Summary
Systemic chemotherapy using two-drug platinum-based regimens for the treatment of advanced stage non-small cell lung cancer (NSCLC) has largely reached a plateau of effectiveness. Accordingly, efforts to improve survival and quality of life outcomes have more recently focused on the use of molecularly targeted agents, either alone or in combination with standard of care therapies such as taxanes. The molecular chaperone heat shock protein 90 (Hsp90) represents an attractive candidate for therapeutic intervention, as its inhibition results in the simultaneous blockade of multiple oncogenic signaling cascades. Ganetespib is a non-ansamycin inhibitor of Hsp90 currently under clinical evaluation in a number of human malignancies, including NSCLC. Here we show that ganetespib potentiates the cytotoxic activity of the taxanes paclitaxel and docetaxel in NSCLC models. The combination of ganetespib with paclitaxel, docetaxel or another microtubule-targeted agent vincristine resulted in synergistic antiproliferative effects in the H1975 cell line in vitro. These benefits translated to improved efficacy in H1975 xenografts in vivo, with significantly enhanced tumor growth inhibition observed in combination with paclitaxel and tumor regressions seen with docetaxel. Notably, concurrent exposure to ganetespib and docetaxel improved antitumor activity in 5 of 6 NSCLC xenograft models examined. Our data suggest that the improved therapeutic indices are likely to be mechanistically multifactorial, including loss of pro-survival signaling and direct cell cycle effects resulting from Hsp90 modulation by ganetespib. Taken together, these findings provide preclinical evidence for the use of this combination to treat patients with advanced NSCLC.
Similar content being viewed by others
Introduction
Non-small cell lung cancer (NSCLC) accounts for 85% of all cases of lung cancer, the leading cause of cancer-related deaths worldwide [1]. This high mortality is associated, in part, to the fact that a majority of patients present with advanced disease at the time of diagnosis with treatment options limited to systemic therapy. Combination chemotherapy with a platinum-based regimen is the foundation of current treatment for patients with advanced NSCLC [2]. Two-drug combinations consisting of either cisplatin or carboplatin with an additional ‘third-generation’ cytotoxic agent (paclitaxel, docetaxel, gemcitabine, vinorelabine, or pemetrexed) represent the current standard of care for most patients [3]. Paclitaxel and docetaxel comprise the taxane family of microtubule stabilizers widely used in the treatment of advanced NSCLC. Docetaxel, the only agent that is approved for both first- and second-line treatment of NSCLC [4], was also the first drug to establish superior efficacy and tolerability over other third-generation agents when used in combination with platinum compounds [3]. Unfortunately, however, conventional chemotherapy has largely reached a plateau of effectiveness in improving survival rates for lung cancer patients [3, 4].
In recent years the advent of new molecularly-targeted agents and refinements to existing systemic therapies, such as the addition of the vascular endothelial growth factor (VEGF)-binding monoclonal antibody bevacizumab to platinum doublets, the epidermal growth factor receptor (EGFR)-binding monoclonal antibody cetuximab or the use of EGFR inhibitors erlotinib and gefitinib, as well as ELM4-ALK inhibitors such as crizotinib, have improved the therapeutic options for treating this disease [5–7], resulting in modest improvements in overall survival and quality of life for certain patient populations. Despite this progress, treatment outcomes are still considered disappointing [8]. Clearly, the development and use of novel therapeutic strategies to effectively combat NSCLC represents an urgent unmet medical need.
Heat shock protein 90 (Hsp90) is a molecular chaperone required for the post-translational stability and function of numerous key signal transduction proteins, termed ‘client’ proteins, many of which play critical roles in cell growth, differentiation and survival [9, 10]. Importantly, it is now recognized that the chaperoning activity of Hsp90 can become subverted during tumorigenesis to help facilitate malignant progression [9]. Since multiple signaling cascades are regulated by this molecule, the effects of pharmacological blockade of Hsp90 are transmitted to a variety of client proteins and biochemical pathways. Because of this unique characteristic, inhibition of Hsp90 can overcome signaling redundancies and mechanisms of drug resistance commonly observed in many cancers [11–13]. In addition, because tumor cells contain elevated levels of the active form of the chaperone complex relative to normal cells, tumor cells have been shown to be selectively sensitive to Hsp90 inhibition [14]. Thus, Hsp90 provides an attractive molecular target for the development of novel anticancer agents [13, 15, 16].
Ganetespib (formerly STA-9090) is a potent and selective small molecule Hsp90 inhibitor [17] currently being evaluated in multiple clinical trials in solid tumor and hematological malignancies. Recently, a Phase 2b/3 trial was initiated in which it is being combined with docetaxel to treat patients with advanced NSCLC. This indication is considered promising for the application of Hsp90 inhibitors [18] and, importantly, has provided a compelling rationale for the feasibility of combining Hsp90 inhibitors with other therapeutic agents. For example, mutated EGFR, a known Hsp90 client protein, is an important oncogenic driver in a subset of NSCLC patients [19]. Accordingly, Hsp90 inhibitors have demonstrated clinical efficacy when used in combination with EGFR tyrosine kinase inhibitors (TKIs), even in individuals who had progressed on TKI therapy [20]. Of relevance here, Hsp90 inhibitors have also been shown to potentiate the cytotoxic effects of paclitaxel in multiple tumor models, including NSCLC [21–24].
These considerations therefore prompted a more comprehensive evaluation of ganetespib activity in combination with taxanes in preclinical models of NSCLC. In the present study we show that combinatorial treatment results in synergistic antiproliferative and antitumor effects both in vitro and in vivo. Our findings support the potential therapeutic value of ganetespib, particularly in combination with docetaxel, for the treatment of patients with NSCLC.
Materials and methods
Cell lines, antibodies and reagents
All cell lines were obtained from the ATCC (Rockville, MD) and were maintained according to standard techniques at 37°C in 5% (v/v) CO2 using culture medium recommended by the supplier. All primary antibodies were purchased from Cell Signaling Technology (CST, Beverly, MA). Ganetespib [3-(2,4-dihydroxy-5-isopropylphenyl)-4-(1-methyl-1H-indol-5-yl)-1H-1,2,4-triazol-5(4H)-one] was synthesized by Synta Pharmaceuticals Corp. Paclitaxel, docetaxel and vincristine were purchased from LC Laboratories (Woburn, MA).
Cell viability assays
Twenty fours hours after plating in 96 well plates, H1975 cells were dosed with graded concentrations of the indicated compound or DMSO controls for 72 h. AlamarBlue (Invitrogen, Carlsbad, CA) was added (10% v/v) to the cells, and the plates incubated for 3 h and subjected to fluorescence detection in a SpectraMax Plus 384 microplate reader (Molecular Devices, Sunnyvale, CA). Data were normalized to percent of control.
Western blotting
Following ganetespib treatment for 4 or 24 h, H1975 cells were disrupted in lysis buffer (CST) on ice for 10 min. Lysates were clarified by centrifugation and equal amounts of protein resolved by SDS-PAGE before transfer to nitrocellulose membranes (Invitrogen, Carlsbad CA). Membranes were blocked with 5% skim milk in TBS with 0.5% Tween and immunoblotted with the indicated antibodies. The antibody-antigen complex was visualized and quantitated using an Odyssey system (LI-COR, Lincoln, NE).
Cell cycle analysis
Docetaxel- and ganetespib-treated H1975 cells were incubated with the respective compounds (0–30 nM) for 24 h prior to harvest. Cells were fixed, washed and stained with propidium iodide before being analyzed by flow cytometry. The percentage of cells in each phase of the cell cycle (sub-G1, G1, S and G2/M) was determined from the FL2-A histogram.
Median effect analysis
H1975 cells were seeded into the viability assay and combination treatments of ganetespib with paclitaxel, docetaxel or vincristine were performed at fixed, non-constant ratios of the compounds. Drugs were added to cell cultures for 72 h and viability measured by alamarBlue assay. The nature of the combinatorial interactions were evaluated using the combination index (CI) method [25] and values generated using Median Effect analysis (Calcusyn Software; Biosoft, Cambridge, UK).
In vivo NSCLC tumor models
Female immunodeficient CB-17/Icr-Prkdc scid/Crl (SCID) mice (Charles River Laboratories, Wilmington, MA) were maintained in a pathogen-free environment, and all in vivo procedures were approved by the Synta Pharmaceuticals Corp. Institutional Animal Care and Use Committee in accordance with the Guide for Care and Use of Laboratory Animals. NSCLC cell lines were subcutaneously implanted into mice. Mice bearing established tumors (~150 mm3) were randomized into treatment groups (5–8 animals per group) and i.v. dosed via the tail vein with ganetespib, paclitaxel or docetaxel formulated in 10/18 DRD (10% DMSO, 18% Cremophore RH 40, 3.8% dextrose) either as single agents or concurrently on a 1X/week schedule. Tumor volume measurements were made twice weekly and tumor growth inhibition determined as described previously [26].
Statistical analysis
A mixed-model, repeated measures analysis of variance was used to analyze the tumor growth inhibition data. The model included the tumor measurement as dependent variable and treatment (fixed effect), days after tumor implantation (fixed effect), the interaction between treatment and days after tumor implantation (fixed effect) and mice (random effect) as independent variables. P-values are obtained from pair-wise comparisons of each drug to the vehicle. SAS Version 9.1 was used for analysis.
Histological analysis and apoptosis assessment
Mice bearing established H1437 xenografts were administered a single dose of ganetespib (50 mg/kg), docetaxel (4 mg/kg), ganetespib plus docetaxel, or vehicle (10/18 DRD) for 24 h. Tumors were excised and formalin fixed. Paraffin embedded sections were subject to immunohistochemical staining for TUNEL expression using the ApopTag Peroxidase ISOL Apoptosis Detection kit (Millipore, Billerica, MA) according to manufacturers instructions. Images were acquired using a Nikon E800 microscope and Leica DC camera linked to Image-Pro plus software (Media Cybernetics, Inc., Bethesda, MA). Image analysis was performed using a total of 6 sections per slide at 20X magnification. The percentage of apoptotic area was determined by the Average apoptotic area/Average total area. Statistical significance was determined using one-way ANOVA.
Results
Single agent activity in H1975 NSCLC cells
We initially examined the single-agent effects of ganetespib or taxane treatment using the NSCLC cell line H1975. As shown in Fig. 1a, ganetespib reduced cellular viability with low nanomolar potency (IC50 < 10 nM), and exposure to nanomolar concentrations of paclitaxel and docetaxel also resulted in potent cytotoxic effects. H1975 cells were equally sensitive to vincristine, a microtubule-targeted agent of the vinca alkaloid class, which acts via a similar mechanism to the taxanes by causing mitotic cell cycle arrest (Fig. 1a).
Single agent effects on cell viability, Hsp90 client protein degradation and cell cycle distribution in H1975 NSCLC cells. a H1975 cells were treated with ganetespib, paclitaxel, docetaxel or vincristine over a broad dose range (0.1 to 330 nM) for 72 h and cell viability assessed by alamarBlue staining. b Temporal and dose-dependent effects on Hsp90 client proteins by ganetespib. H1975 cells were treated with increasing concentrations of ganetespib for 4 and 24 h and cell lysates subject to immunoblotting using the indicated antibodies. c H1975 cells were treated with the indicated doses of docetaxel or ganetespib and cell cycle distribution determined by flow cytometry 24 h post-treatment
The H9175 cell line expresses EGFRL858/T790M, a constitutively activated, erlotinib-resistant form of EGFR and an Hsp90 client. Ganetespib exposure resulted in a time- and dose-dependent degradation of this oncogenic driver, as well as loss of its downstream effector p-STAT3 (Fig. 1b). Further, inactivation of AKT and GSK3β, Hsp90 client proteins important in regulating apoptosis, was observed with a similar dose response to that of EGFR signaling (Fig. 1b). Together, these data indicate that ganetespib effectively inhibits Hsp90 client proteins in H1975 cells sufficient to account for the cytotoxic response seen following treatment.
Cell cycle analysis (Fig. 1c) confirmed the cellular activity of docetaxel, which induced a dose-dependent mitotic arrest in the G2/M phase of H1975 cells, with concomitant loss of G1 and S phases. Interestingly, ganetespib treatment resulted in an accumulation of cells in the G2/M phase at the highest concentration examined (30 nM) while also reducing the number of cells in S phase. This finding is consistent with our earlier report that ganetespib can additionally modulate cell cycle regulatory proteins to exert its antitumor activity [26].
Ganetespib synergizes with taxanes in vitro
Next we examined the potential for improved therapeutic benefit in NSCLC by combining ganetespib with the standard of care agents paclitaxel and docetaxel. Because of the similarities in mechanism and responses seen in Fig. 1a we also included vincristine in the study. H1975 cells were concurrently treated with ganetespib and each of the three agents using fixed non-constant ratios. Combinatorial activity was assessed using the Median Effect method [25] to determine whether the combinations exhibited antagonistic, additive or synergistic activity (Supplementary Tables 1–3). The results are summarized in the normalized isobolograms shown in Fig. 2. Each point in the isobologram represents the effect of an individual drug combination and the further a point lays from the additive line the stronger the (synergistic or antagonistic) impact of the combination. Combinations of paclitaxel or docetaxel with ganetespib were highly synergistic in these cells (Fig. 2a,b). The vincristine interaction was more modest, although additive and synergistic combinatorial benefit was observed at a number of doses (Fig. 2c). These data clearly indicate that ganetespib can potentiate the effects of taxanes in this NSCLC cell line.
Median effect analysis of the combinatorial activity of ganetespib with paclitaxel, docetaxel and vincristine in H1975 cells in vitro. Drugs were added to H1975 cells at fixed, non-constant concentration ratios for 72 h and viability assessed by Alamar blue assay. Each point represents a CI value for a specific combination of drug concentrations. Data points below the line in the isobologram represent synergy, whereas data points above indicate antagonism between the drug pairs. a Isobologram analysis of ganetespib in combination with paclitaxel. b Isobologram analysis of ganetespib in combination with docetaxel. c Isobologram analysis of ganetespib in combination with vincristine
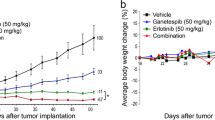
Ganetespib in combination with paclitaxel or docetaxel results in improved efficacy in the H1975 NSCLC xenograft model in vivo
To examine whether the synergistic effects observed in vitro translated to improved efficacy in vivo, mice bearing H1975 xenografts were treated with ganetespib and taxanes, both as single agents and in combination. We have previously determined that the highest non-severely toxic dose (HNSTD) of ganetespib on a weekly dosing regimen is 150 mg/kg [17]. As shown in Fig. 3a, weekly administration of sub-optimal doses of ganetespib (50 mg/kg) and paclitaxel (7.5 mg/kg) reduced tumor growth by 45% and 62%, respectively. Consistent with the in vitro findings, concurrent treatment with both drugs at the same dose level resulted in a significant enhancement of antitumor activity, blocking tumor growth by 93% (i.e., T/C value 7%). The combination treatment was well tolerated, with no significant loss of body weight seen after 3 weeks of dosing (data not shown).
In vivo activity of ganetespib in combination with paclitaxel or docetaxel in H1975 xenografts. a Human NSCLC H1975 tumor-bearing SCID mice were i.v. dosed with ganetespib (50 mg/kg) and paclitaxel (7.5 mg/kg) alone or in combination on a 1X/week schedule for 3 weeks. Data represent the mean and S.E.M. The combination of ganetespib and paclitaxel displayed significantly greater efficacy than either agent alone (*, p < 0.05). b Human NSCLC H1975 tumor-bearing SCID mice were i.v. dosed with ganetespib (100 mg/kg) and docetaxel (5 mg/kg) alone or in combination on a 1X/week schedule for 3 weeks. Data represent mean and S.E.M. The combination of ganetespib and docetaxel resulted in tumor regression (24%)
Next, mice were treated with ganetespib at 100 mg/kg, which inhibited tumor growth by 85%, and a similar level of inhibition (87%) was seen when docetaxel was administered at 5 mg/kg (Fig. 3b). Even at these more efficacious doses, combination treatment with ganetespib and docetaxel resulted in an improved antitumor response, inducing 24% tumor regression (Fig. 3b). Taken together, these results indicate that the combination of ganetespib with taxanes results in a superior therapeutic response compared to the single-agent activity of any of the compounds alone.
Combination ganetespib plus docetaxel treatment inhibits tumor growth in multiple NSCLC xenografts
To extend these findings, we evaluated the antitumor efficacy of ganetespib plus docetaxel treatment in additional NSCLC xenograft models. As shown in Fig. 4a, when delivered as a single agent at 75 mg/kg, ganetespib potently inhibited HCC827 tumor growth (T/C 26%). Docetaxel (4 mg/kg) also inhibited tumor growth in this model (T/C 46%). Importantly, the antitumor effects were enhanced and tumor growth was completely abrogated when the two agents were administered concurrently (Fig. 4a).
Combination of ganetespib and docetaxel induces enhanced antitumor efficacy and apoptosis in NSCLC xenografts. a SCID mice bearing HCC827 NSCLC xenografts were i.v. dosed with ganetespib (75 mg/kg) and docetaxel (4 mg/kg) alone or in combination on a 1X/week schedule for 4 weeks. Data represent the mean and S.E.M. b SCID mice bearing H1437 xenografts were i.v. dosed with ganetespib (50 mg/kg) and docetaxel (4 mg/kg) alone or in combination on a 1X/week schedule for 4 weeks. Data represent the mean and S.E.M. The combination of ganetespib and docetaxel displayed significantly greater efficacy than either agent alone (*, p < 0.05). c H1437 tumor-bearing SCID mice were treated with a single dose of vehicle, ganetespib (50 mg/kg), docetaxel (4 mg/kg) or ganetespib plus docetaxel and tumors harvested 24 h later. Immunohistochemical staining for TUNEL positivity (apoptosis) of tumor cross sections from vehicle control, ganetespib, docetaxel, or ganetespib + docetaxel treated animals. Original magnification, 40X. d Quantitation of TUNEL-positive areas of tumors as described in (C). Data represent the mean and S.D. (*, p < 0.05; one-way ANOVA)
In the H1437 NSCLC model, the combination of ganetespib (50 mg/kg) and docetaxel (4 mg/kg) was significantly more efficacious than either agent alone (Fig. 4b). To make correlations with the cellular responses produced by these treatments, mice bearing H1437 xenografts were treated with a single dose of vehicle, ganetespib, docetaxel or ganetespib plus docetaxel, and their tumors were harvested 24 h later. These tissues were then analyzed by immunohistochemistry to determine their apoptotic index following the treatments (Fig. 4c). Consistent with the effects on tumor growth, apoptotic induction in vivo correlated with the tumor responses of each treatment (Fig. 4d).
In total, combination treatment of ganetespib with docetaxel was evaluated in six in vivo models of NSCLC and the results are summarized in Fig. 5. In five of these models, ganetespib markedly enhanced the antitumor activity of docetaxel, with H2228-derived xenografts as the one exception. However these xenografts manifest the greatest sensitivity to both ganetespib and docetaxel as single agents alone (88% tumor growth inhibition, 30% tumor regression, respectively). Thus it is reasonable to suggest that any potential synergistic effects in this line are likely to be masked at the dosing level examined. Overall, our data show that the addition of ganetespib to docetaxel regimens strongly enhances the antitumor activity of the taxane in vivo.
Comparative antitumor activity of combination ganetespib plus docetaxel treatment in NSCLC xenograft models. Summary of antitumor efficacy of ganetespib and docetaxel either alone or in combination in 6 NSCLC xenograft models.%T/C values are reported. Ganetespib was dosed at 50 mg/kg except for HCC827 (75 mg/kg) and H1975 (100 mg/kg). Docetaxel was dosed at 4 mg/kg except for H1975 (5 mg/kg)
Discussion
Providing improved treatment options for NSCLC remains a daunting challenge for clinicians and oncologists worldwide. Systemic combination chemotherapy is considered the standard of care for patients with advanced NSCLC despite intense efforts at modifying treatments toward improving survival outcomes [3]. The use of standard chemotherapy is restricted to a defined number of cycles, as continuation results in added toxicity without meaningful improvements in progression-free or overall survival [27]. The addition of a third cytotoxic agent to the two-drug combination has been evaluated, however no differences in efficacy were seen and the toxicity profile worsens [28]. More recently, the use of maintenance therapy has evolved as a promising treatment option for NSCLC, based on emerging clinical data using novel molecularly targeted agents or chemotherapeutic drugs that exhibit a more favorable therapeutic index [6, 27].
One strategy to improve objective response rates in patients is through the use of molecularly targeted agents in combination with front line chemotherapeutics, such as bevacizumab and cetuximab. Indeed, combining complimentary agents that possess different presumed mechanisms of action and non-overlapping toxicities has proven important for the control of many human malignancies [29]. This biologically rational approach in NSCLC has revealed that benefit from targeted therapy combinations [5] is typically observed within subsets of patients and correlates with specific tumor histology and/or molecular phenotypes [8]. The coordinate impact of Hsp90 blockade on multiple oncogenic pathways and processes, as well as substantial evidence of the clinical promise of using Hsp90 inhibitors in combination with other therapeutic agents [30], provide a compelling rationale for investigating novel combinatorial strategies. Ganetespib is a next generation Hsp90 inhibitor, structurally unrelated to the prototypic ansamycin class, which exhibits superior pharmacologic and biological properties in terms of potency and safety [17]. Accordingly, an important finding of this study is that ganetespib greatly enhances the efficacy of chemotherapeutics commonly used in the treatment of advanced NSCLC.
Here we showed that ganetespib synergistically potentiated the cytotoxic and antitumor activity of paclitaxel or docetaxel in a panel of NSCLC cell lines both in vitro and in vivo. As a single agent, ganetespib treatment resulted in loss of EGFR client protein expression and blockade of AKT signaling in the H1975 cell line, and significantly suppressed H1975 tumor growth in vivo when used in combination with paclitaxel or docetaxel. These findings are in agreement with a previous report showing that degradation of mutant EGFR and inhibition of AKT activity by the ansamycin Hsp90 inhibitor 17-allyamino-17-demethoxygeldanamycin (17-AAG) could sensitize NSCLC tumors to paclitaxel [24]. In addition, the Hsp90 inhibitor CUDC-305 was recently shown to potentiate paclitaxel activity in H1975 xenografts [31] where it was proposed that this occurred, at least in part, via suppression of AKT. Other studies in breast and ovarian cancer cell lines have also suggested that suppression of AKT activity by 17-AAG resulted in an enhanced sensitivity to the proapoptotic effects of paclitaxel [23, 32]. In this regard, we have additionally found that ganetespib treatment promotes synergistic improvements in docetaxel activity in breast, colon and prostate cell lines (D. Proia, unpublished observations). Taken together, these data imply that the modulation of Hsp90 function and consequent loss of pro-survival pathways may render cancer cells more susceptible to taxane treatment, and that this mechanism is conserved across tumor types.
However, the mechanism(s) by which ganetespib achieves improved therapeutic indices in combination with taxanes is likely to be multifactorial. Other, not mutually exclusive, molecular interactions likely exist - including complementary effects of ganetespib on the cell cycle machinery that enhance taxane activity. Paclitaxel and docetaxel each cause microtubule stabilization, mitotic arrest of cycling tumor cells, and subsequent apoptosis. Ganetespib treatment itself exerts profound effects on cell cycle regulatory proteins, in addition to oncogenic signaling pathways, that contribute to its potent antitumor activity [26]. Further, it is known that mitotic catastrophe can be exacerbated by Hsp90 inhibition in cell lines with defects in the function of the cell checkpoint regulators BRCA1 [33] and RB [22], an effect presumably linked to interference with Hsp90’s role in centrosome organization [34, 35]. The Hsp90 client protein CRAF has also now been shown to localize to the mitotic spindle of proliferating tumor cells to promote progression in a MEK-independent manner [36]. Inhibition of this process results in prometaphase arrest thus providing another avenue for targeted mitotic interference by Hsp90 inhibitors. It is reasonable to suggest, therefore, that modulation of the cell division machinery may represent an important component of the cytotoxic sensitizing property of ganetespib. This premise is supported by our findings that additive and synergistic benefit was also seen for ganetespib in combination with vincristine, another microtubule-targeted agent that induces mitotic arrest prior to cell death.
Notably, we observed that concurrent exposure to ganetespib and docetaxel was significantly more efficacious than either agent alone in 5 of 6 xenograft models in mice bearing established NSCLC tumors. In the one exception, H2228 cells, it appeared that the concentrations tested masked any potential benefit as each drug alone caused pronounced antiproliferative effects. These data have important clinical considerations. Docetaxel is the only agent that is approved for both first- and second-line therapy in advanced NSCLC [4]. Meta-analyses of the current treatment regimens for these patients have shown that docetaxel is associated with better disease control than paclitaxel combinations [3]. In addition, tumor histology does not exert any influence over the activity or efficacy of docetaxel, as opposed other third-generation cytotoxics [3]. Thus, docetaxel represents an optimal front line candidate for combination with a targeted agent such as ganetespib. In light of these observations, we have recently initiated a Phase 2b/3 trial evaluating this combination in patients with refractory NSCLC.
In summary, the capacity of ganetespib to potentiate the cytotoxic effects of taxanes, in particular docetaxel, provides a molecular rationale for combining these agents as a clinical strategy for NSCLC. Overall, the data presented here provide strong preclinical support for the exploration of this combination as a novel therapeutic approach in patients suffering from this disease.
References
Jemal A, Center MM, DeSantis C, Ward EM (2010) Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev 19:1893–1907
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A et al (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346:92–98
Grossi F, Kubota K, Cappuzzo F, de Marinis F, Gridelli C et al (2010) Future scenarios for the treatment of advanced non-small cell lung cancer: focus on taxane-containing regimens. Oncologist 15:1102–1112
Ramalingam S, Belani C (2008) Systemic chemotherapy for advanced non-small cell lung cancer: recent advances and future directions. Oncologist 13(Suppl 1):5–13
Herbst RS, Lynch TJ, Sandler AB (2009) Beyond doublet chemotherapy for advanced non-small-cell lung cancer: combination of targeted agents with first-line chemotherapy. Clin Lung Cancer 10:20–27
Ramalingam SS, Owonikoko TK, Khuri FR (2011) Lung cancer: New biological insights and recent therapeutic advances. CA Cancer J Clin 61:91–112
Gadgeel SM, Bepler G (2011) Crizotinib: an anaplastic lymphoma kinase inhibitor. Future Oncol 7:947–953
Dienstmann R, Martinez P, Felip E (2011) Personalizing therapy with targeted agents in non-small cell lung cancer. Oncotarget 2:165–177
Whitesell L, Lindquist SL (2005) HSP90 and the chaperoning of cancer. Nat Rev Cancer 5:761–772
Hahn JS (2009) The Hsp90 chaperone machinery: from structure to drug development. BMB Rep 42:623–630
Xu W, Neckers L (2007) Targeting the molecular chaperone heat shock protein 90 provides a multifaceted effect on diverse cell signaling pathways of cancer cells. Clin Cancer Res 13:1625–1629
Neckers L (2007) Heat shock protein 90: the cancer chaperone. J Biosci 32:517–530
Banerji U (2009) Heat shock protein 90 as a drug target: some like it hot. Clin Cancer Res 15:9–14
Kamal A, Thao L, Sensintaffar J, Zhang L, Boehm MF et al (2003) A high-affinity conformation of Hsp90 confers tumour selectivity on Hsp90 inhibitors. Nature 425:407–410
Taldone T, Gozman A, Maharaj R, Chiosis G (2008) Targeting Hsp90: small-molecule inhibitors and their clinical development. Curr Opin Pharmacol 8:370–374
Li Y, Zhang T, Schwartz SJ, Sun D (2009) New developments in Hsp90 inhibitors as anti-cancer therapeutics: mechanisms, clinical perspective and more potential. Drug Resist Updat 12:17–27
Ying W, Du Z, Sun L, Foley KP, Proia DA et al (2011) Ganetespib, a unique triazolone-containing Hsp90 inhibitor, exhibits potent antitumor activity and a superior safety profile for cancer therapy. Mol Cancer Ther. doi:10.1158/1535-7163.MCT-11-0755
Trepel J, Mollapour M, Giaccone G, Neckers L (2010) Targeting the dynamic HSP90 complex in cancer. Nat Rev Cancer 10:537–549
Zhang Z, Stiegler AL, Boggon TJ, Kobayashi S, Halmos B (2010) EGFR-mutated lung cancer: a paradigm of molecular oncology. Oncotarget 1:497–514
Sequist LV, Gettinger S, Natale R, Martins R, Lilenbaum R et al (2009) A phase II trial of IPI-504 (retaspimycin hydrochloride), a novel Hsp90 inhibitor, in patients with relapsed and/or refractory stage IIIb or stage IV non-small cell lung cancer (NSCLC) stratified by EGFR mutation status. J Clin Oncol 27(15S):8073
Nguyen DM, Lorang D, Chen GA, Stewart JHT, Tabibi E et al (2001) Enhancement of paclitaxel-mediated cytotoxicity in lung cancer cells by 17-allylamino geldanamycin: in vitro and in vivo analysis. Ann Thorac Surg 72:371–378
Munster PN, Basso A, Solit D, Norton L, Rosen N (2001) Modulation of Hsp90 function by ansamycins sensitizes breast cancer cells to chemotherapy-induced apoptosis in an RB- and schedule-dependent manner. Clin Cancer Res 7:2228–2236
Sain N, Krishnan B, Ormerod MG, De Rienzo A, Liu WM et al (2006) Potentiation of paclitaxel activity by the HSP90 inhibitor 17-allylamino-17-demethoxygeldanamycin in human ovarian carcinoma cell lines with high levels of activated AKT. Mol Cancer Ther 5:1197–1208
Sawai A, Chandarlapaty S, Greulich H, Gonen M, Ye Q et al (2008) Inhibition of Hsp90 down-regulates mutant epidermal growth factor receptor (EGFR) expression and sensitizes EGFR mutant tumors to paclitaxel. Cancer Res 68:589–596
Chou TC, Talalay P (1984) Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul 22:27–55
Proia DA, Foley KP, Korbut T, Sang J, Smith D et al (2011) Multifaceted intervention by the Hsp90 inhibitor ganetespib (STA-9090) in cancer cells with activated JAK/STAT signaling. PLoS One 6:e18552
Owonikoko TK, Ramalingam SS, Belani CP (2010) Maintenance therapy for advanced non-small cell lung cancer: current status, controversies, and emerging consensus. Clin Cancer Res 16:2496–2504
Alberola V, Camps C, Provencio M, Isla D, Rosell R et al (2003) Cisplatin plus gemcitabine versus a cisplatin-based triplet versus nonplatinum sequential doublets in advanced non-small-cell lung cancer: a Spanish Lung Cancer Group phase III randomized trial. J Clin Oncol 21:3207–3213
Kummar S, Chen HX, Wright J, Holbeck S, Millin MD et al (2010) Utilizing targeted cancer therapeutic agents in combination: novel approaches and urgent requirements. Nat Rev Drug Discov 9:843–856
Solit DB, Chiosis G (2008) Development and application of Hsp90 inhibitors. Drug Discov Today 13:38–43
Bao R, Lai CJ, Wang DG, Qu H, Yin L et al (2009) Targeting heat shock protein 90 with CUDC-305 overcomes erlotinib resistance in non-small cell lung cancer. Mol Cancer Ther 8:3296–3306
Solit DB, Basso AD, Olshen AB, Scher HI, Rosen N (2003) Inhibition of heat shock protein 90 function down-regulates Akt kinase and sensitizes tumors to Taxol. Cancer Res 63:2139–2144
Zajac M, Moneo MV, Carnero A, Benitez J, Martinez-Delgado B (2008) Mitotic catastrophe cell death induced by heat shock protein 90 inhibitor in BRCA1-deficient breast cancer cell lines. Mol Cancer Ther 7:2358–2366
Lange BM, Bachi A, Wilm M, Gonzalez C (2000) Hsp90 is a core centrosomal component and is required at different stages of the centrosome cycle in Drosophila and vertebrates. EMBO J 19:1252–1262
de Carcer G (2004) Heat shock protein 90 regulates the metaphase-anaphase transition in a polo-like kinase-dependent manner. Cancer Res 64:5106–5112
Mielgo A, Seguin L, Huang M, Camargo MF, Anand S et al (2011) A MEK-independent role for CRAF in mitosis and tumor progression. Nat Med. doi:10.1038/nm.2464
Acknowledgments
The authors wish to thank Richard Bates who provided drafts and editorial assistance during preparation of this manuscript.
Ethical standards
We declare that all experiments were performed in compliance with all laws of the United States of America.
Conflict of interest
All authors are current or former employees of Synta Pharmaceuticals Corp.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOC 41 kb)
Supplementary Table 2
(DOC 41 kb)
Supplementary Table 3
(DOC 39 kb)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Proia, D.A., Sang, J., He, S. et al. Synergistic activity of the Hsp90 inhibitor ganetespib with taxanes in non-small cell lung cancer models. Invest New Drugs 30, 2201–2209 (2012). https://doi.org/10.1007/s10637-011-9790-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-011-9790-6