Abstract
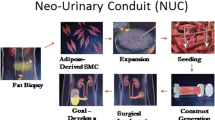
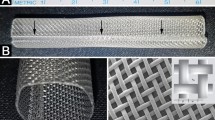
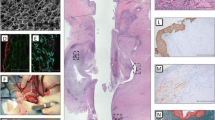
Previous attempts to create small-caliber vascular prostheses have been limited. The aim of this study was to generate tissue-engineered small-diameter vascular grafts using decellularized ureters (DUs). Canine ureters were decellularized using one of four different chemical agents [Triton-X 100 (Tx), deoxycholate (DCA), trypsin, or sodium dodecyl sulfate (SDS)] and the histology, residual DNA contents, and immunogenicity of the resulting DUs were compared. The mechanical properties of the DUs were evaluated in terms of water permeability, burst strength, tensile strength, and compliance. Cultured canine endothelial cells (ECs) and myofibroblasts were seeded onto DUs and evaluated histologically. Canine carotid arteries were replaced with the EC-seeded DUs (n = 4). As controls, nonseeded DUs (n = 5) and PTFE prostheses (n = 4) were also used to replace carotid arteries. The degree of decelularization and the maintenance of the matrix were best in the Tx-treated DUs. Tx-treated and DCA-treated DUs had lower remnant DNA contents and immunogenicity than the others. The burst strength of the DUs was more than 500 mmHg and the maximum tensile strength of the DUs was not different to that of native ureters. DU compliance was similar to that of native carotid artery. The cell seeding test resulted in monolayered ECs and multilayered α-smooth muscle actin-positive cells on the DUs. The animal implantation model showed that the EC-seeded DUs were patent for at least 6 months after the operation, whereas the nonseeded DUs and PTFE grafts become occluded within a week. These results suggest that tissue-engineered DUs may be a potential alternative conduit for bypass surgery.
Similar content being viewed by others
References
American Heart Association. Heart disease and stroke statistics — 2004 update. Coronary heart disease, acute coronary syndrome, angina pectoris. Dallas: American Heart Association, 2004;9–11
Yada I, Wada H, Fujita H. Thoracic and cardiovascular surgery in Japan during 2002: annual report by the Japanese Association for Thoracic Surgery. Jpn J Thorac Cardiovasc Surg 2004;52:491–508
Campeau L, Enjalbert M, Lesperance J, Vaislic C, Grondin CM, Bourassa MG. Atherosclerosis and late closure of aortocoronary saphenous vein grafts: sequential angiographic studies at 2 weeks, 1 year, 5–7 years, and 10–12 years after surgery. Circulation 1983;68:1–7
Hoerstrup SP, Zund G, Sodian R, Schnell AM, Grunenfelder J, Turina MI. Tissue engineering of small-caliber vascular graft. Eur J Cardiothorac Surg 2001;20:164–169
Shin’oka T, Imai Y, Watanabe M, Matsumura G, Kosaka Y, Konuma T, Hibino N, Toyama S, Yamakawa M, Ikada Y, Morita S. Current status of tissue engineering for cardiovascular structures. J Artif Organs 2000;3:102–106
Dohmen PM, Lembcke A, Hotz H, Kivelitz D, Konertz WF. Ross operation with a tissue-engineered heart valve. Ann Thorac Surg 2002;74:1438–1442
Hawkins JA, Hillman ND, Lambert LM, Jones J, Di Russo GB, Profaizer T, Fuller TC, Minich LL, Williams RV, Shaddy RE. Immunogenicity of decellularized cryopreserved allografts in pediatric cardiac surgery: comparison with standard cryopreserved allografts. J Thorac Cardiovasc Surg 2003;126:247–253
Clarke DR, Lust RM, Sun YS, Black KS, Ollerenshaw JD. Transformation of nonvascular acellular tissue matrices into durable vascular conduits. Ann Thorac Surg 2001;71:S433–S436
Matsuura JH, Black KS, Levitt AB, Rosenthal D, Wellons ED, Fallon MT, Davenport CK, Goodman CL, Pagelsen ND, Ollerenshaw JD. Cellular remodeling of depopulated bovine ureter used as an arteriovenous graft in a canine model. J Am Coll Surg 2004;198:778–783
Darby CR, Roy D, Deardon D, Cornall A. Depopulated bovine ureteric xenograft for complex haemodialysis vascular access. Eur J Vasc Endovasc Surg 2006;32:181–186
Warakaulle DR, Evans AL, Cornall AJ, Darby CR, Boardman P, Uberoi R. Diagnostic imaging of, and radiologic intervention for, bovine ureter grafts used as a novel conduit for hemodialysis fistulas. AJR Am J Roentgenol 2007;188:641–646
Bader A, Schilling T, Teebken OE, Brandes G, Herden T, Steinhoff G, Haverich A. Tissue engineering of heart valves — human endothelial cell seeding of detergent-acellularized porcine valves. Eur J Cardiothorac Surg 1998;14:279–284
Cayan S, Chermansky C, Schlote N, Sekido N, Nunes L, Dahiya R, Tanagho EA. The bladder acellular matrix graft in a rat chemical cystitis model: functional and histologic evaluation. J Urology 2002;168:798–804
Steinhoff G, Stock U, Karim N, Mertsching H, Timke A, Meliss RR, Pethig K, Haverich A, Bader A. Tissue engineering of pulmonary heart valves on allogeneic acellular matrix conduit — in vivo restoration of valve tissue. Circulation 2000;102[suppl III]:III50–III55
Booth C, Korossis SA, Wilcox HE, Watterson KG, Kearney JN, Fisher J, Ingham E. Tissue engineering of cardiac valve prostheses I: development and histological characterization of an acellular porcine scaffold. J Heart Valve Dis 2002;11:457–462
Murase Y, Narita Y, Kagami H, Miyamoto K, Ueda Y, Ueda M, Murohara T. Evaluation of mechanical properties of decellularized tissues as scaffolds for engineered small-caliber vascular grafts using intravascular ultrasound. ASAIO J 2006;52:450–455
Lalka SG, Oelker LM, Malone JM, Duhamel RC, Kevorkian MA, Raper BA, Nixon JC, Etchberger KJ, Dalsing MC, Cikrit DF. Acellular vascular matrix: a natural endothelial cell substrate. Ann Vasc Surg 1989;3:108–117
Malone JM, Brendel K, Duhamel RC, Reinert RL. Detergent-extracted small-diameter vascular prostheses. J Vasc Surg 1984;1:181–191
Iwai S, Torikai K, Coppin CM, Sawa Y. Minimally immunogenic decellularized porcine valve provides in situ recellularization as a stentless bioprosthetic valve. J Artif Organs 2007;10:29–35
Huynh T, Abraham G, Murray J, Brockbank K, Hagen PO, Sullivan S. Remodeling of an acellular collagen graft into a physiologically responsive neovessel. Nature Biotech 1999;17:1083–1086
Wilson GJ, Courtman DW, Klement P, Lee JM, Yeger H. Acellular matrix: a biomaterials approach for coronary artery bypass and heart valve replacement. AnnThoracSurg 1995;60:S353–S358
Leyh RG, Wilhelmi M, Walles T, Kallenbach K, Rebe P, Oberbeck A, Herden T, Haverich A, Mertsching H. Acellularized porcine heart valve scaffolds for heart valve tissue engineering and the risk of cross-species transmission of porcine endogenous retrovirus. J Thorac Cardiovasc Surg 2003;126:1000–1004
Ketharanathan V, Christie BA. Bovine ureter as a vascular prosthesis: a preliminary report of an experimental study in the dog. Aust N Z J Surg 1982;52:590–593
Miyata T, Noishiki Y, Matsumae M, Yamane Y. A new method to give antithrombogenicity to biological materials and its successful application to vascular grafts. Trans Am Soc Artif Intern Organs 1983;29:363–368
Field PL. The chemically treated bovine ureter — clinical performance of a novel biological vascular prosthesis. Cardiovasc Surg 2003;11:30–34
Fujisato T, Minatoya K, Niwaya K, Kishida A, Nakatani T, Kitamura S. Vascular tissue regeneration using bioscaffold acellularized by ultrahigh-pressure treatment. Proceedings of 7th Annual Meeting for Tissue Engineering Society International; 2004 Oct 10–13; Lausanne, Switzerland.
Iwasaki K, Ozaki S, Nakazawa T, Imaki Y, Morimoto Y, Ishihara M, Kikuchi M, Umezu M. Development of two types of novel bioreactor for decellularization and in vitro pulsatile conditioning of endothelial cells cultured on the porcine aortic valves. Proceedings of Kanto Regional 9th Annual Meeting for The Japan Society of Mechanical Engineers; 2003 Mar 14–15; Yokohama, Japan.
Abbott WM, Megerman J, Hasson JE, L’Italien G, Warnock DF. Effect of compliance mismatch on vascular graft patency. J Vas Surg 1987;5:376–382
Weston MW, Rhee K, Tarbell JM. Compliance and diameter mismatch affect the wall shear rate distribution near an end-to-end anastomosis. J Biomech 1996;29:187–198
Sonoda H, Urayama S, Takamizawa K, Nakayama Y, Uyama C, Yasui H, Matsuda T. Compliant design of artificial graft: compliance determination by new digital X-ray imaging system-based method. J Biomed Mater Res 2002;60:191–195
Miyamoto K, Sugimoto T, Okada M, Maeda S. Usefulness of polyurethane for small-caliber vascular prostheses in comparison with autologous vein graft. J Artif Organs 2002;5:113–116
Deutsch M, Meinhart J, Fischlein T, Preiss P, Zilla P. Clinical autologous in vitro endothelialization of infrainguinal ePTFE grafts in 100 patients: a 9-year experience. Surgery 1999;126:847–855
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science 1997;275:964–967
Kaushal S, Amiel GE, Guleserian KJ, Shapira OM, Perry T, Sutherland FW, Rabkin E, Moran AM, Schoen FJ, Atala A, Soker S, Bischoff J, Mayer JE. Functional small-diameter neovessels created using endothelial progenitor cells expanded ex vivo. Nature Med 2001;7:1035–1040
He H, Shirota T, Yasui H, Matsuda T. Canine endothelial progenitor cell-line hybrid vascular graft with nonthrombogenic potential. J Thorac Cardiovasc Surg 2003;126:455–464
Allaire E, Muscatelli-Groux B, Mandet C, Guinault AM, Bruneval P, Desgranges P, Clowes A, Méllière D, Becquemin JP. Paracrine effect of vascular smooth muscle cells in the prevention of aortic aneurysm formation. J Vasc Surg 2002;36:1018–1026
Sharp MA, Phillips D, Roberts I, Hands L. A cautionary case: the synergraft vascular prosthesis. Eur J Vasc Endovasc Surg 2004;27:42–44
Narita Y, Hata K, Kagami H, Usui A, Ueda M, Ueda Y. Novel pulse duplicating bioreactor system for tissue-engineered vascular construct. Tissue Eng 2004;10:1224–1233
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narita, Y., Kagami, H., Matsunuma, H. et al. Decellularized ureter for tissue-engineered small-caliber vascular graft. J Artif Organs 11, 91–99 (2008). https://doi.org/10.1007/s10047-008-0407-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-008-0407-6