Abstract
Purpose
The purpose of this study was to compare the efficacy of proton pump inhibitor (PPI) with H2 receptor antagonist (H2RA) in treatment of upper abdominal symptoms.
Methods
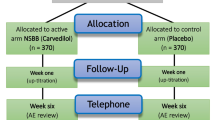
This was a multi-center, open study conducted at 102 hospitals in Japan. Patients with reflux esophagitis received famotidine 10 mg twice daily for 2 weeks, then omeprazole 10 mg once daily for 2 weeks. Thereafter, patients were switched to famotidine 10 mg twice daily for a third 2-weekperiod, provided those with a medical condition agreed to continue the study. Patients evaluated the treatment response to each gastrointestinal symptom using a predefined patient questionnaire and gastrointestinal symptom rating scale (GSRS).
Results
161 patients entered the study, of whom 8 were excluded from all analyses due to lack of participation following entry. Overall symptom improvement rate (n = 130) at week 4, after the 2-week omeprazole treatment, was 75.4% and this was significantly higher than that after the first 2-week famotidine treatment (41.5%) at week 2. In patients (n = 36) who completed 6 weeks of treatment, 2-week omeprazole treatment at week 4 showed a significantly higher overall symptom improvement rate compared with both the first 2-week and third 2-week famotidine treatments.
Conclusions
Omeprazole was superior to famotidine for treatment of upper abdominal symptoms in patients with reflux esophagitis, which suggested that gastric acid might be a cause not only of reflux symptoms, but also of ulcer symptoms and dysmotility symptoms such as epigastric pain and feeling of fullness in reflux esophagitis.





Similar content being viewed by others
References
Suzuki H, Hibi T, Marshall BJ. Helicobacter pylori: present status and future prospects in Japan. J Gastroenterol. 2007;42:1–15.
Stanghellini V. Three-month prevalence rate of gastrointestinal symptoms and the influence of demographic factors: results from the Domestic/International Gastroenterology Surveillance (DIGEST). Scand J Gastroenterol. 1999;231:20–8.
Tougas G, Chen Y, Hwang P, Liu MM, Eggleston A. Prevalence and impact of upper gastrointestinal symptoms in the Canadian population: findings from the DIGEST study. Am J Gastroenterol. 1999;94:2845–54.
Thomson ABR, Barkun AN, Armstrong D, Chiba N, White RJ, Daniels S, et al. The prevalence of clinically significant upper gastrointestinal findings in primary care patients with uninvestigated dyspepsia: the Canadian adult dyspepsia empiric treatment-prompt endoscopy (CADET-PE) study. Aliment Pharmacol Ther. 2003;17:1481–91.
Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada J, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130(5):1466–79.
Suzuki H, Nishizawa T, Hibi T. Therapeutic strategies for functional dyspepsia and the information of the Rome III classification. J Gastroenterol. 2006;41:513–23.
Talley NJ, Vakil N. Guidelines for management of dyspepsia. Am J Gastroenterol. 2005;100:2324–37.
Veldhuyzen van Zanten SJO, Chiba N, Armstrong D, Barkun A, Thomson A, Smyth S, et al. A randomized trial comparing omeprazole, ranitidine, cisapride, or placebo in helicobacter pylori negative, primary care physicians with dyspepsia: the CADET-HN study. Am J Gastroenterol. 2005;100:1477–88.
Mason I, Millar LJ, Sheikh RR, Evans WMI, Todd PL, Turbitt ML, et al. The management of acid-related dyspepsia in general practice: a comparison of an omeprazole versus an antacid-alginate/ranitidine management strategy. Compete Research Group [corrected]. Aliment Pharmacol Ther. 1998;12(3):263–71.
Hongo M, Kanatsuka H, Sugawara A, Nagasaki Y, Endo Y, Karahashi K, et al. Primary care in the treatment of functional gastrointestinal symptoms in Japan: prescription preferences and impression of results. Aliment Pharmacol Ther. 2005;21:47–54.
Adachi K, Matsumori Y, Fujisawa T, Kamada T, Kusaka M, Ohumi T, et al. Symptom diversity of patients with reflux esophagitis: effect of omeprazole treatment. J Clin Biochem Nutr. 2006;39:46–54.
Armstrong D, Bennett JR, Blum AL, Dent J, Dombal T, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92.
Laheij RJ, De Koning RW, Horrevorts AM, Rongen RJ, Leo Rossum GM, Wittenman EM, et al. Predominant symptom behavior in patients with persistent dyspepsia during treatment. J Clin Gastroenterol. 2004;38:490–5.
Chiba N. Treat the patients’ main dyspepsia complaint, not the ROME criteria. Am J Gastroenterol. 2004;99(6):1059–62.
van Zanten SV, Armstrong D, Chiba N, et al. Esomeprazole 40 mg once a day in patients with functional dyspepsia: the randomized, placebo-controlled “ENTER” trial. Am J Gastroenterol. 2006;101(9):2096–106.
Talley NJ, Stanghellini V, Heading RC, Koch KL, Malagelada JR, Tytgat GN. Functional gastroduodenal disorders. Gut. 1999;45:II37–42.
Quigley EMM. Motility, heartburn and dyspepsia. Aliment Pharmacol Ther. 1997;11:41–50.
Penagini R, Hebbard G, Horowitz M, Dent J, Bermingham H, Jones K, et al. Motor function of the proximal stomach and visceral perception in patients with gastroesophageal reflux disease. Gut. 1998;42:251–7.
Tosetti C, Stanghellini V, Tucci A, Poli L, Salvioli B, Biasco G, et al. Gastric emptying and dyspeptic symptoms in patients with nonautoimmune fundic atrophic gastritis. Dig Dis Sci. 2000;45(2):252–7.
Tucci A, Poli L, Tosetti C, Biasco G, Grigioni W, Varoli O, et al. Reversal of fundic atrophy after eradication of Helicobacter pylori. Am J Gastroenterol. 1998;93(9):1425–31.
Ebara S, Shirasaka D, Aoyama N, Kachi M, Miki I, Morita Y, et al. The relationship between gastric emptying determined by the breath test and H. pylori. Hepatogastroenterology. 2007;54:613–6.
Suzuki H, Masaoka T, Sakai G, Ishii H, Hibi T. Improvement of gastrointestinal quality of life in cases of Helicobacter pylori-positive functional dyspepsia after successful eradication therapy. J Gastroenterol Hepatol. 2005;20:1652–60.
William DC, Benjamin CYW. American college of gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808–25.
Samsom M, Verhagen M, Henegouwen G, Smout A. Abnormal clearance of exogenous acid and increased acid sensitivity of the proximal duodenum in dyspeptic patients. Gastroenterology. 1999;116(3):515–20.
Miwa H, Nakajima K, Yamaguchi K, Fujimoto K, Veldhuyzen VAN, Zanten SJ, et al. Generation of dyspeptic symptoms by direct acid infusion into the stomach of healthy Japanese subjects. Aliment Pharmacol Ther. 2007;26(2):257–64.
Simren M, Vos R, Janssens J, Tack J. Acid infusion enhances duodenal mechanosensitivity in healthy subjects. Am J Physiol Gastrointest Liver Physiol. 2003;285(2):G309–15.
Lee KJ, Vos R, Janssens J, Tack J. Influence of duodenal acidification on the sensorimotor function of the proximal stomach in humans. Am J Physiol Gastrointest Liver Physiol. 2004;286(2):G278–84.
Coffin B, Chollet R, Flourie B, Lemann M, Franchisseur C, Rambaud JC, et al. Intraluminal modulation of gastric sensitivity to distension: effects of hydrochloric acid and meal. Am J Physiol Gastrointest Liver Physiol. 2001;280(5):G904–9.
Hunt JN, Knox MT. The slowing of gastric emptying by four strong acids and three weak acids. J Physiol. 1972;222(1):187–208.
Hansen AN, Bergheim R, Fagertun H, Lund H, Wiklund I, Moum B. Long-term management of patients with symptoms of gastro-oesophageal reflux disease—a Norwegian randomised prospective study comparing the effects of esomeprazole and ranitidine treatment strategies on health-related quality of life in a general practitioners setting. Int J Clin Pract. 2006;60(1):15–22.
Dimenäs E, Glise E, Hallebäck B, Hernqvist H, Svedlund J, Wiklund I. Well-being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scand J Gastroenterol. 1995;30:1046–52.
Dimenäs E, Carlsson G, Glise H, Israelsson B, Wiklund I. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl. 1996;221:8–13.
Acknowledgments
There was no financial support for the study. We would like to thank the following investigators: Iwakiri R, Sakata H, Tsunada S, Ootani H, Sakata Y, Fujise T, Shimoda R, Shiraishi R, Watanabe K, Akiyama T, Saga Medical School; Okada K, Fujiyamato Onsen Hospital; Nakayama S, Kanzaki Clinic; Matsunaga C, Matsunaga Medical Clinic; Matsunaga K, Arima S, Sasebo Kyosai Hospital; Ogata S, Nakahara S, Mannen K, Saga Prefectural Hospital Koseikan; Kikkawa A, Takeo City Hospital; Tsuruta H, Kawazoe H, National Hospital Organization Ureshino Medical Center; Fujioka Y, Yamaguchi K, Fujioka Hospital; Sakata Y, Yuaikai Oda Hospital; Ishibashi S, Koga Pediatric Medical Hospital; Fujisaki J, Fujisaki Clinic; Mori H, Mori Clinic; Mitsuoka S, Mitsuoka Medical Gastrointestinal Clinic; Maeyama H, Maeyama Medical Gastrointestinal Clinic; Danjo A, Oyama T, Saga Social Insurance Hospital; Noda T, Matsumoto Y, Karatsu Red Cross Hospital; Endo H, Kojima M, Saiseikai Karatsu Hospital; Fukuyama K, Karatsu City Hospital Kitahata; Tomonaga M, Tomonaga Clinic; Tanaka T, Tanaka Medical Clinic; Fujimura T, Yamaguchi Hospital; Ono T, Ono Clinic; Tsuchihashi K, Tsuchihashi Clinic; Terada H, Terada Medical Clinic; Inutsuka S, Inutsuka Hospital; Kuwahara A, Omachi Municipal Hospital; Muto Y, Muto Medical Clinic; Moriyama M, Moriyama Medical Gastrointestinal Clinic; Sakata T, Sakata Clinic; Goto S, Amemori S, Taku City Hospital. Sakagami T, Nakajima K, Yamamoto N, Ohshima T, Hyogo College of Medicine; Yamamura M, Kobe Ekisaikai Hospital; Toyoda T, Nomura Kaihin Hospital; Arai E, Nishinomiya Kyoritsu Neurosurgical Hospital; Sawada Y, Takarazuka Municipal Hospital; Hayashi T, Amagasaki Central Hospital; Kishi K, Meiwa Hospital; Yamaji S, Seiwa Hospital; Hara H, Hara Surgery Clinic; Kuroda Y, Kuroda Clinic; Kishimoto Y, Kishimoto Clinic; Kang K, Asahi Clinic; Yamamoto I, Yamamoto Clinic; Akashi H, Akashi Clinic; Takahashi A, Tsukumo Memorial Hospital. Furuta K, Amano Y, Ishihara S, Sato S, Shimane University School of Medicine; Amano K, Masuda Red Cross Hospital; Okuyama T, Kurashiki Medical Center; Matsumori Y, Takatsuki General Hospital; Higashi R, Shibagaki K, Tottori Municipal Hospital; Niigaki M, Shimane Adult Disease Prevention Center; Hamamoto N, Unnan Municipal General Hospital; Mishima I, Masuda Medical Association Hospital; Nishi K, Hyogo Prefectural Awaji Hospital; Inoue H, Miki City Hospital; Yamada H, Maruno T, Shinko Hospital; Kitajima N, Kasai City Hospital; Kawamura A, Yuaikai Ono Municipal Hospital; Kawashima K, Matsue Seikyo General Hospital; Goubaru Y, Goubaru Clinic; Takatori Y, Takatori Clinic; Yuuki T, Matsue City Hospital; Fukuhara K, Abe Clinic; Honda C, Jusei Hospital; Maekawa T, Kanebo Memorial Hospital. Kamata T, Fujita M, Kawasaki Medical School; Sakakibara T, Sakakibara Hospital; Fujimura Y, Kawasaki Hospital; Kawanishi M, Unno M, Kamao T, Kaneda Hospital; Otani K, Otani Hospital; Yoneda M, Yoneda Medical Clinic; Iguchi D, Ochiai Hospital; Watanabe T, Watanabe Gastrointestinal Surgical Hospital; Miyashita K, Mitsubishi Mizushima Hospital; Koga H, Tanaka T, Tarumi K, Satou Memorial Hospital; Sugiu K, Sugiu Clinic; Nishina H, Shimizu K, Takeda M, Ueda Kinen Hospital; Ohumi T, Ohumi Clinic; Sasaki A, JA Onomichi General Hospital; Hamada H, Mitsubishi Mihara Hospital; Tokumo K, Tokumo Gastrointestinal Hospital; Suzuki T, Suzuki Medical Gastrointestinal Clinic; Miyajima N, Kasaoka Daiichi Hospital; Sano T, Sano Medical Clinic; Tanaka R, Kurashiki Heisei Hospital; Koduka K, Koduka Clinic; Kariya K, Mabi Central Hospital; Moritani Y, Moritani Surgical Clinic; Sato K, Sato Gastrointestinal Surgical Hospital; Murakami Y, Murakami Clinic; Nishioka T, Kanbe Clinic.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kusunoki, H., Kusaka, M., Kido, S. et al. Comparison of the effects of omeprazole and famotidine in treatment of upper abdominal symptoms in patients with reflux esophagitis. J Gastroenterol 44, 261–270 (2009). https://doi.org/10.1007/s00535-009-0003-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-009-0003-4