Abstract
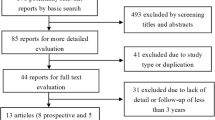
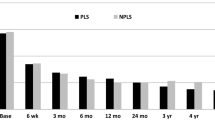
SWISSspine is a so-called pragmatic trial for assessment of safety and efficiency of total disc arthroplasty (TDA). It follows the new health technology assessment (HTA) principle of “coverage with evidence development”. It is the first mandatory HTA registry of its kind in the history of Swiss orthopaedic surgery. Its goal is the generation of evidence for a decision by the Swiss federal office of health about reimbursement of the concerned technologies and treatments by the basic health insurance of Switzerland. During the time between March 2005 and 2008, 427 interventions with implantation of 497 lumbar total disc arthroplasties have been documented. Data was collected in a prospective, observational multicenter mode. The preliminary timeframe for the registry was 3 years and has already been extended. Data collection happens pre- and perioperatively, at the 3 months and 1-year follow-up and annually thereafter. Surgery, implant and follow-up case report forms are administered by spinal surgeons. Comorbidity questionnaires, NASS and EQ-5D forms are completed by the patients. Significant and clinically relevant reduction of low back pain VAS (70.3–29.4 points preop to 1-year postop, p < 0.0001) leg pain VAS (55.5–19.1 points preop to 1-year postop, p < 0.001), improvement of quality of life (EQ-5D, 0.32–0.73 points preop to 1-year postop, p < 0.001) and reduction of pain killer consumption was revealed at the 1-year follow-up. There were 14 (3.9%) complications and 7 (2.0%) revisions within the same hospitalization reported for monosegmental TDA; there were 6 (8.6%) complications and 8 (11.4%) revisions for bisegmental surgery. There were 35 patients (9.8%) with complications during followup in monosegmental and 9 (12.9%) in bisegmental surgery and 11 (3.1%) revisions with new hospitalization in monosegmental and 1 (1.4%) in bisegmental surgery. Regression analysis suggested a preoperative VAS “threshold value” of about 44 points for increased likelihood of a minimum clinically relevant back pain improvement. In a short-term perspective, lumbar TDA appears as a relatively safe and efficient procedure concerning pain reduction and improvement of quality of life. Nevertheless, no prediction about the long-term goals of TDA can be made yet. The SWISSspine registry proofs to be an excellent tool for collection of observational data in a nationwide framework whereby advantages and deficits of its design must be considered. It can act as a model for similar projects in other health-care domains.







Similar content being viewed by others
References
Baur-Melnyk A, Birkenmaier C, Reiser MF (2006) Lumbale Bandscheibenendoprothesen: Indikationen, Biomechanik, Typen und radiologische Kriterien. Radiologe 46:768–778. doi:10.1007/s00117-006-1356-9
Bertagnoli R, Yue JJ, Shah RV, Nanieva R, Pfeiffer F, Fenk-Mayer A, Kershaw T, Husted DS (2005) The treatment of disabling single-level lumbar discogenic low back pain with total disc arthroplasty utilizing the prodisc prosthesis: a prospective study with 2-year minimum follow-up. Spine 30:2230–2236. doi:10.1097/01.brs.0000182217.87660.40
Cochrane AL (1989) Archie Cochrane in his own words. Selections arranged from his 1972 introduction to “Effectiveness and Efficiency: Random Reflections on the Health Services” 1972. Control Clin Trials 10:428–433. doi:10.1016/0197-2456(89)90008-1
de Kleuver M, Oner FC, Jacobs WC (2003) Total disc replacement for chronic low back pain: background and a systematic review of the literature. Eur Spine J 12:108–116
Deyo RA, Nachemson A, Mirza SK (2004) Spinal-fusion surgery—the case for restraint. N Engl J Med 350:722–726. doi:10.1056/NEJMsb031771
Errico TJ (2005) Lumbar disc arthroplasty. Clin Orthop Relat Res 435:106–117. doi:10.1097/01.blo.0000165718.22159.d9
Fritzell P, Hagg O, Nordwall A (2003) Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J 12:178–189
Grevitt M, Pande K, O’Dowd J, Webb J (1998) Do first impressions count? A comparison of subjective and psychologic assessment of spinal patients. Eur Spine J 7:218–223. doi:10.1007/s005860050059
Hägg O, Fritzell P, Ekselius L, Nordwall A (2003) Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish Lumbar Spine Study. Eur Spine J 12:22–33
Hägg O, Fritzell P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12:12–20
Hutton J, Trueman P, Henshall C (2007) Coverage with evidence development: an examination of conceptual and policy issues. Int J Technol Assess Health Care 23:425–432. doi:10.1017/S0266462307070651
Pellise F, Hernandez A, Vidal X, Minguell J, Martinez C, Villanueva C (2007) Radiologic assessment of all unfused lumbar segments 7.5 years after instrumented posterior spinal fusion. Spine 32:574–579. doi:10.1097/01.brs.0000256875.17765.e6
Putzier M, Funk JF, Schneider SV, Gross C, Tohtz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F (2006) Charite total disc replacement—clinical and radiographical results after an average follow-up of 17 years. Eur Spine J 15:183–195. doi:10.1007/s00586-005-1022-3
Tropiano P, Huang RC, Girardi FP, Marnay T (2003) Lumbar disc replacement: preliminary results with ProDisc II after a minimum follow-up period of 1 year. J Spinal Disord Tech 16:362–368
Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA 296:2451–2459. doi:10.1001/jama.296.20.2451
Acknowledgments
We are indebted to Prof. M. Aebi and all staff members of the Institute for Evaluative Research in Orthopaedic Surgery involved in the SWISSpine project. Without his belief in the absolute necessity of outcome documentation, the vision of an academic data clearing house with proprietary data collection system and the endurance of turning this vision into reality in the past 8 years, the SWISSspine registry would not have become a successful postmarket surveillance project within such a short time frame. We thank Daniel Dietrich, PhD, for statistical consulting in all analyses presented in the current article. We are thankful to SGS and the SWISSspine registry group who made this research possible by populating the database with their valuable and much appreciated entries. Aebi M, Baerlocher C, Baur M, Berlemann U, Binggeli R, Boos N, Boscherini D, Cathrein P, Etter C, Favre J, Forster T, Grob D, Hasdemir M, Hausmann O, Heini P, Huber J, Jeanneret B, Kast E, Kleinstueck F, Kroeber M, Lattig F, Lutz T, Maestretti G, Marchesi D, Markwalder T, Martinez R, Min K, Morard M, Otten P, Payer M, Porchet F, Ramadan A, Renella R, Richter H, Schaeren S, Schizas C, Schwarzenbach O, Selz T, Sgier F, Stoll T, Tessitore E, Van Dommelen K, Vernet O, Wernli F.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00586-009-0971-3
Rights and permissions
About this article
Cite this article
Schluessmann, E., Diel, P., Aghayev, E. et al. SWISSspine: a nationwide registry for health technology assessment of lumbar disc prostheses. Eur Spine J 18, 851–861 (2009). https://doi.org/10.1007/s00586-009-0934-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-0934-8