Abstract
Introduction
Osteoarticular prosthesis loosening involves recruitment, activation, and differentiation of mononuclear phagocytes, with a complex and still unclear interplay of local and systemic inflammation. We hypothesized that aseptic hip prosthesis loosening is bound to a coordinated systemic and local activation of the mononuclear phagocyte system (MPS), which can be demonstrated by simultaneous assessment of both compartments. We, therefore, compared systemic and synovial inflammatory cytokines, circulating monocyte activation state, and synovial fluid (SF) ability to induce osteoclastic differentiation.
Materials and Methods
Twenty-seven patients undergoing total hip replacement for aseptic loosening were compared to 30 patients receiving total hip prosthesis for primary osteoarthritis.
Results and Discussion
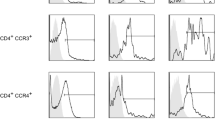
SF from aseptic loosening patients induced a more effective osteoclast-like differentiation of monocytic THP-1 cells in vitro and a proinflammatory pattern of cytokine production in these osteoclast-like cultures. On the contrary, SF from osteoarthritis patients did not favor osteoclastogenesis and exerted an anti-inflammatory effect through IL-10 upregulation and TNF-α inhibition. Peripheral blood monocytes of aseptic loosening patients were primed for activation, with higher TNF-α responses than their counterparts in the osteoarthritis group. Finally, cytokine enrichment in SF versus serum was observed in both patient groups: a fivefold increase in synovial TNF-α in aseptic loosening patients and a 14-fold increase in synovial IL-10 in osteoarthritis patients. The TNF-α/IL-10 ratio was elevated in both systemic and synovial settings from aseptic loosening patients with respect to osteoarthritis patients.
Conclusion
Taken together, our results demonstrate the integrated activation of the MPS and suggest the possible use of cytokines in the laboratory workup of prosthesis aseptic loosening.








Similar content being viewed by others
Abbreviations
- GM-CSF:
-
granulocyte macrophage colony-stimulating factor
- IL:
-
interleukin
- LPS:
-
lipopolysaccharide (endotoxin)
- M-CSF:
-
macrophage colony-stimulating factor
- MPS:
-
mononuclear phagocyte system
- OA:
-
osteoarthritis
- O/THP-1:
-
osteoclast-differentiated THP-1 cells
- RANK:
-
receptor activator of NFκB
- RANKL:
-
receptor activator of NFκB ligand
- SF:
-
synovial fluid
- Th:
-
helper T cell
- THR:
-
total hip revision
- TGFβ1:
-
transforming growth factor-β1
- TNF-α:
-
tumor necrosis factor-α
- TRAP:
-
tartrate-resistant acid phosphatase
References
Goodman S. Wear particles, periprosthetic osteolysis and the immune system. Biomaterials. 2007;28:5044–8. doi:10.1016/j.biomaterials.2007.06.035.
Greenfield EM, Bi Y, Ragab AA, Goldberg VM, Van De Motter RR. The role of osteoclast differentiation in aseptic loosening. J Orthop Res. 2002;20:1–8. doi:10.1016/S0736-0266(01)00070-5.
Mandelin J, Liljeström M, Li TF, Ainola M, Hukkanen M, Salo J, et al. Pseudosynovial fluid from loosened total hip prosthesis induces osteoclast formation. J Biomed Mater Res. 2005;74(B):582–8.
Shen Z, Crotti TN, McHugh KP, Matsuzaki K, Gravallese EM, Bierbaum BE, et al. The role played by cell–substrate interactions in the pathogenesis of osteoclast-mediated peri-implant osteolysis. Arthritis Res Ther. 2006;8:70. doi:10.1186/ar1938.
Haynes DR, Crotti TN, Zreiqat H. Regulation of osteoclast activity in peri-implant tissues. Biomaterials. 2004;25:4877–85. doi:10.1016/j.biomaterials.2004.01.003.
Sabokbar A, Rushton N. Role of inflammatory mediators and adhesion molecules in the pathogenesis of aseptic loosening in total hip arthroplasties. J Arthroplasty. 1995;10:810–6. doi:10.1016/S0883-5403(05)80080-4.
Urban RM, Tomlinson MJ, Hall DJ, Jacobs JJ. Accumulation in liver and spleen of metal particles generated at nonbearing surfaces in hip arthroplasty. J Arthroplasty. 2004;19(S3):94–101. doi:10.1016/j.arth.2004.09.013.
De Haar C, Kool M, Hassing I, Bol M, Lambrecht BN, Pieters R. Lung dendritic cells are stimulated by ultrafine particles and play a key role in particle adjuvant activity. J Allergy Clin Immunol. 2008;121:1246–54. doi:10.1016/j.jaci.2008.01.010.
Tanaka R, Yasunaga Y, Hisatome T, Yamasaki T, Iwamori H, Ochi M. Serum interleukin 8 levels correlates with synovial fluid levels in patients with aseptic loosening of hip prosthesis. J Arthroplasty. 2005;20:1049–54. doi:10.1016/j.arth.2005.03.034.
Adamopoulos IE, Dank L, Itonaga I, Locklin RM, Sabokbar A, Ferguson DJP, et al. Stimulation of osteoclast formation by inflammatory synovial fluid. Virchows Arch. 2006;449:69–77. doi:10.1007/s00428-006-0200-y.
Vignery A. Macrophage fusion: the making of osteoclasts and giant cells. J Exp Med. 2005;202:337–40. doi:10.1084/jem.20051123.
Krohmer G, Koleganova N, Hagjicostas P, Fink B, Berger I. Degenerative changes of the interface membrane as a possible reason for prosthesis loosening. Histol Histopathol. 2008;23:925–33.
Chiang CY, Kyritsis G, Graves DT, Amar S. Interleukin-1 and tumor necrosis factor activities partially account for calvarial bone resorption induced by local injection of lipopolysaccharide. Infect Immun. 1999;67:4231–6.
Clarke SA, Brooks RA, Hobby JL, Wimhurst JA, Myer BJ, Rushton N. Correlation of synovial fluid cytokine levels with histological and clinical parameters of primary and revision total hip and knee replacements. Acta Orthop Scand. 2001;72:491–8. doi:10.1080/000164701753532835.
Holding CA, Findlay DM, Stamenkov R, Neale SD, Lucas H, Dharmapatni ASSK, et al. The correlation of RANK, RANKL and TNFα expression with bone loss volume and polyethylene wear debris around hip implants. Biomaterials. 2006;27:5212–9. doi:10.1016/j.biomaterials.2006.05.054.
Sypniewska G, Lis K, Bilinski PJ. Bone turnover markers and cytokines in joint fluid. Acta Orthop Scand. 2002;73:518–22.
Maynard CL, Weaver CT. Diversity in the contribution of interleukin-10 to T- cell-mediated immune regulation. Immunol Rev 2008;226:219–33.
Sabokbar A, Kudo O, Athanasou NA. Two distinct mechanisms of osteoclast formation and bone resorption in periprosthetic osteolysis. J Orthop Res. 2003;21:73–80.
Li M, Flavell RA. Contextual regulation of inflammation: a duet by transforming growth factor-b and Interleukin-10. Immunity. 2008;28:468–76.
O'Shea JJ, Murray PJ. Cytokine signaling modules in inflammatory responses. Immunity. 2008;28:477–87.
Wang ML, Hauschka PV, Tuan RS, Steinbeck MJ. Exposure to particles stimulates superoxide production by human THP-1 macrophages and avian HD-11EM osteoclasts activated by tumor necrosis factor- and PMA. J Arthroplasty. 2002;17:335–46.
Lubberts E. IL-17/Th17 targeting: on the road to prevent chronic destructive arthritis? Cytokine. 2008;41:84–91.
Ouyang W, Kolls JK, Zheng Y. The biological functions of T helper 17 cell effector cytokines in inflammation. Immunity. 2008;28:454–67.
Tsuchiya S, Yamabe M, Yamaguchi Y, Kobayashi Y, Konno T, Tada K. Establishment and characterization of a human acute monocytic leukemia cell line (THP-1). Int J Cancer. 1980;26:171–6.
Baumann B, Rader CP, Seufert J, Nöth U, Rolf O, Eulert J, et al. Effects of polyethylene and TiAlV wear particles on expression of RANK, RANKL and OPG mRNA. Acta Orthop Scand. 2004;75:295–302.
Rader CP, Sterner T, Jakob F, Schütze N, Eulert J. Cytokine response of human macrophage-like cells after contact with polyethylene and pure titanium particles. J Arthroplasty. 1999;14:840–8.
Soares-Schanoski A, Gomez-Pina V, del Fresno C, Rodriguez-Rojas A, Garcia F, Glaria A, et al. 6-Methylprednisolone down-regulates IRAK-M in human and murine osteoclasts and boosts bone-resorbing activity: a putative mechanism for corticoid-induced osteoporosis. J Leukoc Biol. 2007;82:700–9.
Susa M, Luong-Nguyen NH, Cappellen D, Zamurovic N, Gamse R. Human primary osteoclasts: in vitro generation and applications as pharmacological and clinical assay. J Transl Med. 2004;2:6–17.
Granchi D, Pellacani A, Spina M, Cenni E, Savarino LM, Baldini N, et al. Serum levels of osteoprotegerin and receptor activator of nuclear factor- B ligand as markers of periprosthetic osteolysis. J Bone Joint Surg Am. 2006;88:1501–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flecher, X., Rolland, C., Rixrath, E. et al. Local and Systemic Activation of the Mononuclear Phagocyte System in Aseptic Loosening of Total Hip Arthroplasty. J Clin Immunol 29, 681–690 (2009). https://doi.org/10.1007/s10875-009-9305-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-009-9305-9