0.5 ± 1.1).
The carboplatin-treated lung cancer cohort consisted of 5,414 patients, with 66.6% treated with 5-HT3 RA antiemetic prophylaxis only, 29.0% treated with 5-HT3 RAs in combination with dexamethasone, 1.6% treated with 5-HT3 RAs combined with aprepitant, and 2.8% treated with a combined regimen of 5-HT3 RAs, dexamethasone and aprepitant. This cohort had an average age of 64.6 ± 10.2 years, with 2,518 (46.5%) females, and an average CCI score of 6.8 ± 3.2. Average days on carboplatin treatment were 6.2 ± 3.7. Average number of claims for all antiemetics was 10.6 ± 6.7, with an average of 9.6 ± 6.0 when only the 5-HT3 RAs were considered.
One third (33.4%) of the patients with lung cancer treated with carboplatin was in the palonosetron-only group. The palonosetron-only group was significantly older (65.0 ± 10.3 years vs. 64.4 ± 10.1 years), had significantly fewer antiemetic claims (8.5 ± 5.4 vs. 11.7 ± 7.1) or 5-HT3 RA claims (7.7 ± 4.9 vs. 10.5 ± 6.3), and lower CCI score (6.7 ± 3.3 vs. 6.9 ± 3.2); all p < 0.05; (Table 1) versus the other 5-HT3 RA group.
There were 1,692 patients identified with lung cancer on cisplatin therapy. Among these, 46.8% were treated with 5-HT3 RA antiemetic prophylaxis only, 20.1% treated with 5-HT3 RAs in combination with dexamethasone, 13.6% treated with 5-HT3 RAs in combination with aprepitant, and 19.3% treated with a combination regimen of 5-HT3 RAs, dexamethasone and aprepitant. This cohort had an average age of 60.2 ± 9.6 years, 682 (40.3%) females, and an average CCI score of 6.5 ± 3.2. The average cisplatin treatment days throughout the study were 5.6 ± 4.2. The average numbers of claims of all antiemetics were 13.3 ± 7.8 and 11.1 ± 6.6 when only the 5-HT3 RAs were counted.
A total of 390 (23.0%) patients in the cisplatin-treated lung cancer cohort belonged to the palonosetron-only group. The palonosetron-only group was significantly older than the other 5-HT3 RA regimen group (61.3 ± 9.8 years vs. 59.9 ± 9.5 years), incurred significantly fewer antiemetic claims (8.5 ± 5.6 vs. 14.7 ± 7.8) or 5-HT3 RA claims (6.4 ± 4.4 vs. 12.4 ± 6.5), with fewer cisplatin treatment days (4.9 ± 3.2 vs. 5.7 ± 4.4). There were significantly fewer females in the palonosetron-only group (33.3% vs. 42.4%; all p < 0.05, Table 1).
Antiemetic combination use by comparison groups
In all three cohorts, higher proportions of patients in the palonosetron-only group were treated without adding aprepitant, dexamethasone, or both. In the breast cancer cohort, 46.1% of the patients in the palonosetron-only group were treated with palonosetron only, as opposed to 41.3% who used any other 5-HT3 RA agent in the other 5-HT3 RA regimen group (p < 0.0001). Similarly, in the carboplatin-treated lung cancer cohort, 72.9% of the patients in the palonosetron-only group were treated with palonosetron only, as opposed to 63.4% in the other group (p < 0.0001). Among the cisplatin-treated lung cancer cohort, 51.0% in the palonosetron-only treated group used palonosetron as the sole antiemetic, as opposed to 45.6% in the other group (p = 0.1170, Table 2).
Unadjusted risk for CINV
In the 6-month study follow-up period, 3.5% of the patients with breast cancer in the palonosetron-only group experienced ≥1 hospital/ED-associated CINV events as opposed to 6.3% in the other group, p < 0.0001. Among the carboplatin-treated lung cancer cohort, the proportions were 9.5% and 13.8% for the two groups, respectively, p < 0.0001. A similar pattern was observed in the cisplatin-treated lung cancer cohort, with proportions of 16.4% and 22.6% (p = 0.0089).
Adjusted risk for CINV
In the breast cancer cohort, multivariate logistic regression analysis showed that the palonosetron-only group experienced a significantly lower risk (45%) for a hospital/ED-associated CINV event as compared to the other 5-HT3 RA group (OR, 0.550; 95% CI: 0.412–0.733; p < 0.0001; Table 3). Older age significantly reduced risk of outcome (OR, 0.984, 95% CI: 0.971–0.997, p = 0.0196) while higher CCI score significantly increased the risk (OR, 1.271; 95% CI: 1.168–1.384, p < 0.001).
In the carboplatin-treated lung cancer cohort, the palonosetron-only group showed a significantly lower risk (35%) of CINV events (OR, 0.653; 95% CI: 0.543–0.785; p < 0.0001). Higher CCI score significantly increased the risk of CINV (OR, 1.028; 95% CI, 1.002–1.054, p = 0.0361), whereas more carboplatin treatment days reduced the risk (OR, 0.952; 95% CI, 0.929–0.976, p = 0.0001). Similar findings were observed in the cisplatin-treated lung cancer cohort, with the palonosetron-only group experiencing significantly lower risk for a CINV event (OR, 0.689, 95% CI: 0.510–0.931; p = 0.0152). Higher CCI scores significantly increased the risk of CINV (OR, 1.041, 95% CI: 1.003–1.080; p = 0.0319; Table 3).
Results from the current study and the four published phase III clinical trials [2, 8–10] comparing palonosetron and older 5-HT3 RAs are summarized in Table 4. Based on the complete response rate of CINV in the overall study period reported in the clinical trials, the computed relative risks of CINV events for the palonosetron group versus the other comparison groups ranged from 0.618 to 0.884. Also, the computed relative risk reductions ranged between 11.6% and 38.2% for the palonosetron group versus the older 5-HT3 RAs. The relative risk reductions ranged from 25.9% to 43.4% in the current study.
Discussion
To our knowledge, this study is the first to investigate the comparative effectiveness of palonosetron-only as the 5-HT3 RA treatment versus other 5-HT3 RA treatment regimens using claims from a large database compiled from real-world clinical practice. Results indicated that among patients with breast or lung cancer on HEC or MEC, those initiated and maintained with palonosetron throughout the chemotherapy treatment cycles experienced a significantly reduced risk of hospital/ED-associated CINV events, as compared to patients who received other 5-HT3 RA-based regimens.
Results of this retrospective cohort study corroborate data obtained from earlier published clinical trials. The clinical trials and real-world community setting practice data indicate that prophylaxis and treatment with palonosetron was associated with a significant risk reduction for more severe CINV events. Although this study focused only on CINV events associated with admission to emergency departments or hospitals as opposed to all CINV events reported in clinical trials, the relative risk reductions reported here are comparable to those reported in these trials. More specifically, the relative risk reductions computed from the four trials ranged between 11.6% and 38.2% for the palonosetron group as compared to the older 5-HT3 RAs. This study focused on the more severe CINV events, while the clinical trials conducted with palonosetron reported on all CINV events. In spite of the difference in severity of CINV between this study and the earlier conducted clinical trials, our calculated relative risk reductions ranging between 25.9% and 43.4% were in line with the trials’ data. Additionally, a recently published study using medical record review reported that patients with gynecological cancer treated with cisplatin when prophylaxed with palonosetron experienced a lower risk of CINV-related hospital readmission versus patients prophylaxed with ondansetron [14].
Depending on the chemotherapy regimens, cyclophosphamide is given in a dose of 300–600 mg/m2 as adjuvant therapy to patient with breast cancer [15]. The average dose of cyclophosphamide used in the breast cancer cohort was at the lower end of the dosing range, which might imply that our study cohort might have a less severe clinical status than patients with breast cancer receiving higher doses of cyclophosphamide. As such, one might anticipate that the impact of palonosetron on CINV may be more pronounced if a patient cohort with more intense chemotherapy regimens was studied. There were additional noteworthy clinical differences between the two comparison groups. In the breast cancer cohort, patients on palonosetron-only received, on average, 27 mg/m2 (or 7%) higher cyclophosphamide dose per treatment cycle than the dose received by patients treated with the other 5-HT3 RA regimens. One of the plausible explanations of this finding maybe that patients who received palonosetron-only were better able to tolerate higher cyclophosphamide doses. This finding is relevant to the extent that high and moderate-dose intensity regimens were reported to result in significantly better disease-free survival and overall survival than the low-dose intensity regimens [16]. Similarly, the palonosetron-only group of the lung cancer cohorts needed fewer total CT days (cisplatin-treated lung cancer, 4.9 days vs. 5.7 days, p < 0.0001; carboplatin-treated lung cancer, 6.1 days vs. 6.2 days, p > 0.05) to complete their chemotherapy regimens. One of the plausible explanations, based on the study findings, is that patients who received the palonosetron-only regimen may have been better able to complete their chemotherapy treatment regimen within fewer days, in light of their CINV experience. The results of the logistic regressions support our contention. Patients with more CT days showed a lower risk of CINV, indicating that spreading CT over more days, and thus potentially lowering the dose given per day, might have been a strategy used to reduce the burden of CINV. Further comparative studies are required to investigate whether the differences seen between the two study groups in chemotherapy doses/days may in fact impact patients’ clinical status or result in some economic efficiency.
The proportion of patients who used a 5-HT3 RA alone without adding dexamethasone and/or aprepitant was higher in the palonosetron-only group. It is important to note that the pattern of antiemetic utilization observed in this analysis did not conform to the recommendations of the major CINV guidelines. The ASCO, MASCC-ESMO, and NCCN guidelines all recommend utilizing doublet therapy (dexamethasone and a 5-HT3 RA) for MEC and a triplet regimen (dexamethasone, a 5-HT3 receptor antagonist and an NK1 RA) for HEC as well as anthracycline–cyclophosphamide chemotherapy. In this analysis, single-agent 5-HT3 RA therapy was received by 43% of breast cancer patients, 67% of carboplatin-treated patients and 47% of cisplatin-treated patients. Furthermore, only 19% of cisplatin-treated lung cancer patients received triple therapy. These findings suggest that undertreatment with antiemetics was widespread during this period and the number of visits to the ED could be improved with a higher percentage of patients adhering to the current CINV prevention guidelines.
Although a triplet regimen of dexamethasone, palonosetron, and aprepitant has been shown to be an effective regimen for emesis prevention [17–19], whether palonosetron would similarly improve upon the results relative to other 5-HT3 RA regimens when evaluated in a population of patients who all received the recommended standard triplet antiemetic therapy remains an important question. The patient numbers from the current study were insufficient to carry out this type of analyses. However, a recent retrospective claims data analysis in over 4,000 patients all receiving a triplet regimen suggests that a difference persists even when guideline recommended regimens are given [20]. The triplet regimen that included palonosetron was associated with a lower risk for an uncontrolled CINV event than the triplet regimen that included an older 5-HT3 RA. Further prospective studies are warranted to further clarify an answer to this question [20].
In this study, we did not differentiate the individual first generation 5-HT3 RAs used, in part, to simplify the study design, and also based on an earlier report of no significant difference between the antiemetic efficacy of dolasetron, granisetron, or ondansetron in controlling CINV in patients on platinum-based chemotherapy regimens [21].
Finally, our ability to identify CINV depended on the availability of unique identifiers such as ICD-9-CM or CPT codes. As such, this study focused on CINV events resulting in ED or hospitalization episodes needed to manage these events without being able to address the significant negative impact of CINV events on patients’ health-related quality of life.
Limitations
The calculations of the actual doses used in the various chemotherapy regimens depended on the level of details provided by HCPCS codes. There were 11 unique HCPCS codes to identify cyclophosphamide. In contrast, there were only one or two HCPCS codes for cisplatin or carboplatin, respectively. The lack of HCPCS codes did not allow the calculation of the actual doses for carboplatin/cisplatin consumed, or the further delineation of the relationship between chemotherapy dose and 5-HT3 RA utilization patterns in the two cohorts of patients with lung cancer. Moreover, this study had the inherent limitations associated with retrospective analyses using claims database, such as the potential for selection bias. While CCI and multiple regressions were employed to adjust for the differences between comparison groups, it is not possible to ascertain whether the adjustment was sufficient to account for all the selection bias. Additionally, other factors that would be relevant to CINV outcomes, such as staging of the cancer, race, alcohol consumption, and smoking history were not available. The study analysis was based on an intent-to-treat principle, thereby not allowing for the estimation of chemotherapy or antiemetic medication discontinuation rates, or for dose adjustment, or medication adherence. Finally, the database used in this study was employer-based, thus potentially limiting the generalizability of the study findings.
Conclusions
The results from this real-world claims database corroborate clinical trial findings. This study showed that initiating and maintaining patients on a palonosetron-only 5-HT3 RA-based regimen reduced the risk of hospital/ED-associated CINV events in female breast cancer undergoing MEC adjuvant therapy post-surgical interventions. Similar results were also demonstrated in lung cancer patients treated with either MEC or HEC. Further studies are warranted on the overall comparative effectiveness of the individual antiemetics and their combined use on CINV outcomes and on patients’ health-related quality of life.
References
Mertens WC, Higby DJ, Brown D, Parisi R, Fitzgerald J, Benjamin EM, Lindenauer PK (2003) Improving the care of patients with regard to chemotherapy-induced nausea and emesis: the effect of feedback to clinicians on adherence to antiemetic prescribing guidelines. J Clin Oncol 21:1373–1378. doi:10.1200/JCO.2003.08.118
Aapro MS, Grunberg SM, Manikhas GM, Olivares G, Suarez T, Tjulandin SA, Bertoli LF, Yunus F, Morrica B, Lordick F, Macciocchi A (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol 17:1441–1449. doi:10.1093/annonc/mdl137
Oo TH, Hesketh PJ (2005) Drug insight: new antiemetics in the management of chemotherapy-induced nausea and vomiting. Nat Clin Pract Oncol 2:196–201. doi:10.1038/ncponc0132
Li Y, Wu X, Rojas C (2009) Palonosetron uniquely inhibits substance P-mediated neuronal responses in rat nodose ganglia. Annual American Society of Hematology Meeting, New Orleans
Rojas C, Thomas AG, Alt J, Stathis M, Zhang J, Rubenstein EB, Sebastiani S, Cantoreggi S, Slusher BS (2010) Palonosetron triggers 5-HT(3) receptor internalization and causes prolonged inhibition of receptor function. Eur J Pharmacol 626:193–199. doi:10.1016/j.ejphar.2009.10.002
Siddiqui MA, Scott LJ (2004) Palonosetron. Drugs 64:1125–1132. doi:10.2165/00003495-200464100-00006
Yang LP, Scott LJ (2009) Palonosetron: in the prevention of nausea and vomiting. Drugs 69:2257–2278. doi:10.2165/11200980-000000000-00000
Gralla R, Lichinitser M, Van Der Vegt S, Sleeboom H, Mezger J, Peschel C, Tonini G, Labianca R, Macciocchi A, Aapro M (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol 14:1570–1577. doi:10.1093/annonc/mdg417
Eisenberg P, Figueroa-Vadillo J, Zamora R, Charu V, Hajdenberg J, Cartmell A, Macciocchi A, Grunberg S (2003) Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist: results of a phase III, single-dose trial versus dolasetron. Cancer 98:2473–2482. doi:10.1002/cncr.11817
Saito M, Aogi K, Sekine I, Yoshizawa H, Yanagita Y, Sakai H, Inoue K, Kitagawa C, Ogura T, Mitsuhashi S (2009) Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. Lancet Oncol 10:115–124. doi:10.1016/S1470-2045(08)70313-9
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40:373–383
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
Zhang J, Yu KF (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691. doi:10.1001/jama.280.19.1690
Yeh YC, McDonnell A, Klinger EV, Fowler B, Matta L, Voit D, Reddy P (2011) Comparison of healthcare resource use between patients receiving ondansetron or palonosetron as prophylaxis for chemotherapy-induced nausea and vomiting. J Oncol Pharm Pract. doi:10.1177/1078155210366491
Perez E, Muss HB (2005) Optimizing adjuvant chemotherapy in early-stage breast cancer. Oncology 19:1759–1767
Bonadonna G, Moliterni A, Zambetti M, Daidone MG, Pilotti S, Gianni L, Valagussa P (2005) 30 years’ follow up of randomised studies of adjuvant CMF in operable breast cancer: cohort study. BMJ 330:217. doi:10.1136/bmj.38314.622095.8F
Grote T, Hajdenberg J, Cartmell A, Ferguson S, Ginkel A, Charu V (2006) Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol 4:403–408
Grunberg SM, Dugan M, Muss H, Wood M, Burdette-Radoux S, Weisberg T, Siebel M (2009) Effectiveness of a single-day three-drug regimen of dexamethasone, palonosetron, and aprepitant for the prevention of acute and delayed nausea and vomiting caused by moderately emetogenic chemotherapy. Support Care Canc 17:589–594
Herrington JD, Jaskiewicz AD, Song J (2008) Randomized, placebo-controlled, pilot study evaluating aprepitant single dose plus palonosetron and dexamethasone for the prevention of acute and delayed chemotherapy-induced nausea and vomiting. Cancer 112(9):2080–2087
Schwartzberg L, Jackson J, Jain G, Balu S, Buchner D. Risk of uncontrolled chemotherapy induced nausea and vomiting (CINV) with highly emetogenic chemotherapy and a triple combination anti-emetic prophylaxis regimen. Abtract accepted at 2011 Hematology/Oncology Pharmacists Association Annual Meeting; March 23–26, Salt Lake City, Utah
Hamadani M, Chaudhary L, Awan FT, Khan JK, Kojouri K, Ozer H, Tfayli A (2007) Management of platinum-based chemotherapy-induced acute nausea and vomiting: is there a superior serotonin receptor antagonist? J Oncol Pharm Pract 13:69–75. doi:10.1177/1078155207078137
Acknowledgments
This study was funded by Eisai, Inc.
Conflict of interest
H. T. Hatoum is a paid consultant to Eisai, Inc., the marketer of palonosetron in the USA and the sponsor of the study. S. Lin is a consultant to Hind T. Hatoum & Company. Both Deborah Buchner and David Cox are employees of Eisai, Inc. The authors had full control of all the primary data and findings. All authors agree to allow the journal to review the data if requested. Results are presented without any oversight or interference from the sponsor of the work.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Hatoum, H.T., Lin, SJ., Buchner, D. et al. Comparative clinical effectiveness of various 5-HT3 RA antiemetic regimens on chemotherapy-induced nausea and vomiting associated with hospital and emergency department visits in real world practice. Support Care Cancer 20, 941–949 (2012). https://doi.org/10.1007/s00520-011-1165-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-011-1165-1