Abstract
We conducted a study to assess the effect of family-based treatment on adherence amongst HIV-infected parents and their HIV-infected children attending the Mother-To-Child-Transmission Plus program in Kampala, Uganda. Adherence was assessed using home-based pill counts and self-report. Mean adherence was over 94%. Depression was associated with incomplete adherence on multivariable analysis. Adherence declined over time. Qualitative interviews revealed lack of transportation money, stigma, clinical response to therapy, drug packaging, and cost of therapy may impact adherence. Our results indicate that providing ART to all eligible HIV-infected members in a household is associated with excellent adherence in both parents and children. Adherence to ART among new parents declines over time, even when patients receive treatment at no cost. Depression should be addressed as a potential barrier to adherence. Further study is necessary to assess the long-term impact of this family treatment model on adherence to ART in resource-limited settings.
Similar content being viewed by others
Introduction
Globally, there were an estimated 33 million people living with HIV in 2007 (UNAIDS 2008). Women account for half of all people living with HIV worldwide, and nearly 60% of all HIV infections in sub-Saharan Africa (UNAIDS 2008). Among the estimated 3 million people worldwide who were receiving ART at the end of 2007, 61% were female (WHO 2008). About 800,000 adults in Uganda live with HIV/AIDS, giving an HIV prevalence of 6.1%. Of these individuals about 60% are women (UNAIDS/WHO 2008).
While most studies have shown high levels of adherence to ART in resource-constrained settings (Amberbir et al. 2008; Bisson et al. 2008; Byakika-Tusiime et al. 2005; Diabate et al. 2007; Etard et al. 2007; Fong et al. 2003; Landman et al. 2003; Laniece et al. 2003; Laurent et al. 2004; Laurent et al. 2005a, b; Mills et al. 2006b; Nachega et al. 2004; Orrell et al. 2003; Oyugi et al. 2004; Remien et al. 2003; San Lio et al. 2008; Tadios and Davey 2006; Weidle et al. 2002; Weidle et al. 2006; Weiser et al. 2003) there has been little discussion about how HIV+ women balance the demands of adherence to HIV ART, childcare, and antiretroviral adherence among their children who are HIV-infected. Motherhood potentially places particular stress on HIV-infected women due to higher levels of depression, poorer family cohesion, less ability to perform daily functions, and the need to care for HIV-infected children (Murphy et al. 2002). In a study to evaluate whether living with children adversely affects adherence to ART in HIV-infected women, Merenstein et al. (2008) found that adherence to ART was inversely associated with the number of children living in the household. Each additional child reported to be living in the household was associated with a 6% decrease in the odds of ≥95% adherence. The desire to share or ration therapy is a concern for programs that do not provide treatment to the entire family (Crane et al. 2006). This is particularly important in Uganda, due to the high rates of fertility. Uganda has the third highest total fertility rate in Africa, at 6.81, and the third highest crude birth rate worldwide of 48.15 births per 1,000 population (CIA 2008). The specifics of how HIV-infected women balance childcare, adherence to their own medication, and adherence among their children need to be further elucidated. Using data from participants in the MTCT-Plus Program in Kampala Uganda, we examined whether having children in a household affected adherence to ART; the effect on adherence when all eligible HIV-infected members in a household are treated; and the factors associated with incomplete adherence in HIV-infected mothers.
Methods
Participants and Study Setting
The study was conducted among patients attending the MTCT-Plus program at Mulago Hospital in Kampala, Uganda. Mulago Hospital is Uganda’s largest teaching, referral, and research hospital. The MTCT-Plus program enrolls participants from existing prevention of mother to child HIV transmission programs. It is a comprehensive model of family-centered, multidisciplinary care for HIV-infected patients. The “Plus” component provides an essential treatment package of appropriate therapies for mothers and their HIV-infected family members, including basic care for prevention and/or treatment of HIV-related opportunistic infections and treatment with antiretroviral drugs.
Study Description
We conducted a quantitative study to measure adherence among individuals attending the MTCT-Plus program and a qualitative study to understand reasons for incomplete (<95%) adherence among HIV-infected mothers. In order to look at adherence to initial and chronic ART, we recruited individuals who were newly initiating ART and individuals who were on chronic ART. New initiates were followed for 6 months and individuals on chronic treatment received a single assessment.
Recruitment
New Antiretroviral Treatment
Patients initiating ART were recruited if they were antiretroviral (ARV) naïve, residing within 15 km of the city centre, planning to stay within the study area for at least 6 months, and consented to participate. We considered individuals ART-naive if they had never previously taken ART, except for vertical transmission prophylaxis for the women and children. From April 2004 to March 2005 we enrolled a consecutive sample of patients initiating ART at the MTCT-Plus Program clinic. Newly treated individuals received monthly unannounced pill counts and structured interviews, and phlebotomy at baseline, 3 and 6 months.
Stable Antiretroviral Treatment
Patients on stable ART for 2–42 months were identified from the MTCP-plus register. Stably treated individuals underwent a single structured interview and had one unannounced pill count conducted.
Data Collection
After determining eligibility and obtaining written informed consent, the research assistants administered a structured questionnaire in either English or Luganda (the dominant regional language) to obtain socio-demographic characteristics of the participants. The Luganda questionnaire was translated from the original English version and then a second translator back-translated the Luganda questionnaire into English to ensure consistency between the two languages. Mothers or guardians consented for their children below 10 years and children above 10 and below 18 years gave assent to participate, together with consent from their parents. In addition, the research assistants administered the Beck Depression Inventory (BDI) to detect depressive symptoms. This instrument has been used elsewhere in sub-Saharan Africa (Deribe et al. 2008; Kagee 2008; Moosa et al. 2005) and validated in similar settings (Awaitefe 1988; Steele 2003). The validation studies demonstrated high degrees of reliability and validity of the BDI in these settings.
For patients initiating ART, the research assistant did a baseline count of the pills the patient had received from the pharmacy on the day of enrollment. Tracking information, including contact address, telephone, friends’ and relatives’ names, and places where the participants usually spend their time, was collected. Participants were escorted home to map their home location for future follow-up adherence visits.
Adherence Measures
Three measures of adherence were used: unannounced pill counts, 3-day self report and a 30-day visual analogue scale as previously described (Oyugi et al. 2004). Adherence measures were collected monthly for patients initiating therapy and once for patients on stable antiretroviral therapy. At each visit, all three measures of adherence were obtained and reasons for missed pills recorded. On the visual analog scale, participants were asked to mark off on a scale that run from 0 to 100%, the point that best described how well they had taken their pills over the previous 30 days. For children using liquid ARV formulations, the amount of each medication taken between home visits was determined by weighing the medications in their containers at the beginning of the study and at the time of the visit. We used a Proscale PR-500 digital pocket scale to measure the weights. The care takers of the children reported the children’s adherence.
Biologic Measures
Plasma HIV-1 RNA (viral load) and CD4 T cell counts were assessed at baseline and at 24 weeks for patients initiating ART and once for the patients on stable ART, using the Amplicor HIV-1 Monitor, version 1.5 (Roche Diagnostics, Indianapolis, IN) (lower limit of detection, 400 copies per milliliter) and flow cytometry, respectively.
Qualitative Study
Focus Group Discussions (FGDs)
Three FGDs were conducted to understand the factors associated with adherence. The groups were made homogenous to encourage free discussion among people with similar characteristics. Hence, we formed groups of six HIV positive mothers, five HIV positive male partners, and four HIV negative male partners. Discussions were conducted in the local language (Luganda), facilitated by a research assistant well trained in qualitative research methods. The discussions were tape recorded and transcribed and then translated into English. Patients were asked to describe how they initiated antiretroviral medication and the impact of HIV therapy on their health, their household finances, and their family. Interviews were coded according to theme, and analyzed using an inductive method (Miles and Haberman 1994). Analysis was conducted through a systematic reading of all focus group transcripts and the development of a series of codes corresponding to dominant themes. These codes were then used to identify recurrent patterns in the data. Results reported here focus on the themes of adherence and medication cost, and are presented in narrative form in order to highlight the complex social dynamics of medication access and adherence described by patients.
Data Analysis
Socio-demographic characteristics were summarized using medians and means, with standard deviations (SD) for continuous variables and using proportions for categorical variables. Depression was defined as a BDI score of ≥14. For the subjects newly beginning ART, the level of adherence was determined by calculating the average of all individual adherence scores over 6 months. Each measure of adherence was considered separately and an average score for each measure determined. Adherence was also dichotomized at < or ≥95%. Logistic regression models were used to determine predictors of adherence and to adjust for the effects of potential confounders in ART treated adults. There were too few subjects to model predictors of adherence in children. Generalized Estimating Equations (GEE) were used to assess the longitudinal effect of time on adherence. Bootstrap standard errors were used to make inferences. All statistical tests were two-sided and considered significant at α = 0.05. Ninety-five percent confidence intervals were estimated for the results.
Results
Baseline Characteristics
One hundred seventy-seven participants were enrolled in the study: 75 patients newly initiating ART and 102 on stable ART. A detailed description of the participants is given in Table 1. Of the 177 patients 70% (n = 124) were women and 23% (n = 41) were children below 18 years of age. The median age was 30 (IQR = 25–34) years. Among the adults, the majority of the patients (65%) were married. About half of all the patients (49%, 74/149) had primary education as the highest level of education attained. Some children (n = 25) and adults (n = 3) had not received any formal education. Seventy-one percent (n = 126) of the patients reported having at least one other household member infected with HIV while 38% (n = 68) reported having at least one other member of the household on ART. The median baseline CD4 cell count for the new ART initiates was 161 cells/μl (IQR = 93–197) while that for patients on chronic treatment was 402 cells/μl (IQR = 279–605).
Adherence
New Antiretroviral Therapy
Mean (±SD) adherence was 98.3 ± 7.3, 98.0 ± 6.4 and 98.5 ± 5.7% by 3-day self report, 30-day visual analogue scale and home based unannounced pill count for all observations, respectively. Median adherence by all measures was 100% (Table 2). Sixty-six participants (88%) had ≥95% adherence by pill count. Among those with average adherence ≥95% by pill count, 83% (54/65) achieved virologic suppression (≤400 copies/ml) at 24 weeks of follow-up (Table 4).
Stable Antiretroviral Therapy
The mean, median, and range of the duration of ART prior to enrollment were 11.8 ± 4.5, 11.0 (IQR = 8.0–15.0), and 2–42 months, respectively. Mean (±SD) adherence was, 100 ± 0.0, 100 ± 0.0 and 94.1 ± 10.7% by 3-day self report, 30-day visual analogue scale and pill count, respectively. All patients reported ≥95% adherence, but pill counts showed that only 60% of the patients (61/102) had ≥95% adherence.
Adherence in Children
Mean (±SD) adherence was 98.1 ± 4.6, 97.8 ± 5.7 and 100 ± 0.0 by 3-day self report, 30-day visual analogue scale and pill counts, respectively for children initiating ART (Table 3). Among chronically treated patients, the mean, median, and range of antiretroviral therapy prior to enrollment were 13 ± 7.3, 10.5 (IQR = 8–17.5) and 5–42 months, respectively. Mean (±SD) adherence was 100.0 ± 0.0, 100.0 ± 0.0 and 87.7 ± 14.6 by 3-day self report, 30-day visual analogue scale and pill counts, respectively. All patients [through their guardians] reported ≥95% adherence, but pill counts showed that only 36% of the patients (10/28) had ≥95% adherence.
Predictors of Adherence
In a combined multivariable analysis of individuals newly initiating ART and of those on stable ART among adults, only depression was found to be a predictor of adherence [OR = 0.32; 95% CI (0.11–0.93); P = 0.04]. The number of children in the household was not significantly associated with adherence [OR = 1.0; 95% CI (0.72–1.38); P = 0.99]. In a repeated measures analysis using Generalized Estimating Equations, there was a significant decline in adherence over time on therapy [OR = 0.93; 95% CI (0.88–0.97); P = 0.003]. Patients on ART for each month longer had 0.9 times the odds of achieving ≥95% adherence. Reasons given for incomplete adherence were forgetfulness, side effects, traveling away from home and lack of money for transport to the clinic to refill their prescriptions. Separate multivariable analysis results for new ARV initiates and chronic patients are given in Table 5.
Qualitative Findings
Fifteen individuals participated in the Focus Group Discussions. Eight of these also participated in the quantitative study. Demographic and socioeconomic data were not collected for the qualitative study hence these descriptive data are available only for those participants who also participated in the quantitative study. A summary of the characteristics of the participants for whom we collected descriptive data is given in Table 6. Participants in the qualitative study were similar to those in the quantitative study. We have no reason to think that the seven participants who did not participate in the quantitative study were significantly different from those who participated in the quantitative study given that all participants in the qualitative study were selected from the same pool of ARV-experienced patients in the MTCT+ program. Adherence rates were comparable between the two study groups (99.0 ± 2.0 vs. 94.1 ± 10.2). Similar to a previous report in patients on self-pay antiretroviral therapy (Crane et al. 2006); the most common motivator to adhere to ART was the desire to stay alive in order to care and support one’s children and other family members. Improvements in children’s health status motivated their mothers/guardians to ensure that their children adhered to their prescribed medications. As one respondent said,
In my case, this virus made me worry about my child. I would fail to eat food, I would be crying all the time. Whenever I looked at my child he was diminishing, turning into bones. But since my child started taking medicine I became stronger, and I stopped worrying. (HIV-positive mother)
Participants identified their spouses as important sources of adherence support. Spouses reminded them to take their medicines. Type of packaging of medicines was also a factor in adherence. Packaging that separated daily doses was very helpful in keeping track of whether or not that day’s doses had been taken. This packaging was preferred to tablets in bottles and liquid medications.
Self pay therapy has been associated with missed doses (Byakika-Tusiime et al. 2005). The MTCT-Plus program provides ART at no cost to its members. Many participants stated that they would not have had access to antiretroviral medications without MTCT-Plus, because they could not have afforded it. Provision of no-cost therapy to all eligible HIV-infected individuals in the household ensured sustained adherence.
They tell us that a dose for 1 month is 70,000 U Shs [USD 35]; others say the cost reduced to 50,000 U Shs [USD25]. But personally I couldn’t afford 50,000 [USD 25]. Plus that of the child! (HIV-positive mother)
We must thank the organizers of this program, because where we work if you are HIV-positive, your salary is cut 50% to go for treatment. But through this program the medications are free. (HIV-negative father)
As has been reported in other studies (Mills et al. 2006a; Nachega et al. 2004; Weiser et al. 2003), perceived stigma was commonly reported as a barrier to access and adherence to ART.
These days when people come to know that you have AIDS they don’t want to come near you, as if you are an abominable thing (“bakwenyinyala”). You cannot feel free. Wherever you go they start talking, “See that one, she is sick.” (HIV-positive mother)
Women who test HIV-positive through the MTCT-Plus program are required to inform their partners of their HIV status in order to obtain ART for themselves and their family members. Disclosing their status was often very difficult for women, who feared that their partners would blame and/or abandon them upon hearing the news. Some women dealt with this challenge by keeping their HIV infection status a secret until they were able to bring their partner in for testing:
[After testing positive] I went back home and first kept quiet for two days. I asked myself, how can I approach him to tell him? One day when he came back I told him, they checked my blood but they refused to give me the results until I take my spouse in for testing. I convinced him and he accompanied me. (HIV-positive mother)
Clinical response to ART in children was an important factor in reducing stigma. One woman described how giving birth to a healthy baby caused her family to reverse their assumption that she was dying of AIDS and became supportive again:
You scare people so much that they take you out of their thoughts. They think you are dead even before your time, and count you among those who died long ago. And yet you are still alive…. There was a time when I had a skin rash all over and one of my sisters asked, “What is it, what is it?” She said “You look like an infected person.”…. Then when she saw that since giving birth, my baby was not falling sick (the other children used to be sickly), that my baby was looking nice, did not have a rash, and was growing fast she said “I used to think you were infected. I had taken you out of all of my plans.” I responded that “I am not infected, don’t you see my baby?” So that’s where I ended her suspicions about my being sick. Now she knows that I am not infected, which is not true. (HIV-positive mother)
Explaining antiretroviral use to children was cited as a challenge to long-term care of HIV+ children. Parents generally did not tell their children why they were giving them medicine, but some children started to inquire:
The thing that disturbs me is that I always think what will I tell my child when he grows to a level of understanding and he asks me why he is taking drugs. Because even now he asks me, ‘Mummy I no longer cough but why am I still taking drugs every day?’ What will I tell the child? (HIV-positive mother)
Discussion
Near perfect adherence to ART was observed in mothers and children when treatment was provided to all eligible HIV-infected members in the family. These high levels of adherence confirm findings in other resource-limited settings (Byakika-Tusiime et al. 2005; Fong et al. 2003; Landman et al. 2003; Laniece et al. 2003; Laurent et al. 2004; Laurent et al. 2005a, b; Nachega et al. 2004; Orrell et al. 2003; Oyugi et al. 2004; Remien et al. 2003; Weidle et al. 2002; Weiser et al. 2003). Our findings contrast with those of Merenstein et al. (2008), who found an inverse relationship between adherence and the number of children in the family. The major difference between the two studies is that in our study, all household members had an opportunity to be treated and there was complete disclosure of HIV sero-status. Together with Merestein findings, our findings suggest that adherence is supported by a family-based model that promotes disclosure and provides free therapy to all individuals in a household.
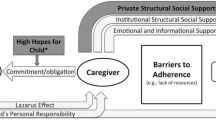
Depression was significantly associated with incomplete adherence. This is consistent with observations in resource-rich settings (Boarts et al. 2006; Gibbie et al. 2007; Turner et al. 2003; Villes et al. 2007; Vranceanu et al. 2008) and resource-limited settings (Amberbir et al. 2008; Campos et al. 2008; Pina Lopez et al. 2008; Poupard et al. 2007). In a meta-analysis of the effects of depression and anxiety on patient adherence, depressed patients had three times the odds of noncompliance compared to non-depressed patients (DiMatteo et al. 2000). The observation that depression is inversely associated with adherence suggests that treatment of depression may improve adherence to medications (Dalessandro et al. 2007). The qualitative study however, did not identify depression as a significant factor for adherence. This is possibly because we did not specifically ask about depression and its effects on adherence during the FGDs. Lack of money for transportation, and stigma were identified as additional barriers to adherence. Ware and Bangsberg have hypothesized that HIV+ individuals in sub-Saharan Africa achieve exceptional ART adherence, despite enormous adherence barriers, because of a synergistic cycle created by the support of close social relationships to overcome adherence barriers (Ware et al. 2008). In the context of this support, ART-treated individuals feel a responsibility to reciprocate this assistance, which is only possible with preserved health and excellent adherence. Reciprocation then strengthens these social bonds and the ability to ask for further assistance. Depression and stigma have an impact on adherence by disrupting the support, or social capital, provided by these reciprocal relationships.
New mothers are at risk for post-partum depression (Wisner et al. 2002). Early parenthood is also a vulnerable time with regard to stigma, as many mothers first learn of their HIV status during delivery. This may explain the observed significant effect of depression among new initiates on ART where as among chronically treated patients this effect [depression] was not observed. These factors may contribute to the decline in adherence we observed in this population. It is interesting that while declining adherence is common in resource-rich settings, it has not yet been reported in resource-limited settings. If fact, two recent longitudinal studies found no decline in adherence (Bangsberg et al. 2008; Muyingo et al. 2008). In the Muyingo et al. study, adherence was good (>95%) for 87% of the participants in the first 4 weeks and this proportion improved over the first year of treatment. Our population of new parents may be particularly vulnerable to the impact of stigma and depression. Interventions to reduce depression and stigma among new HIV+ parents may be an important strategy to maintain adherence in resource-limited settings.
There have been concerns about development of resistance to antiretroviral drugs with increased use of a single dose of nevirapine (Sd-NVP) for prophylaxis of MTCT in HIV+ women and in infants who nevertheless become infected (McIntyre 2006). In our study, where all women and children had been exposed to Sd-NVP, 83% of those with adherence ≥95% achieved suppression of HIV (≤400 copies/ml) at 24 weeks of follow-up. While we did not test for antiretroviral drug resistance, our results suggest that the majority of highly adherent women and children exposed to Sd-NVP at delivery nevertheless achieved suppression of HIV. One limitation in this interpretation, however, is that we did not collect information on the time from delivery to the time of initiating ART. Lockman et al. (2007) found that Sd-NVP is not associated with treatment response when ART is initiated more than 6 months after Sd-NVP in the mother and child (Lockman et al. 2007).
Two of our adherence measures were by self-report. This could introduce information bias and misclassification of participants into adherence categories with respect to these measures. Our self-report measures generally produced results similar to the objective measure of adherence [unannounced pill counts]. Our analysis was based on the unannounced pill counts. The discrepancy between the proportion of patients with adequate adherence (≥95%) between the objective measure and the subjective measures (60 vs. 100% for all subjects and 36 vs. 100% in children) suggests that the objective measure may be more accurate in identifying non-adherent patients, while the subjective measure may only be good for identifying trends in adherence. Our adherence results for the children are comparable to other studies (Nabukeera-Barungi et al. 2007; Williams et al. 2006). Lower levels of adherence in the children suggest that their care givers may not be administering the medications as prescribed. We did not have a sufficient number of children to address predictors of adherence in this group. Another limitation of this study is that our findings were in early participants in the MTCT-Plus program before free antiretroviral therapy was widely available in Uganda. As a result, the participants in this study may not be representative of the larger HIV+ population. Finally, our study did not have a control group that would enable us to evaluate the effectiveness of the MTCT+ model in improving patient adherence to antiretroviral therapy. However the findings from this study generate a hypothesis that may be tested in future studies.
There are some limitations to the focus group data. First, the transcripts did not distinguish between participants, so it was not possible to discern whether participation was roughly equal throughout the group or if the discussion was dominated by the opinions of a few. Also for this reason we were not able to link different statements made over the course of the discussion to particular participants, which made it difficult to get any sense of them as distinct individuals.
In summary, our results suggest that providing ART to all eligible HIV-infected members in a household promotes adherence. Further study will be necessary to assess the long-term impact of this family model on adherence to ART in resource-limited settings. However, we also found a significant decline in adherence over time. Interventions to sustain high levels of adherence should be designed and implemented, one of which is treatment of depression in patients on ART.
References
Amberbir, A., Woldemichael, K., Getachew, S., Girma, B., & Deribe, K. (2008). Predictors of adherence to antiretroviral therapy among HIV-infected persons: A prospective study in Southwest Ethiopia. BioMed Central Public Health, 8, 265.
Awaitefe, A. (1988). The Beck Depression Inventory in relation to some commonly used tests in Nigeria. Nigeria Journal of Basic and Applied Psychology, 1, 23–28.
Bangsberg, D., Emenyonu, N., Andia, I., Bwana, M., Pepper, L., Ragland, K., Weiser, S. D., Hahn, J., Deeks, S. G., & Martin, J. N. (2008). No decline in high levels of electronic pill cap, unannounced home pill count, and patient-reported adherence to free ARV therapy over 12 months in rural Uganda. In Paper presented at the 15th conference on retroviruses and opportunistic infections, Boston, MA, USA. (Abstract # K-170).
Bisson, G. P., Rowh, A., Weinstein, R., Gaolathe, T., Frank, I., & Gross, R. (2008). Antiretroviral failure despite high levels of adherence: Discordant adherence-response relationship in Botswana. Journal of Acquired Immune Deficiency Syndrome, 49, 107–110. doi:10.1097/QAI.0b013e3181820141.
Boarts, J. M., Sledjeski, E. M., Bogart, L. M., & Delahanty, D. L. (2006). The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS and Behavior, 10, 253–261. doi:10.1007/s10461-006-9069-7.
Byakika-Tusiime, J., Oyugi, J. H., Tumwikirize, W. A., Katabira, E. T., Mugyenyi, P. N., & Bangsberg, D. R. (2005). Adherence to HIV antiretroviral therapy in HIV+ Ugandan patients purchasing therapy. International Journal of STD & AIDS, 16, 38–41. doi:10.1258/0956462052932548.
Campos, L. N., Guimaraes, M. D., & Remien, R. H. (2008). Anxiety and depression symptoms as risk factors for non-adherence to antiretroviral therapy in Brazil. AIDS and Behavior [Epub ahead of print]. doi:10.1007/s10461-008-9435-8.
CIA. (2008). The 2008 World fact book. Retrieved August 21, 2008, from https://www.cia.gov/library/publications/the-world-factbook/rankorder/2127rank.html.
Crane, J. T., Kawuma, A., Oyugi, J. H., Byakika, J. T., Moss, A., Bourgois, P., et al. (2006). The price of adherence: Qualitative findings from HIV positive individuals purchasing fixed-dose combination generic HIV antiretroviral therapy in Kampala, Uganda. AIDS and Behavior, 10, 437–442. doi:10.1007/s10461-006-9080-z.
Dalessandro, M., Conti, C. M., Gambi, F., Falasca, K., Doyle, R., Conti, P., et al. (2007). Antidepressant therapy can improve adherence to antiretroviral regimens among HIV-infected and depressed patients. Journal of Clinical Psychopharmacology, 27(1), 58–61. doi:10.1097/JCP.0b013e31802f0dd1.
Deribe, K., Woldemichael, K., Wondafrash, M., Haile, A., & Amberbir, A. (2008). Disclosure experience and associated factors among HIV positive men and women clinical service users in Southwest Ethiopia. BioMed Central Public Health, 8, 81.
Diabate, S., Alary, M., & Koffi, C. K. (2007). Determinants of adherence to highly active antiretroviral therapy among HIV-1-infected patients in Cote d’Ivoire. AIDS (London, England), 21, 1799–1803. doi:10.1097/QAD.0b013e3282a5667b.
DiMatteo, M. R., Lepper, H. S., & Croghan, T. W. (2000). Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine, 160(14), 2101–2107. doi:10.1001/archinte.160.14.2101.
Etard, J. F., Laniece, I., Fall, M. B., Cilote, V., Blazejewski, L., Diop, K., et al. (2007). A 84-month follow up of adherence to HAART in a cohort of adult Senegalese patients. Tropical Medicine & International Health, 12, 1191–1198.
Fong, O. W., Ho, C. F., Fung, L. Y., Lee, F. K., Tse, W. H., Yuen, C. Y., et al. (2003). Determinants of adherence to highly active antiretroviral therapy (HAART) in Chinese HIV/AIDS patients. HIV Medicine, 4, 133–138. doi:10.1046/j.1468-1293.2003.00147.x.
Gibbie, T., Hay, M., Hutchison, C. W., & Mijch, A. (2007). Depression, social support and adherence to highly active antiretroviral therapy in people living with HIV/AIDS. Sexual Health, 4, 227–232. doi:10.1071/SH06062.
Kagee, A. (2008). Symptoms of depression and anxiety among a sample of South African patients living with a chronic illness. Journal of Health Psychology, 13, 547–555. doi:10.1177/1359105308088527.
Landman, R., Schiemann, R., Thiam, S., Vray, M., Canestri, A., Mboup, S., et al. (2003). Once-a-day highly active antiretroviral therapy in treatment-naive HIV-1-infected adults in Senegal. AIDS (London, England), 17, 1017–1022. doi:10.1097/00002030-200305020-00010.
Laniece, I., Ciss, M., Desclaux, A., Diop, K., Mbodj, F., Ndiaye, B., et al. (2003). Adherence to HAART and its principal determinants in a cohort of Senegalese adults. AIDS (London, England), 17(Suppl 3), S103–S108. doi:10.1097/00002030-200317004-00014.
Laurent, C., Kouanfack, C., Koulla-Shiro, S., Nkoue, N., Bourgeois, A., Calmy, A., et al. (2004). Effectiveness and safety of a generic fixed-dose combination of nevirapine, stavudine, and lamivudine in HIV-1-infected adults in Cameroon: Open-label multicentre trial. Lancet, 364, 29–34. doi:10.1016/S0140-6736(04)16586-0.
Laurent, C., Meilo, H., Guiard-Schmid, J. B., Mapoure, Y., Noel, J. M., M’Bangue, M., et al. (2005a). Antiretroviral therapy in public and private routine health care clinics in Cameroon: Lessons from the Douala antiretroviral (DARVIR) initiative. Clinical Infectious Diseases, 41, 108–111. doi:10.1086/430712.
Laurent, C., Ngom Gueye, N. F., Ndour, C. T., Gueye, P. M., Diouf, M., Diakhate, N., et al. (2005b). Long-term benefits of highly active antiretroviral therapy in Senegalese HIV-1-infected adults. Journal Acquired Immune Deficiency Syndrome, 38, 14–17. doi:10.1097/00126334-200501010-00003.
Lockman, S., Shapiro, R. L., Smeaton, L. M., Wester, C., Thior, I., Stevens, L., et al. (2007). Response to antiretroviral therapy after a single, peripartum dose of nevirapine. The New England Journal of Medicine, 356, 135–147. doi:10.1056/NEJMoa062876.
McIntyre, J. A. (2006). Controversies in the use of nevirapine for prevention of mother-to-child transmission of HIV. Expert Opinion on Pharmacotherapy, 7, 677–685. doi:10.1517/14656566.7.6.677.
Merenstein, D. J., Schneider, M. F., Cox, C., Schwartz, R., Weber, K., Robison, E., et al. (2008). Association between living with children and adherence to highly active antiretroviral therapy in the Women’s Interagency HIV Study. Pediatrics, 121, e787–e793. doi:10.1542/peds.2007-1586.
Miles, M. B., & Haberman, M. (1994). Qualitative data analysis (2nd ed.). Thousand Oaks, CA: Sage.
Mills, E. J., Nachega, J. B., Bangsberg, D. R., Singh, S., Rachlis, B., Wu, P., et al. (2006a). Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Medicine, 3, e438. doi:10.1371/journal.pmed.0030438.
Mills, E. J., Nachega, J. B., Buchan, I., Orbinski, J., Attaran, A., Singh, S., et al. (2006b). Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. Journal of the American Medical Association, 296, 679–690. doi:10.1001/jama.296.6.679.
Moosa, M., Jeenah, F., & Vorster, M. (2005). HIV in South Africa—depression and CD4 count. South African Journal of Psychiatry, 11, 12–15.
Murphy, D. A., Marelich, W. D., Dello Stritto, M. E., Swendeman, D., & Witkin, A. (2002). Mothers living with HIV/AIDS: Mental, physical, and family functioning. AIDS Care, 14, 633–644. doi:10.1080/0954012021000005461.
Muyingo, S. K., Walker, A. S., Reid, A., Munderi, P., Gibb, D. M., Ssali, F., et al. (2008). Patterns of individual and population-level adherence to antiretroviral therapy and risk factors for poor adherence in the first year of the DART trial in Uganda and Zimbabwe. Journal of Acquired Immune Deficiency Syndrome, 48, 468–475.
Nabukeera-Barungi, N., Kalyesubula, I., Kekitiinwa, A., Byakika-Tusiime, J., & Musoke, P. (2007). Adherence to antiretroviral therapy in children attending Mulago Hospital, Kampala, Uganda. Annals of Tropical Paediatrics, 27, 123–131. doi:10.1179/146532807X192499.
Nachega, J. B., Stein, D. M., Lehman, D. A., Hlatshwayo, D., Mothopeng, R., Chaisson, R. E., et al. (2004). Adherence to antiretroviral therapy in HIV-infected adults in Soweto, South Africa. AIDS Research and Human Retroviruses, 20, 1053–1056. doi:10.1089/aid.2004.20.1053.
Orrell, C., Bangsberg, D. R., Badri, M., & Wood, R. (2003). Adherence is not a barrier to successful antiretroviral therapy in South Africa. AIDS (London, England), 17, 1369–1375. doi:10.1097/00002030-200306130-00011.
Oyugi, J. H., Byakika-Tusiime, J., Charlebois, E. D., Kityo, C., Mugerwa, R., Mugyenyi, P., et al. (2004). Multiple validated measures of adherence indicate high levels of adherence to generic HIV antiretroviral therapy in a resource-limited setting. Journal of Acquired Immune Deficiency Syndrome, 36, 1100–1102. doi:10.1097/00126334-200408150-00014.
Pina Lopez, J. A., Davila Tapia, M., Sanchez-Sosa, J. J., Togawa, C., & Cazares Robles, O. (2008). Association between stress and depression levels and treatment adherence among HIV-positive individuals in Hermosillo, Mexico. Revista Panamericana de Salud Publica, 23, 377–383.
Poupard, M., Ngom Gueye, N. F., Thiam, D., Ndiaye, B., Girard, P. M., Delaporte, E., et al. (2007). Quality of life and depression among HIV-infected patients receiving efavirenz- or protease inhibitor-based therapy in Senegal. HIV Medicine, 8, 92–95. doi:10.1111/j.1468-1293.2007.00435.x.
Remien, R. H., Hirky, A. E., Johnson, M. O., Weinhardt, L. S., Whittier, D., & Le, G. M. (2003). Adherence to medication treatment: A qualitative study of facilitators and barriers among a diverse sample of HIV+ men and women in four US cities. AIDS and Behavior, 7, 61–72. doi:10.1023/A:1022513507669.
San Lio, M. M., Carbini, R., Germano, P., Guidotti, G., Mancinelli, S., Magid, N. A., et al. (2008). Evaluating adherence to highly active antiretroviral therapy with use of pill counts and viral load measurement in the drug resources enhancement against AIDS and malnutrition program in Mozambique. Clinical Infectious Diseases, 46, 1609–1616. doi:10.1086/587659.
Steele, G. I. (2003). The development and validation of the Xhosa translations of Beck Depression Inventory, the Beck Anxiety Inventory and the Beck Hopelessness Scale. Grahamstown: Rhodes University.
Tadios, Y., & Davey, G. (2006). Antiretroviral treatment adherence and its correlates in Addis Ababa, Ethiopia. Ethiopian Medical Journal, 44, 237–244.
Turner, B. J., Laine, C., Cosler, L., & Hauck, W. W. (2003). Relationship of gender, depression, and health care delivery with antiretroviral adherence in HIV-infected drug users. Journal of General Internal Medicine, 18, 248–257. doi:10.1046/j.1525-1497.2003.20122.x.
UNAIDS. (2008). 2008 Report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS.
UNAIDS/WHO. (2008). Epidemiological fact sheet on HIV and AIDS, Uganda: Core data on epidemiology and response, 2008 update. Geneva: Joint United Nations Programme on HIV/AIDS/World Health Organization.
Villes, V., Spire, B., Lewden, C., Perronne, C., Besnier, J. M., Garre, M., et al. (2007). The effect of depressive symptoms at ART initiation on HIV clinical progression and mortality: Implications in clinical practice. Antiviral Therapy, 12, 1067–1074.
Vranceanu, A. M., Safren, S. A., Lu, M., Coady, W. M., Skolnik, P. R., Rogers, W. H., et al. (2008). The relationship of post-traumatic stress disorder and depression to antiretroviral medication adherence in persons with HIV. AIDS Patient Care and STDs, 22, 313–321. doi:10.1089/apc.2007.0069.
Ware, N., Idoko, J., Kaaya, S., Andia-Biraro, I., Wyatt, M., Agbaji, O., Chlalamilla, G., & Bangsberg, D.R. (2008). A conceptual model to explain adherence success in sub-Saharan Africa. In Paper presented at the 4th international conference on adherence to HIV treatment, Jersey City, NJ.
Weidle, P. J., Malamba, S., Mwebaze, R., Sozi, C., Rukundo, G., Downing, R., et al. (2002). Assessment of a pilot antiretroviral drug therapy programme in Uganda: Patients’ response, survival, and drug resistance. Lancet, 360, 34–40. doi:10.1016/S0140-6736(02)09330-3.
Weidle, P. J., Wamai, N., Solberg, P., Liechty, C., Sendagala, S., Were, W., et al. (2006). Adherence to antiretroviral therapy in a home-based AIDS care programme in rural Uganda. Lancet, 368, 1587–1594. doi:10.1016/S0140-6736(06)69118-6.
Weiser, S., Wolfe, W., Bangsberg, D., Thior, I., Gilbert, P., Makhema, J., et al. (2003). Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. Journal of Acquired Immune Deficiency Syndrome, 34, 281–288. doi:10.1097/00126334-200311010-00004.
WHO. (2008). Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector. Progress Report 2008. Geneva: World Health Organization, UNAIDS, UNICEF.
Williams, P. L., Storm, D., Montepiedra, G., Nichols, S., Kammerer, B., Sirois, P. A., et al. (2006). Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics, 118, e1745–e1756.
Wisner, K. L., Parry, B. L., & Piontek, C. M. (2002). Clinical practice. Postpartum depression. The New England Journal of Medicine, 347, 194–199. doi:10.1056/NEJMcp011542.
Acknowledgments
The authors acknowledge Professor Arthur Reingold for critically reading and editing the paper. We acknowledge Mary Kasango, Muzamir Baryamushanga, Grace Manyangwa, Irene Zawedde, Sarah Nakandi, Ibrahim Kiviri and all MTCT-Plus program staff for their invaluable assistance in participant recruitment, data collection and data management. Our greatest appreciation goes to all patients in the MTCT-Plus program who participated in this study.
Funding
Funding was provided by the Bill and Melinda Gates Grant; the RO-1 MH54907, R21 AA015897, K24 AA015287 grants; and by the Fogarty AIDS International Training and Research Program/University of California, Berkeley (1D43 TW00003).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Byakika-Tusiime, J., Crane, J., Oyugi, J.H. et al. Longitudinal Antiretroviral Adherence in HIV+ Ugandan Parents and Their Children Initiating HAART in the MTCT-Plus Family Treatment Model: Role of Depression in Declining Adherence Over Time. AIDS Behav 13 (Suppl 1), 82–91 (2009). https://doi.org/10.1007/s10461-009-9546-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-009-9546-x