Abstract
Objective
To study the association between consumption of dairy products and calcium intake and risk of breast cancer risk according to menopausal status.
Methods
In a population-based prospective cohort study of 64,904 Norwegian women followed from 1996/1999 through 2006, we examined total dairy consumption and consumption of various dairy products in relation to pre- and postmenopausal breast cancer risk. We also examined breast cancer in relation to calcium intake and to milk consumption during childhood and performed additional analyses corrected for measurement errors in the dietary data. In total, 218 premenopausal and 1,189 postmenopausal incident breast cancer cases were diagnosed during follow-up.
Results
Total dairy, adult, and childhood milk consumption was not associated with either pre- or postmenopausal breast cancer risk. Premenopausal women with the highest consumption of white cheese had half the risk of breast cancer compared to those with the lowest consumption (hazard rate ratio in the 4th quartile vs. the 1st quartile 0.50, 95% confidence interval 0.29–0.87). Total calcium intake tended to be inversely related to premenopausal (hazard rate ratio in the 4th quartile vs. the 1st quartile 0.65, 95% confidence interval 0.39–1.08) and postmenopausal breast cancer (hazard rate ratio in the 4th quartile vs. the 1st quartile 0.85, 95% confidence interval 0.70–1.04). Correcting for measurement errors did not alter the results substantially, nor did exclusion of early cancer cases.
Conclusion
Dairy consumption is not strongly related to breast cancer risk in this prospective study. A non-significant negative association between calcium intake and breast cancer risk was seen, particularly among premenopausal women.
Similar content being viewed by others
Introduction
A high consumption of dairy products is common in many Western populations [1]. The food group often contributes a substantial part of individual’s intake of saturated fat and calcium, and also vitamin D in areas with widespread vitamin D fortification of dairy products. Whereas saturated fat has been suggested to increase the risk of breast cancer [2], calcium and vitamin D—whether supplied through the diet or synthesized in the skin during sun exposure—have been hypothesized to decrease the risk [3]. Also other components of dairy products have been proposed to influence the risk of breast cancer, e.g., an increased risk by environmental contaminants and insulin-like growth factors [4–6], and a decreased risk by conjugated linoleic acids [7, 8]. The fact that dairy products contain a mixture of components that possibly influences breast cancer risk in opposite directions makes the net effect of dairy consumption difficult to settle.
Reviews of epidemiological studies [4, 6], a meta-analysis [9] and a pooled analysis of cohort studies [10] have concluded that there is no evidence for a strong association between dairy consumption and breast cancer risk. Positive [11], negative [12–14], and null findings [15–20] have been reported in cohort studies. Moreover, the findings may vary according to menopausal status [21–23] and between various dairy products [11, 12, 15]. Also for calcium intake the association with breast cancer is inconsistent and may differ with menopausal status [3, 20, 21, 23, 24].
In an earlier study of premenopausal breast cancer in the Norwegian Women and Cancer study (NOWAC), we found an inverse association between milk consumption and breast cancer risk [25]. The age-adjusted incidence rate of breast cancer in Norway is high (72.8 per 100,000 person-years in 2008) [26] and so is the consumption of milk and other dairy products (per capita supply in 2008 was 178 kg) [27]. In the present study, we wanted to examine breast cancer risk and dairy consumption more thoroughly using more detailed dietary data from NOWAC (comprising intake of several dairy products and calcium), a higher number of breast cancer cases, and performing analyses for both pre- and postmenopausal women. Furthermore, as dietary data are prone to measurement errors we also perform corrections for such errors in our risk analyses by applying validation data from a sub-sample of NOWAC [28].
Materials and methods
Subjects and study design
NOWAC is a nationwide cohort study set up at the University of Tromsø, Norway in 1991. It currently comprises more than 165,700 women born 1927–65 randomly drawn from the National Central Person Register [29, 30]. There is a small oversampling from the three most northern counties (n = 13,674). Due to practical workload, financial restraints and methodological sub-studies [31] the baseline enrollment was separated into a number of different sub-series and carried out from 1991 to 1997, and from 2003 to 2006. As the follow-up time for the women in the last inclusion period is very short, only women enrolled from 1991 to 1997 are included in the current paper. The women received a mailed letter of invitation requesting informed consent and a self-instructive questionnaire focusing on certain topics (e.g., diet or sun exposure), and also containing a number of core questions. Detailed dietary questions have been included in the questionnaires since 1996. To expand and update the exposure information, a second questionnaire was from 1998 to 2002 sent to the responders of the baseline mailing conducted in 1991–1997. After one or two reminders, the response rate for the first (baseline) questionnaire (1991–1997) was 57% (102,540/179,387), and 81% (80,835/99,541) for the second questionnaire (1998–2002). The present analyses are restricted to women who gave detailed dietary information in the period 1996–1999, either in their first questionnaire (n = 30,333) or in their second questionnaire (n = 38,184). The Regional Committee for Medical Research Ethics and the Norwegian Data Inspection Board approved the study.
Dietary assessment and nutrient calculations
Dietary information was collected by means of a semi-quantitative food frequency section in the questionnaire, described in details previously [28, 32]. In short, the participants were asked to record their average consumption of various food items during the last year ticking off fixed boxes. Consumption of the following dairy items was asked for: glasses of whole milk, low-fat milk and skimmed milk drunk per week or day, packages of yoghurt eaten per week or day, slices of bread with whole fat brown cheese, low-fat/skimmed brown cheese, whole fat white cheese and low-fat/skimmed white cheese eaten per week, and frequency and amount of ice cream eaten per month or week during the summer and during the rest of the year. In addition, the participants were asked to record what kind of fat (butter or margarine) they usually used on bread, and how often and how much melted or solid fat, full fat sour cream, and fat-reduced sour cream they used for fish meals. Number of glasses of milk consumed per day during childhood was recorded in most of the sub-series. Alcohol intake was calculated from three questions on beer, wine, and spirit consumption.
Daily intake of foods, energy and nutrients was computed using a computation program developed at the Institute of Community Medicine, University of Tromsø, for SAS software. Missing frequencies were treated as null intake and missing portion sizes as the smallest portion unit in the questionnaire, giving a conservative intake estimate [33]. For the women included in the analytic cohort, mode for missing frequencies on the 10 relevant dairy questions was zero; the median was two. The recorded frequency was multiplied with the recorded portion size or a standard portion [34], and transformed into daily food intake in grams. Total dairy consumption was calculated by summing up the consumption of all the items listed above (Table 1), except brown cheese and fat on bread and for fish meals due to the dissimilar nutrient content of these items. Nutrient intake was calculated by multiplying the daily food intake (in grams) of each item with the nutrient content of the item as given in the official Norwegian food composition table [35]. Calcium intake was calculated from all food items in the questionnaire (about 80 questions), excluding supplements. Vitamin D intake was calculated from all food items in the questionnaire including cod liver oil (commonly used in Norway), but no other supplements. At the time of the data collection, margarine and butter were the only foods in Norway fortified with vitamin D.
The intake of dairy foods and calcium was energy-adjusted by using the residual method [36]. That is, we added the residuals of the regression of the intake of dairy foods and calcium on total energy intake, to the predicted intake at mean level of energy intake.
Reproducibility and validity of the food frequency questionnaire
The reproducibility of the questionnaire has been examined in a sub-sample of 1,370 NOWAC participants [37]. Spearman’s correlation coefficient between consumption of milk, yoghurt and cheese in the test (February/March 2002) and in the retest (May/June 2002) questionnaire was 0.74. The relative validity of the questionnaire has been evaluated against four repeated 24-h dietary recalls in a sub-sample of 238 NOWAC women [28]. Compared to the registrations by the 24-h recalls, the questionnaire slightly underestimated the consumption of milk and yoghurt, whereas no significant differences were seen for consumption of cheese and ice cream. Spearman’s correlation coefficient between consumption registered by the questionnaire and by the 24-h recalls was 0.74 (95% confidence intervals (CI) 0.68–0.79) for milk and yoghurt, 0.42 (95% CI 0.31–0.52) for cheese and 0.35 (95% CI 0.23–0.46) for ice cream. As for calcium, the questionnaire underestimated the intake compared to the 24-h recalls (619 vs. 724 mg/day), Spearman’s correlation coefficient between the registrations made by the two methods was 0.50 (95% CI 0.39–0.59), 68% of the subjects were classified into the same or adjacent calcium quintile by the two methods, and 2% were classified in the extreme quintile. Parts of the questionnaire have also been evaluated against fatty acid composition in serum phospholipids [32].
Assessment of other exposures
Information on age at invitation was obtained from National Central Person Register. To handle the effect of potential confounding factors and effect modifying factors the following information was derived from the questionnaire: body weight and height, weight change since age 18, level of physical activity, smoking status, years of education, maternal history of breast cancer, mammography practice, age at menarche, number of children and age at first birth, use of oral contraceptives, menopausal status, and use of hormone replacement therapy (HRT) if postmenopausal.
As only one single recording of menopausal status was available for the present analyses, we assigned all women who were premenopausal when filling out the questionnaire to be postmenopausal when they reached the age of 50 during follow-up. This procedure was followed for women reporting hysterectomy, whereas women reporting bilateral oophorectomy were considered postmenopausal throughout. The age of 50 as a dividing line for menopausal status was chosen based on data from an older sub-sample of NOWAC [38]. Information on self-reported menopausal status and use of HRT has be evaluated against plasma levels of sex hormones and found valid [39].
When checking for interactions between menopausal status and dairy consumption, we examined both the effect of menopausal status at the time of data recording and the effect of menopausal status at end of follow-up. No significant interaction was seen in either of the analyses.
Identification of breast cancer cases
Information from the questionnaire was linked to the Cancer Registry of Norway to identify incident breast cancer cases. In Norway, it is mandatory by law to report all incident cancer cases to the cancer registry, and the registry has an almost complete record of all cancer cases [40–42]. More than 98% of the breast cancers were histologically verified. In situ breast cancers were not regarded as breast cancer. A corresponding linkage to records at Statistics Norway provided information on death and emigration. All linkages were done by means of the unique individual national identification number present in the cohort data set and in the national registers, and ensured complete follow-up.
Analytic cohort
Of the 68,517 women initially in the present cohort, we excluded 2,900 women with a prior cancer diagnosis (any type), one woman with uncertain breast cancer diagnosis, seven women who died and three women who emigrated before the start of the follow-up. We also excluded 104 women who did not answer any of the dairy questions, 585 women for whom the calculated daily energy intake was below 2,500 kJ (n = 516) or above 15,000 kJ (n = 69), and 13 women with implausible age at menopause. Thus, 64,904 women were included in the main analyses. In addition, we performed analyses excluding women who were diagnosed with any kind of cancer (n = 364) or died (n = 41) during the first year of follow-up in order to avoid the possibility that undiagnosed cancer or other severe illness influenced the self-reported data.
Statistical analyses
Person-years of follow-up were calculated as the time elapsed from the date of the returned questionnaire (defined as 3 months after mailing of the invitation letter) to the time of cancer (any type), to time of death or emigration, or to the end of follow-up (31 December 2006), whichever occurred first. Cox proportional hazards regression analyses were carried out to investigate the simultaneous effect of dairy consumption and covariates on breast cancer incidence rate, and hazard rate ratios (HRR) and 95% CI were calculated.
Various categorizations (e.g., quartiles, users–non-users) were applied for the dairy variables. The combined effect of childhood milk consumption and adult dairy consumption was examined by constructing a three-level variable: ‘low consumption,’ defined as no milk consumption as a child or 1st quartile of dairy consumption as adult and not more than next-lowest consumption (1–3 glasses/day)/2nd quartile on the other occasion; ‘high consumption,’ defined as the highest milk consumption as a child (7 or more glasses/day) or 4th quartile of dairy consumption as adult and not less than the next-highest consumption (4–6 glasses/day)/3rd quartile on the other occasions; and ‘moderate consumption,’ defined as all other combinations. The low consumption group was used as the reference category. Calcium intake was examined in quartiles.
Different combinations of the covariates reported at cohort enrollment were employed in multivariable analyses: age at cohort enrollment (5-year categories), height (quartiles: <163, 163–165, 166–169, >169 cm), body mass index (BMI = (wt(kg))/(ht(m)2)) (quartiles: <22.0, 22.0–23.9, 24.0–26.4, >26.4), BMI at age 18 (quartiles: <19.2, 19.2–20.5, 20.6–22.2, >22.2), weight increase since age 18 years (quartiles: <4, 4–9, 10–15, >15 kg), level of physical activity (inactive, moderately active, active), smoking status (current, former, never), education (<11, 11–13, >13 years), maternal history of breast cancer (yes, no), mammography practice (no, every 2nd year or more often, every 2nd year or more seldom), age at menarche (quartiles: <13, 13, 14, >14 years), number of children and age at first birth (nulliparous, 1 child/birth before age 21, 2 or more children/first birth before age 21, 1 child/birth at age 21 or older, 2 or more children/first birth at age 21 or older), use of oral contraceptives (ever, never), and alcohol consumption (0 and tertiles: 0.1–1.52, 1.53–4.13, >4.13 g/day). To assess the influence of HRT (ever, never), we conducted analysis restricted to women who were postmenopausal when completing the questionnaire. Further, we examined any possible confounding effect of intake of fruit, vegetables and potatoes, fat, and vitamin D (all in quartiles). To adjust for energy intake, we categorized the women according to their energy-adjusted intake of each dairy variable (except childhood milk consumption and the combined child/adult consumption variable) and also added total energy intake (in quartiles) to the model.
To test for linear trend in risk, we created a continuous variable by assigning ordinal numbers to each level of exposure and including the continuous variable in the regression models.
Interaction effects were tested using the likelihood ratio test. The assumptions of proportional hazards for the exposures of interest were examined by log–log plots and cumulative hazard plots.
To get an idea about the effect of measurement error in the dietary data, we used the 24-h dietary recalls from the validation study to perform a measurement error correction based on the regression calibration method [43, 44]. Using the energy-adjusted dairy variables and alcohol on its original continuous scale, we constructed multivariate calibration models by regressing the individual means of the recall values of the dairy variables and alcohol on the questionnaire values. Information about total energy intake, age, height, weight increase since age 18, level of physical activity, years of education, maternal history of breast cancer, mammography practice, and use of oral contraceptives were also included in this model. This was done separately for each of the six dairy exposure variables. The calibration models are slightly smaller than the full models used in the main analyses due to the lower number of women included in the calibration. We excluded variables assumed not to be associated with intake of dairy products or alcohol. Data from 180 women were included in the calibration. This is a somewhat lower number than what was originally included in the validation study (n = 238). The 180 women included here are those among the 238 who are also included in the main analysis, so that we were able to collect background information to be used in the calibration. Using the publicly available SAS-macro blinplus (http://www.hsph.harvard.edu/faculty/spiegelman/blinplus.html), we then performed a measurement error correction based on this calibration model.
All reported p values are two-sided, and a significance criterion of p < 0.05 was used to consider an association as statistically significant. The number of subjects included in the separate analyses varies somewhat due to item non-response. Statistical analyses were done by means of the SAS software package, version 9.1.
Results
During 557,753 person-years of follow-up (average 8.6 years), 1,407 of the 64,904 women were diagnosed with breast cancer. Two hundred eighteen of the diagnosed breast cancers were regarded as premenopausal cancer, and 1,189 were regarded as postmenopausal cancer. The mean age at diagnosis was 56.8 years (range 41.1–78.9).
Median daily consumption of dairy products was 174 g, with low-fat milk and skimmed milk as the largest contributors (Table 1). Less than 0.5% of the women did not consume any dairy products at all.
Some characteristics of the cohort according to total dairy consumption are given in Table 2. Most of the known breast cancer risk factors did not vary noticeably across quartiles of dairy consumption. Women in the 3rd quartile of dairy consumption (174–369 g/day) tended to have more years of education and a smaller fraction of them were smokers compared to women in the other quartiles. Both energy intake and daily intake of fat, calcium and vitamin D increased with increasing intake of dairy products. Dairy products were not fortified with vitamin D in Norway at the time of data collection, and the positive association between intake of vitamin D and dairy consumption can largely be ascribed to a higher proportion taking cod liver oil, an item very rich in vitamin D, in the higher quartiles.
The majority of the women (64%) reported drinking 1–3 glasses of milk per day during childhood, 27% reported drinking 4–6 glasses per day and nearly 2% reported drinking 7 glasses or more. Some 6% did not drink milk as a child. Both total dairy consumption and total milk consumption as an adult increased by increasing milk consumption as a child (both: p for trend < 0.001) (data not shown). For instance, women who reported drinking 7 or more glasses of milk as a child had an adult median daily intake of milk of 150 g compared to 118 g for women who drank 1–3 glasses and 0 g for women who did not drink milk as a child.
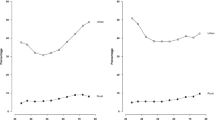
Total dairy consumption was not associated with risk of premenopausal or postmenopausal breast cancer either in age-adjusted analysis or after adjusting for age, energy intake, alcohol intake, height, weight increase since age 18, level of physical activity, years of education, maternal history of breast cancer, mammography practice, age at menarche, number of children and age at first birth, and use of oral contraceptives (Table 3). Additional adjustment for use of HRT among postmenopausal women reduced the number of subjects in the model as this variable was recorded only for women who were postmenopausal when filling in the questionnaire (and not for those who became postmenopausal during follow-up) and reduced the risk estimates marginally (data not shown). Further adjustment for BMI when filling in the questionnaire and at age 18 did not contribute significantly to either the pre- or the postmenopausal model, nor did adjustment for smoking status (data not shown). We also performed analyses adjusting for consumption of fruit, vegetables and potatoes, total intake of fat, and vitamin D intake; the risk estimates for pre- and postmenopausal breast cancer changed negligible (data not shown). Rerunning the multivariate models presented in Table 3 after excluding women who died or got a cancer diagnosis during their first year of follow-up reduced the number of premenopausal breast cancer cases to n = 121 and the number of postmenopausal breast cancer cases to n = 733; the risk estimates were practically identical to those given in Table 3 (data not shown).
Overall, intake of calcium tended to be inversely related to breast cancer risk, but the risk estimates and trends were not statistically significant. Excluding those who died or got a cancer diagnosis during their 1st year of follow-up and rerunning the multivariate model in Table 3 had no effect on the inverse trend for premenopausal breast cancer (p for trend = 0.08), but weakened the trend for postmenopausal breast cancer (p for trend = 0.23).
Like total dairy consumption, total milk consumption (whole, low-fat and skimmed milk) was not associated with neither premenopausal nor postmenopausal breast cancer (Table 4). No noteworthy changes in risk were seen when excluding cancer cases and deaths emerging during the 1st year of follow-up (data not shown). When expressing total milk consumption in terms of fat from milk (median intake 0.8 g/day) there tended to be an increasing risk for premenopausal breast cancer with increasing intake of fat from milk, whereas no association was seen for postmenopausal breast cancer (Table 4). Rerunning the multivariate model in Table 4 excluding those who died or got a cancer diagnosis during their 1st year of follow-up slightly reduced the trend for premenopausal breast cancer (p for trend = 0.10), otherwise there were no changes (data not shown).
Yoghurt consumption was not associated with breast cancer (Table 4). Consumption of white cheese showed a statistically significant inverse association with both premenopausal and postmenopausal breast cancer. Premenopausal women consuming at least 25 g cheese per day (4th quartile) had a 50% reduced risk of breast cancer compared to women consuming <6 g/day (1st quartile) (HRR 0.50, 95% CI 0.29–0.87); for postmenopausal women the risk was reduced by approximately 20% (HRR 0.81, 95% CI 0.66–0.99) (Table 4). The inverse associations were somewhat weakened when early cancer cases and deaths were excluded (both: p for trend = 0.11).
Milk consumption as a child was not related to either pre- or postmenopausal breast cancer (data not shown). Also, when combining milk consumption as a child and adult dairy consumption we did not observe any association with breast cancer risk (Table 4).
As described in the “Materials and methods” section, we also performed a correction for measurement error based on the regression calibration method, on the models presented in Tables 3 and 4, except for the analysis of consumption as a child and as adult. The results from this correction are given in Table 5. Notice that these analyses are based on intake measured on continuous scale. The general trend is that the correction does not alter the initial findings much. The most substantial alteration takes place in the estimated effect of white cheese, where the measurement error corrected analysis shows a non-significant protective effect. It should be noted, however, that the uncertainty associated with the calibration is quite large, leading to wide confidence intervals for the error corrected estimates.
Discussion
In this prospective cohort study, we did not find any significant association between total dairy consumption and risk of pre- or postmenopausal breast cancer. However, there was a tendency of an inverse association for some dairy products, particularly for premenopausal breast cancer. Total calcium intake was inversely related to breast cancer, whereas no association was seen for fat from milk.
Previous studies on dairy consumption and risk of breast cancer have been inconclusive; overall there does not seem to be a strong association either for total dairy consumption or for specific dairy items [4, 6]. In the present study, we saw a 50% decreased risk for premenopausal breast cancer among women consuming 25 g of white cheese per day compared to women consuming less than 6 g/day. However, we found no dose–response relationship. In the analysis corrected for measurement errors an increase of 5 g cheese decreased the risk with 24%. Four previous cohort studies [12, 19, 21, 22] and a pooled analysis of eight cohort studies [10] did not find any significant association between cheese consumption and breast cancer risk (pre and post), whereas in a study of Seventh-day Adventists there was a positive trend with increasing frequency of cheese consumption [15]. Also, the results from case–control studies have been conflicting [4].
White cheese can be a good source for calcium. The most used white cheeses in Norway typically contain about 800 mg calcium/100 g, and cheese contributes 28% of the calcium intake [27]. In the present study we saw a negative association between pre- and postmenopausal breast cancer risk and calcium intake. Calcium intake has been inversely related to risk of breast cancer in some prospective studies [12, 14], although not in all [20, 24]. In two prospective studies among US women and in a small French study, calcium intake was inversely related to premenopausal breast cancer, but not to postmenopausal breast cancer [21–23]. In a Swedish prospective study, pre-diagnostic calcium serum levels were inversely related to premenopausal breast cancer in a dose–response manner, whereas a high level of calcium indicated an increased risk among overweight peri/postmenopausal women [45]. Further, the Women’s Health Initiative randomized trial did not find any reduced incidence of breast cancer among postmenopausal women who had been given calcium and vitamin D supplementation for 7 years [46]. The possibility that any beneficial effect of calcium is modified by menopausal status is in accordance with our finding of a somewhat stronger association for premenopausal than for postmenopausal breast cancer.
Calcium may exercise its anticarcinogenic properties through several mechanisms. In experimental studies increased concentration of calcium decreases cell proliferation and induces differentiation of mammary cells [3]. It may bind and neutralize fatty acids and mutagenic bile acids [6] and may also decrease fat-induced epithelial hyperproliferation in rodent mammary glands [47]. Metabolically calcium is closely related to vitamin D, which also has been shown to influence breast carcinogenesis, and it has been hypothesized that some of the anticarcinogenic effect of calcium may be mediated through vitamin D [3]. For instance, calcium may play an important role in 1,25(OH)2D3 induced apoptosis [48]. In Norway, dairy products were not fortified with vitamin D at the time of data collection, and the correlation between calcium intake and vitamin D intake in the present cohort was not very strong (Pearson’s r = 0.18).
In our previous analysis of milk consumption and premenopausal breast cancer, we found an inverse association between the combined consumption of milk as a child and as an adult and breast cancer [25]. No such association was seen in the present study. Also, our previous analysis showed a significant inverse trend between milk consumption as a child and breast cancer incidence restricted to women younger than 40 years at baseline. In the present study, the youngest women were 41 years at baseline. Childhood dairy intake was not associated with development of breast cancer in a 65-year follow-up of the British Boyd Orr cohort [49], nor was childhood or adolescent consumption of milk or dairy products consistently significantly associated with breast cancer in several studies from North America [21, 50–53]. However, indications of a negative association have been reported in two case–control studies [54, 55].
Our finding that any weak protective effect of some dairy products and of calcium may be stronger or limited to premenopausal breast cancer is in accordance with previous studies [21–23]. The mechanism for this difference is not clear. One hypothesis is that it may be due to the decreased level of insulin growth factors with increasing age, which interact with calcium in promoting growth inhibition in breast cancer cells [5, 23]. Another suggestion points to calcium’s potential as a regulator in estrogen-driven cell proliferation [56].
The strengths of our study are the population-based and prospective design, the large size of the cohort, the complete follow-up with regard to incidence of cancer, death, and emigration, the almost complete histological verification of breast cancer cases, and the opportunity to adjust for all established risk factors for breast cancer. Several questions were asked about dairy consumption and calcium intake was calculated from about 80 semi-quantitative food frequency questions. As dietary data are prone to measurement errors we performed additional analyses correcting the risk estimates for errors by using data from a validation study performed in a subsample of the cohort subjects [28]. As mentioned, the measurement error corrections did not alter the initial findings much. This may be taken as an indication of robustness toward effects of measurement errors.
Possible limitations of our study should also be considered. We did not have access to repeated exposure measures and to information on calcium supplement use, and most non-dietary exposure variables were self-reported for which we do not know the validity, except for menopausal status and use of HRT [39].
We used the linear regression calibration method to adjust for measurement error. This method relies on some assumptions about the structure of possible errors in the reference instrument (the recalls). These errors should be random and independent of both true values and of the errors in the questionnaire. These assumptions may or may not be met in our case. In particular, studies have shown that this last assumption may be doubtful [57, 58]. This means that our method may not be able to fully correct for measurement error. However, we believe that using this instrument and method is our best option to at least gain some insight into the effects of measurement error in these studies.
In summary, in this prospective, population-based study, we found a non-significant inverse association between calcium consumption and risk of breast cancer. Total dairy, adult and childhood milk consumption was not associated with breast cancer risk, whereas a reduced risk was seen for women with the highest consumption of white cheese. The results seem to be robust against effects of measurement error. To confirm any potential protective effect of calcium and/or specific dairy products, more well-designed prospective studies are needed. The protective potential may be largest for premenopausal breast cancer.
References
Hjartaker A, Lagiou A, Slimani N et al (2002) Consumption of dairy products in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort: data from 35,955 24-hour dietary recalls in 10 European countries. Public Health Nutr 5:1259–1271
Bingham SA, Day N (2006) Commentary: fat and breast cancer: time to re-evaluate both methods and results? Int J Epidemiol 35:1022–1024
Cui Y, Rohan TE (2006) Vitamin D, calcium, and breast cancer risk: a review. Cancer Epidemiol Biomarkers Prev 15:1427–1437
Moorman PG, Terry PD (2004) Consumption of dairy products and the risk of breast cancer: a review of the literature. Am J Clin Nutr 80:5–14
Allen NE, Roddam AW, Allen DS et al (2005) A prospective study of serum insulin-like growth factor-I (IGF-I), IGF-II, IGF-binding protein-3 and breast cancer risk. Br J Cancer 92:1283–1287
Parodi PW (2005) Dairy product consumption and the risk of breast cancer. J Am Coll Nutr 24:556S–568S
McCann SE, Ip C, Ip MM et al (2004) Dietary intake of conjugated linoleic acids and risk of premenopausal and postmenopausal breast cancer, Western New York Exposures and Breast Cancer Study (WEB Study). Cancer Epidemiol Biomarkers Prev 13:1480–1484
Larsson SC, Bergkvist L, Wolk A (2009) Conjugated linoleic acid intake and breast cancer risk in a prospective cohort of Swedish Women. Am J Clin Nutr 90:1–5
Boyd NF, Martin LJ, Noffel M, Lockwood GA, Trichler DL (1993) A meta-analysis of studies of dietary fat and breast cancer risk. Br J Cancer 68:627–636
Missmer SA, Smith-Warner SA, Spiegelman D et al (2002) Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies. Int J Epidemiol 31:78–85
Gaard M, Tretli S, Loken EB (1995) Dietary fat and the risk of breast cancer: a prospective study of 25,892 Norwegian women. Int J Cancer 63:13–17
Knekt P, Jarvinen R, Seppanen R, Pukkala E, Aromaa A (1996) Intake of dairy products and the risk of breast cancer. Br J Cancer 73:687–691
Toniolo P, Riboli E, Shore RE, Pasternack BS (1994) Consumption of meat, animal products, protein, and fat and risk of breast cancer: a prospective cohort study in New York. Epidemiology 5:391–397
McCullough ML, Rodriguez C, Diver WR et al (2005) Dairy, calcium, and vitamin D intake and postmenopausal breast cancer risk in the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomarkers Prev 14:2898–2904
Mills PK, Beeson WL, Phillips RL, Fraser GE (1989) Dietary habits and breast cancer incidence among Seventh-day Adventists. Cancer 64:582–590
Ursin G, Bjelke E, Heuch I, Vollset SE (1990) Milk consumption and cancer incidence: a Norwegian prospective study. Br J Cancer 61:454–459
Byrne C, Ursin G, Ziegler RG (1996) A comparison of food habit and food frequency data as predictors of breast cancer in the NHANES I/NHEFS cohort. J Nutr 126:2757–2764
Key TJ, Sharp GB, Appleby PN et al (1999) Soya foods and breast cancer risk: a prospective study in Hiroshima and Nagasaki, Japan. Br J Cancer 81:1248–1256
Voorrips LE, Brants HA, Kardinaal AF, Hiddink GJ, van den Brandt PA, Goldbohm RA (2002) Intake of conjugated linoleic acid, fat, and other fatty acids in relation to postmenopausal breast cancer: the Netherlands Cohort Study on Diet and Cancer. Am J Clin Nutr 76:873–882
Park Y, Leitzmann MF, Subar AF, Hollenbeck A, Schatzkin A (2009) Dairy food, calcium, and risk of cancer in the NIH-AARP Diet and Health Study. Arch Intern Med 169:391–401
Shin MH, Holmes MD, Hankinson SE, Wu K, Colditz GA, Willett WC (2002) Intake of dairy products, calcium, and vitamin d and risk of breast cancer. J Natl Cancer Inst 94:1301–1311
Kesse-Guyot E, Bertrais S, Duperray B et al (2007) Dairy products calcium and the risk of breast cancer: results of the French SU.VI.MAX prospective study. Ann Nutr Metab 51:139–145
Lin J, Manson JE, Lee I-M, Cook NR, Buring JE, Zhang SM (2007) Intakes of calcium and vitamin D and breast cancer risk in women. Arch Intern Med 167:1050–1059
Larsson SC, Bergkvist L, Wolk A (2009) Long-term dietary calcium intake and breast cancer risk in a prospective cohort of women. Am J Clin Nutr 89:277–282
Hjartaker A, Laake P, Lund E (2001) Childhood and adult milk consumption and risk of premenopausal breast cancer in a cohort of 48,844 women—the Norwegian women and cancer study. Int J Cancer 93:888–893
Cancer Registry of Norway (2009) Cancer in Norway 2008—cancer incidence, mortality, survival and prevalence in Norway. Cancer Registry of Norway, Oslo (Norway)
Norwegian Directorate of Health (2008) Trends in the Norwegian diet 2008. Norwegian Directorate of Health, Oslo (Norway)
Hjartaker A, Andersen LF, Lund E (2007) Comparison of diet measures from a food-frequency questionnaire with measures from repeated 24-hour dietary recalls. The Norwegian Women and Cancer Study. Public Health Nutr 10:1094–1103
Lund E, Dumeaux V, Braaten T et al (2008) Cohort profile: the Norwegian Women and Cancer Study NOWAC Kvinner og kreft. Int J Epidemiol 37:36–41
Lund E, Gram IT (1998) Response rate according to title and length of questionnaire. Scand J Soc Med 26:154–160
Hjartaker A, Lund E, Bjerve KS (1997) Serum phospholipid fatty acid composition and habitual intake of marine foods registered by a semi-quantitative food frequency questionnaire. Eur J Clin Nutr 1:736–742
Parr CL, Hjartaker A, Scheel I, Lund E, Laake P, Veierod MB (2008) Comparing methods for handling missing values in food-frequency questionnaires and proposing k nearest neighbours imputation: effects on dietary intake in the Norwegian Women and Cancer study (NOWAC). Public Health Nutr 11:361–370
National Association for Nutrition, Health (1989) Household measures and weights for foods. National Association for Nutrition and Health, Otta (Norway)
National Council for Nutrition, Physical Activity, Norwegian Food Control Authority, Institute for Nutrition Research UoO (2001) The big food composition table. Gyldendal undervisning, Oslo (Norway)
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124:17–27
Parr CL, Veierod MB, Laake P, Lund E, Hjartaker A (2006) Test-retest reproducibility of a food frequency questionnaire (FFQ) and estimated effects on disease risk in the Norwegian Women and Cancer Study (NOWAC). Nutr J 5:4
Bakken K, Eggen AE, Lund E (2001) Hormone replacement therapy in Norwegian women, 1996–1997. Maturitas 40:131–141
Waaseth M, Bakken K, Dumeaux V et al (2008) Hormone replacement therapy use and plasma levels of sex hormones in the Norwegian Women and Cancer postgenome cohort—a cross-sectional analysis. BMC Women’s Health 8:1
Lund E (1981) Pilot study for the evaluation of completeness of reporting to the Cancer Registry. Incidence of cancer in Norway 1978. The Cancer Registry of Norway, Oslo (Norway), pp 11–14
Harvei S, Tretli S, Langmark F (1996) Quality of prostate cancer data in the cancer registry of Norway. Eur J Cancer 32A:104–110
Larsen I, Småstuen M, Parkin DM, Bray F (2007) Data quality at the cancer registry of Norway. In: Bray F (ed) Cancer in Norway 2006—cancer incidence, mortality, survival and prevalence in Norway. Cancer Registry of Norway, Oslo (Norway)
Rosner B, Spiegelman D, Willett WC (1990) Correction of logistic regression relative risk estimates and confidence intervals for measurement error: the case of multiple covariates measured with error. Am J Epidemiol 132:734–745
Spiegelman D, McDermott A, Rosner B (1997) Regression calibration method for correcting measurement-error bias in nutritional epidemiology. Am J Clin Nutr 65:1179S–1186S
Almquist M, Manjer J, Bondeson L, Bondeson AG (2007) Serum calcium and breast cancer risk: results from a prospective cohort study of 7,847 women. Cancer Causes Control 18:595–602
Chlebowski RT, Blackburn GL (2007) Diet and breast cancer recurrence. JAMA 298:2135–2136
Jacobson EA, James KA, Newmark HL, Carroll KK (1989) Effects of dietary fat, calcium, and vitamin D on growth and mammary tumorigenesis induced by 7, 12-dimethylbenz(a)anthracene in female Sprague-Dawley rats. Cancer Res 49:6300–6303
Sergeev IN (2005) Calcium signaling in cancer and vitamin D. J Steroid Biochem Mol Biol 97:145–151
van der Pols JC, Bain C, Gunnell D, Smith GD, Frobisher C, Martin RM (2007) Childhood dairy intake and adult cancer risk: 65-y follow-up of the Boyd Orr cohort. Am J Clin Nutr 86:1722–1729
Hislop TG, Coldman AJ, Elwood JM, Brauer G, Kan L (1986) Childhood and recent eating patterns and risk of breast cancer. Cancer Detect Prev 9:47–58
Michels KB, Rosner BA, Chumlea WC, Colditz GA, Willett WC (2006) Preschool diet and adult risk of breast cancer. Int J Cancer 118:749–754
Potischman N, Weiss HA, Swanson CA et al (1998) Diet during adolescence and risk of breast cancer among young women. J Natl Cancer Inst 90:226–233
Frazier AL, Li L, Cho E, Willett WC, Colditz GA (2004) Adolescent diet and risk of breast cancer. Cancer Causes Control 15:73–82
Pryor M, Slattery ML, Robison LM, Egger M (1989) Adolescent diet and breast cancer in Utah. Cancer Res 49:2161–2167
Shu XO, Jin F, Dai Q et al (2001) Soyfood intake during adolescence and subsequent risk of breast cancer among Chinese women. Cancer Epidemiol Biomarkers Prev 10:483–488
Liu G, Hu X, Chakrabarty S (2009) Calcium sensing receptor down-regulates malignant cell behavior and promotes chemosensitivity in human breast cancer cells. Cell Calcium 45:216–225
Kipnis V, Midthune D, Freedman LS et al (2001) Empirical evidence of correlated biases in dietary assessment instruments and its implications. Am J Epidemiol 153:394–403
Kipnis V, Subar AF, Midthune D et al (2003) Structure of dietary measurement error: results of the OPEN biomarker study. Am J Epidemiol 158:14–21
Acknowledgements
Part of the work was supported by an EXTRA grant from the Norwegian Foundation for Health and Rehabilitation.
Conflict of interest statement
Dr Hjartåker reported having held a lecture paid by Dairy Framers of Canada in 2001 and a lecture paid by the International Dairy Foundation in 2005.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Hjartåker, A., Thoresen, M., Engeset, D. et al. Dairy consumption and calcium intake and risk of breast cancer in a prospective cohort: The Norwegian Women and Cancer study. Cancer Causes Control 21, 1875–1885 (2010). https://doi.org/10.1007/s10552-010-9615-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9615-5