Abstract
Introduction
The 2009 swine-origin H1N1 influenza virus (swH1N1) provided an opportunity to study immune responses to a new influenza strain in the context of seasonal influenza vaccination. Our goals were: to assess whether analyzing multiple parameters of immune responsiveness to influenza has an advantage over evaluating hemagglutination inhibition (HAI) titer alone, to determine whether vaccination with the seasonal vaccine induced cross-reactive immunity to swH1N1 in some individuals, and to determine whether the immune response against swH1N1 is higher after infection than vaccination.
Methods
Antibody and T cell responses were studied in ten subjects who were first immunized with the 2009–2010 seasonal influenza subunit vaccine, then 6 weeks later with the swH1N1 monovalent subunit vaccine. The amount of antibody against native virus glycoproteins, overall avidity of these antibodies, and HAI titer were measured. T cells were evaluated for proliferation and IFNγ secretion in response to the vaccine in vitro. Individuals with influenza-like illness were also evaluated, adding a microplate neuraminidase inhibition (NAI) test.
Results
The immune response to influenza was highly variable and immune parameters did not increase in parallel. The seasonal vaccine induced antibodies recognizing the pandemic virus in 50% of subjects. Antibody affinity and NAI activity to swH1N1 were higher after natural infection than vaccination.
Conclusions
The evaluation of several immune parameters gives a more complete measure of immune responsiveness to influenza infection or vaccination than the HAI test alone.
Similar content being viewed by others
Introduction
In April 2009, a novel H1N1 influenza virus spread throughout the USA and Mexico and then to the world. Its origins remain unknown but sequence analysis of the genome revealed that the new human virus was a reassortant between two swine viruses. There are no data to indicate whether this reassorting event occurred in pigs, in people or in laboratory culture [1]. The new virus is variously called “pandemic,” “2009,” or “swine-origin” H1N1 (swH1N1).
The influenza type A genome consists of eight segments of single stranded, negative-sense RNA, each coding for one or two proteins using alternative splicing or alternative reading frames. When two different influenza A viruses infect a cell there can be a reassorting of the genome segments, and this is considered to be the origin of new pandemic viruses. Genes coding for the major surface antigens of an animal or bird virus can become incorporated into an otherwise human virus, producing a reassortant virus that replicates in humans but has hemagglutinin (HA) and sometimes neuraminidase (NA) antigens that are new to the human immune system. The 2009 swH1N1 virus has a different origin. All of its genes are derived from swine influenza viruses; the NA and matrix genes are from the Eurasian swine virus lineage while the remainder are from a “US triple reassortant” virus [2, 3]. Although the HA of the new virus diverged from classical swine H1N1 HA around 1998, there is still considerable similarity with classical swine HA (such as the A/New Jersey/76 strain) [2, 4] and also with older human HAs as has been noted in comparing antigenic properties [5]. Not surprisingly, older people were found to have more anti-swH1N1 antibodies than younger cohorts in samples taken before the pandemic, but the age cut-off defining “young” vs. “older” subjects varies widely in different reports, making it difficult to compare them [4, 6–8]. At least one study found that anti-swH1N1 antibodies were higher in people who had been vaccinated in 1976 with the swine influenza vaccine [9].
CDC estimated that approximately 60,000,000 people in the USA were infected by swH1N1 in the first year of circulation. The disease caused by this virus is usually mild, but the virus was more commonly isolated from younger people than the elderly population that is usually at risk for complications from influenza infection, and pregnant women were found to be among the more severe cases. Estimates of infection rates using serology varied with age and location, and children seroconverted at higher rates than older people [8, 10].
Curiously, the seasonal vaccine was reported to provide little or no protection against swH1N1 infection [4]. The lack of any cross-reactivity is an anomaly, given that the definition of the H1 subtype is that antibodies against one H1 HA will cross-react with other H1 HAs. There is also wide diversity in results from one study to another. It is well recognized that the hemagglutinin inhibition (HAI) assay used to measure seroconversion is no longer a reliable indicator of vaccine responsiveness or recent infection, partly because high levels of preexisting antibodies suppress further increase in the HAI titer, and partly because of inherent large errors in the method, which measures an end point from 2-fold dilutions. In recent years HAI results have been confounded by varying specificity and affinity of receptor binding [11, 12]. Each virus of interest can be tested with several species of red blood cells, but even after optimizing the red cell species, the results are highly variable [13]. The goal of our study was 3-fold: (1) to determine whether multiple and/or alternative B cell and T cell parameters are more reliable than HAI alone in assessing immune responses to vaccination and infection, (2) to look for evidence of cross-reactive antibodies to swH1N1 as a result of immunization with the seasonal vaccine, and (3) to compare the magnitude of immune responses to vaccination vs. infection. We applied our Native ELISA method [14], [15], HAI, and a new microplate format NA inhibition (NAI) assay to investigate induction of antibodies, along with T cell proliferation and IFNγ production to measure T cell responses, in two sets of subjects: (a) those who were vaccinated first with seasonal trivalent subunit influenza vaccine (2009–2010 formulation) and secondly with monovalent swH1N1 vaccine and (b) those who suffered an influenza-like illness during the pandemic in Oklahoma City in summer/fall of 2009. The results show that individuals vary in whether they respond with increased amount and/or affinity of antibodies and whether the increase is accompanied by robust T cell activity. Thus, multiple parameters are needed to assess the immune response to infection or vaccination. Half of the subjects showed an increase in antibodies that cross-reacted to swH1N1 after seasonal vaccination. Antibody affinity and NAI activity were higher after natural infection than after vaccination.
Materials and Methods
Viruses, Vaccines, and Cells
The swH1N1 virus used in this study was a clinical isolate A/Oklahoma/3052/2009 (similar to A/California/7/2009) that was grown in MDCK cells or in embryonated chicken eggs and purified by sucrose gradient centrifugation [11]. Other influenza viruses used were the 2009–2010 vaccine strains A/Uruguay/716/07 X-175C (H3N2) and A/Brisbane/59/2007 IVR-148 (seasonal H1N1), both grown in eggs. The vaccines used were seasonal 2009–2010 Afluria (CSL) and swH1N1 monovalent (Novartis).
Subjects
Ten healthy female subjects between the ages of 26 and 63 who received the seasonal subunit trivalent influenza vaccine during the fall of 2009 as part of an ongoing NIH-funded study were recruited to receive the monovalent swH1N1 vaccine approximately 6 weeks later. Ethical approval for the study was obtained from the Institutional Review Boards of the Oklahoma Medical Research Foundation and University of Oklahoma Health Sciences Center before the initiation of the study. Informed consent was obtained from each participant in accord with the Declaration of Helsinki. Blood was drawn on the day of vaccinations and 2 weeks after. Plasma was collected for antibody studies and peripheral blood mononuclear cells (PBMCs) were isolated for T cell functional assays.
ELISA and HAI
Antibodies against native conformations of surface proteins were measured by the “native ELISA” capture assay [15] using whole virus particles bound to turkey red cell membranes. The results were calculated using Prism software as Bmax, the amount of antibody (the units are absorbance normalized to a standard serum run with each group of sera), and Kd (apparent), which we converted to the reciprocal Ka, the overall avidity of antibodies in each serum sample. HAI titers were performed by standard procedures using turkey red blood cells after periodate treatment of the plasma samples which results in a 1:10 initial dilution [16, 17]. Results with human red blood cells were the same as with turkey red cells, but the end points were a little clearer with turkey cells.
Neuraminidase Inhibition Test
We adapted the Warren assay [18] to a 96-well plate format by using protease digestion of fetuin and reduced salt concentrations to eliminate the need for an extraction step. Plasma samples were inactivated at 56°C for 30 min and diluted 1:10 before use. Fetuin was digested with proteinase K (1:20 proteinase K/fetuin w/w) at 50° for 2 h, then inactivated at 100°C for 10 min and quick-chilled on ice. Any precipitate was removed by centrifugation. Twenty-five microliters of serum in 2-fold dilutions was added to a row of wells followed by 25 μl of virus that had been diluted to an NA activity in the linear range. After 1 h at room temperature to allow binding of antibodies to virus, we added 25 μl of proteinase K digested fetuin (40 mg/ml). The plate was covered and incubated at 37°C for 1–2 h. Periodate (25 μl 0.08 M sodium periodate in 25% orthophosphoric acid) was added to each well and the plate incubated at room temperature for 20 min. Sodium arsenite (50 μl of 0.77 M, pH 9.0) and thiobarb reagent (100 μl, 0.042 M 2-thiobarbituric acid) were added and the plate heated at 85°C for 20 min to develop the color. Fifty microliters of DMSO was added to each well to enhance and stabilize the color. The plate was centrifuged to pellet any precipitate and 150 μl supernatant transferred to a new plate for reading at 549 nm. Results were calculated as EC50 using Prism software.
Cell Isolation
PBMCs were isolated from freshly drawn blood anti-coagulated with ACD by Ficoll-Hypaque density gradient centrifugation. The cells were washed twice, counted, and resuspended in RPMI 1640 + 10% FBS (Hyclone) supplemented with 2 mM glutamine, penicillin (100 U/ml), and streptomycin (100 μg/ml).
IFNγ ELISPOT
PBMCs were cultured in 0.2 ml volumes in 96-well IFNγ ELISPOT plates (Becton Dickinson) in medium alone or with PHA at 2.5 μg/ml, the seasonal influenza vaccine at 0.6 and 0.2 μg/ml, the swH1N1 vaccine at 0.2 and 0.067 μg/ml, or purified Brisbane H1N1 or swH1N1 at 1.25 or 0.5 μg/ml for 18 h. The cell density was 5 × 105/ml for the control and PHA cultures and 2 × 106/ml for the vaccine and viral cultures. At the end of the cultures, the cells were removed from the wells and the plate was developed to reveal the number of IFNγ-secreting PBMCs according to the manufacturer’s instructions. The spots were counted with an ImmunoSpot (Cellular Technology, Ltd.). Data from the concentration of vaccine or virus giving the best results were used in the analyses.
T Cell Proliferation Assays
PBMCs were labeled with carboxyfluorescein succinimidyl ester (CFSE), washed twice, and then cultured at 106 cells/ml in 0.5 ml volumes in 48-well plates in medium alone, PHA at 1.25 or 0.625 μg/ml, the seasonal influenza vaccine at 0.05 or 0.025 μg/ml, the swH1N1 vaccine at 0.015 or 0.0075 μg/ml, or purified Brisbane H1N1 or swH1N1 at 0.22 or 0.075 μg/ml for 6 days at 37°C and 5% CO2. At the end of the culture period, the cells were stained with APC anti-CD4 and the percentage of CD4+ cells that had undergone cell division (as assessed by CFSE dye dilution) was determined with a FACSCalibur (Becton Dickinson) and FlowJo software (TreeStar). Data from the concentration of vaccine or virus giving the best results were used in the analyses.
Results
Vaccine Responses
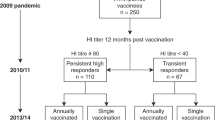
Our study design involved ten subjects who were first immunized with the 2009–2010 seasonal trivalent influenza subunit vaccine, then with the swH1N1 subunit vaccine approximately 6 weeks later. Four blood samples were obtained: (1) on the day of seasonal vaccine administration, (2) 2 weeks later, (3) on the day of swH1N1 vaccine administration, and (4) 2 weeks after swH1N1 vaccination. Each plasma sample was assayed for three antibody parameters; amount of antibody against native virus particles (Bmax), overall avidity of these antibodies (Ka), and hemagglutination inhibition titer (HAI). Response was measured against three viruses; the H3N2 and seasonal H1N1 components of the 2009–2010 vaccine and A/Oklahoma/3052/2009, a 2009 swH1N1 isolate. The only difference in HA1 amino acid sequence of 3052 compared to the vaccine strain A/California/7/2009 is K157T, numbered according to Caton et al. [19]. T cell responses were assessed by IFNγ secretion measured by ELISPOT and T cell proliferation measured by CFSE dye dilution after in vitro stimulation with seasonal or swH1N1 vaccines and viruses. Stimulation with PHA was used as a positive control (data not shown).
Individual Antibody Responses Show Considerable Variation from Subject to Subject
Our ten subjects each showed a unique profile of antibody responses (Supplemental Fig. 1), reflecting their past exposure to influenza infection and/or vaccine as well as their immunogenetic makeup. As we have found in other studies [14, 15], Bmax, Ka and HAI did not increase in concert. The fold increases and final levels achieved against H3N2, H1N1, and swH1N1 are shown in Table I. Two and five of ten subjects showed a ≥1.5-fold increase against the seasonal H3N2 and H1N1, respectively, in at least two parameters. In contrast, the antibody response against the swH1N1 was more robust, with nine of ten subjects showing a ≥1.5-fold increase in at least two parameters. The exception was subject 102 who had a 1.5-fold increase in HAI against swH1N1 and who also showed very little response to either seasonal H1N1 or H3N2 vaccine components. The final levels of Bmax, Ka, and HAI for that subject are among the lowest against all three viruses tested.
All ten subjects showed a ≥1.5-fold increase in HAI against swH1N1 after vaccination. In three subjects (010, 113, and 102), this increase was induced after seasonal vaccine rather than after the swH1N1 vaccine; i.e., antibodies induced were cross-reactive between seasonal and swH1N1 (see Supplemental Fig. 1). Nine of ten subjects also showed a ≥1.5-fold increase in Ka (seven subjects) and/or Bmax (five subjects) against the swH1N1. All subjects except 082 achieved an HAI titer >40 against swH1N1. Thus, when considering the individual responses, one can conclude that there was a more robust response to the swH1N1 than to the seasonal vaccine. This might be expected as the swH1N1 vaccine contained a virus that was new to the population, and in most cases, the pre-vaccination levels against swH1N1 were lower than for H3N2 or H1N1.
The 2009–2010 Seasonal Vaccine-Induced Antibodies that Cross-React with 2009 swH1N1
The average results of Bmax, Ka, and HAI for the ten subjects are shown in Fig. 1a. After seasonal vaccination, there was an increase in Bmax that was significant for H3N2 using a paired t test (p = 0.01) but not for seasonal H1N1 (p = 0.07). Conversely, both Ka and HAI showed significant increases for seasonal H1N1 (p = 0.047 and 0.03, respectively) but not for H3N2 (p = 0.095 and 0.43, respectively). After vaccination with 2009 swH1N1, there was a significant increase in Ka against the homologous virus (p = 0.021) but not in HAI (p = 0.085), or Bmax (p = 0.39). Interestingly, Bmax for swH1N1 increased significantly after seasonal vaccination (p = 0.016), demonstrating cross-reactivity between the seasonal and swH1N1 viruses. Bmax for swH1N1 did not increase further after swH1N1 vaccination. Neither Ka nor HAI for swH1N1 showed significant increases after the seasonal vaccination (p = 0.29 and 0.12, respectively). However, there was a significant increase in HAI for swH1N1 (p = 0.007) if one compares the titer before either vaccination with that after swH1N1 vaccination. It can be noted in Fig. 1a that the baseline levels of antibodies against the swine-origin H1N1 virus are well above background, which also suggests cross-reactivity between antibodies against the seasonal and swine-origin H1N1 viruses. Previously we have found a clear inverse correlation between preexisting antibodies and fold increase after vaccination [14, 15] and that inverse correlation is seen for all three viruses tested (Fig. 1b). Although this study focused on the diversity of individual responses, there are statistically significant increases in average values for some parameters after immunization and each of the three vaccine components elicited an increase in at least one parameter.
Antibody responses to seasonal and 2009 swH1N1 vaccination. All subjects were immunized with the 2009–2010 seasonal trivalent subunit influenza vaccine and with the swH1N1 vaccine approximately 6 weeks later. Blood samples were obtained on the days of vaccination and 2 weeks after each vaccination. a. Bmax, Ka, and HAI were measured against the seasonal H3N2 and H1N1 vaccine strain viruses and against A/Oklahoma/3052/2009, a swH1N1 strain, as described in the “Materials and Methods” section. The units for Bmax are absorbances normalized to a standard plasma run with each group of plasmas. The units for Ka are μl−1 plasma in 50 μl. For HAI, the results are plotted as the number of wells of 2-fold serum dilutions starting at 1:10 that are inhibited (three wells is a titer of 40, usually considered as protective); this is used so that the range is comparable to those of the other parameters. p values are for pre- and post-vaccination values compared using a paired t test. b The fold increase in post-vaccination anti-influenza antibody concentration is inversely related to the pre-vaccination levels. The fold increase in Bmax post-vaccination (blood draw #4) is plotted against the pre-vaccination Bmax levels (blood draw #1) for the seasonal H3N2 (Uruguay), seasonal H1N1 (Brisbane), and swH1N1
Individual T Cell Responses Show Considerable Variation from Subject to Subject
The T cell responses to immunization with the seasonal and swH1N1 vaccines were also highly variable from subject to subject (Supplemental Fig. 1). The fold increases and final levels achieved are shown in Table II. Five of nine subjects from whom complete data were available made a ≥1.5-fold greater IFNγ ELISPOT response to swH1N1 vaccination, but only three of ten did so after seasonal vaccination. Only two subjects made a ≥1.5-fold greater response to both vaccines. Three of nine subjects with complete data made a ≥1.5-fold greater proliferative response to the seasonal vaccine, but only one of seven did so after swH1N1 vaccination. Thus, not only were individual responses highly variable, but the results of the two types of T cell assays were not concordant.
T Cell Responses to the 2009–2010 Seasonal Influenza Vaccine Were Inversely Proportional to the Level of Pre-Vaccination T Cell Immunity
We failed to see significant increases in IFNγ production by ELISPOT (Fig. 2a) to the seasonal vaccine (p = 0.47), the swH1N1 vaccine (p = 0.085), or to the purified seasonal H1N1 (p = 0.19) and swH1N1 vaccine viruses (p = 0.20). As expected, the average response to the swH1N1 vaccine was about one third of that to the seasonal vaccine, as it contained only one virus instead of three. As was seen with the antibody responses, there was an inverse relationship between the pre-vaccination ELISPOT values and the fold increase post-vaccination (Fig. 2b). For the proliferative response, there was no significant increase against the seasonal vaccine (p = 0.32) but after swH1N1 vaccination there were significant increases in the proliferative response to the swH1N1 vaccine (p = 0.027) and the swH1N1 virus (p = 0.00076), but not to seasonal H1N1 virus (p = 0.10). The average proliferative response to the swH1N1 vaccine was only about 20% of that to the seasonal vaccine, even lower than expected based on having only one virus instead of three. Again, an inverse relationship between the pre-vaccination proliferative response and the fold increase post-vaccination was observed (Fig. 2d).
T cell responses to seasonal and 2009 swH1N1 influenza vaccination. All subjects were immunized with the 2009–2010 seasonal trivalent subunit influenza vaccine and with the swH1N1 vaccine approximately 6 weeks later. Blood samples were obtained on the days of vaccination and 2 weeks after each vaccination. a IFNγ ELISPOT responses were measured after culturing PBMCs in vitro with either the vaccines or purified seasonal H1N1 (Brisbane) or swH1N1. p values are for pre- and post-vaccination values compared using a paired t test. b The fold increase in post-vaccination IFNγ ELISPOT is inversely related to the pre-vaccination levels. The fold increase in post-vaccination IFNγ ELISPOT in response to in vitro culture with the seasonal or swH1N1 influenza vaccine is plotted against the pre-vaccination levels. c CD4 T cell responses were measured by CFSE dye dilution after culturing PBMCs in vitro with either the vaccines or purified seasonal H1N1 (Brisbane) or swH1N1. p values are for pre- and post-vaccination values compared using a paired t test. d The fold increase in post-vaccination CD4 T cell proliferative response is inversely related to the pre-vaccination levels. The fold increase in post-vaccination CD4 T cell proliferation in response to in vitro culture with the seasonal or swH1N1 influenza vaccine is plotted against the pre-vaccination levels
Study of Patients with Influenza-Like Illness and Controls
To determine if human immune responses to infection with swH1N1 are larger and more uniform than those following vaccination, we tested convalescent plasma samples from nine subjects who reported influenza-like illness (ILI) during the swH1N1 epidemic in Oklahoma City and two who did not, adding a new 96-well NAI test to the measures of response. We have previously shown that the NA content of seasonal vaccines is variable but always low [15], and there is insufficient NA in most seasonal influenza vaccines to elicit a consistent NAI response except in high-dose formulations [20]. The NAI results are reported as IC50 (volume of plasma that gives 50% reduction of NA activity), so lower numbers represent higher activity. Selected subjects were evaluated for their T cell responses to either the vaccine or virus using an IFNγ ELISPOT assay and a CD4 T cell proliferation assay based on CFSE dye dilution as described above. Only one of our subjects with ILI had PCR-confirmed swH1N1 infection (#202), so we used our multi-parameter evaluation of the immune response to influenza to draw conclusions about which of our ILI subjects had been infected with swH1N1.
Antibody Responses to swH1N1 Infection Were Highly Variable from Subject to Subject
Everybody in our study has their own antibody response profile. As in the vaccination study, we examined each individual’s response using multiple parameters. The results are shown in Fig. 3. The fold differences for the five subjects with two time points as well as the convalescent values for all 11 subjects are shown in Table III. As in the vaccination study, the antibody parameters did not change in concert. For the five subjects with two time points, all showed a ≥1.5 improvement in Ka but only two showed improved HAI, one improved NAI, and one increased Bmax. However, we also know that if a parameter is already high, it tends not to increase after vaccination [14, 15], and the same appears to be true for infection. Subjects 203 and 105 had high Bmax at the first blood draw and showed less than 10% increase, while subjects with lower initial Bmax showed significant increase, except for 202. This subject, the only one confirmed to have swH1N1 by PCR, showed >1.5 increase in HAI and Ka and a decrease (improvement) of 1.25 in NAI. Subject 105 had changes >1.5 in Ka, HAI, and NAI, subject 404 improved in Bmax and Ka. Subject 019 showed >1.5-fold change only in Ka although Bmax and HAI increased slightly. This person had high levels of Bmax and HAI and low NAI at the first blood draw, so further increases in these parameters were unlikely (see Fig 1b). The most difficult subject to interpret was 203. This person, who recalled receiving the swine flu vaccine in 1976, had a high initial Bmax, a low NAI and an initial HAI of 40. There was a 1.5-fold increase in Ka between 1 and 6 weeks, but the Ka remained low. She therefore showed preexisting immunity but was probably not infected with swH1N1. A less likely possibility is that she was infected but the preexisting immunity precluded an improvement in Bmax, HAI, or NAI so that the only change was a modest increase in affinity of antibodies (see text below).
Antibody and T cell responses in subjects with influenza-like illness or control subjects. Antibody and T cell responses to A/Oklahoma/3052/2009 were assessed 4–9 days after the onset of illness and approximately 6 weeks later (except for 105 for whom an archived plasma sample was available and 404 who was studied on days 4 and 8 after the onset of symptoms). The gray areas indicate values expected in healthy subjects as a result of previous vaccinations or influenza exposures, but independent of recent swH1N1 infection. The units are the same as in Figs. 1 and 2
For the subjects with only one time point, including two controls who reported no ILI, we assessed the likelihood of swH1N1 infection by comparing the level of each parameter to a “threshold” value that we considered equivalent to background in a population that is likely to have been previously exposed to some influenza antigens. Values higher (or lower in the case of NAI) than the threshold values shown in Fig. 3 were taken as an indication of a recent influenza infection. Only one of these subjects (002) was high in Bmax, Ka, and HAI and low (good) in NAI, leading to the conclusion that this person had likely been infected with swH1N1 (Table IV). Two others were high in Bmax but the affinities were low, as might be expected for antibodies cross-reactive with seasonal H1N1. One additional person (106) had an HAI titer above the threshold value. This person reported no illness but had received the 1976 swine flu vaccine. By combining all the results from the antibody studies, we were able to draw the conclusion that subjects 202, 105, 019, 404, and 002 had most likely been infected with the swH1N1 virus (Table IV). If one compares the average values for Bmax, Ka, HAI, and NAI between those subjects we assign to the infected vs. not infected groups (Table III), there is a statistically significant difference in the Ka and NAI values and it is evident that the convalescent immune parameters for subject 203 are most consistent with not having had recent swH1N1 infection.
T Cell Responses to Whole Influenza Virus In Vitro Can Be Large, but Are Not Necessarily Informative About Recent Exposure to a Particular Virus
Analysis of T cell responses to the swH1N1 virus among subjects who reported an ILI during the swine flu epidemic in Oklahoma City was incomplete due to the logistical complications of performing in vitro assays on live cells on subjects who were ill (compared to measuring antibodies in stored plasma samples). Nevertheless, we were able study subjects 202 and 203 at two time points and several other subjects at a single time point (Fig. 3). Two interesting observations were made. First, subject 202 who had PCR-confirmed swH1N1 infection had an IFNγ ELISPOT response that was clearly higher than what is normally seen with vaccination. Secondly, even individuals who have never been vaccinated and did not experience ILI (subject 009) can still make significant T cell responses, most likely because of previous exposure to influenza viruses that did not result in clinical illness.
Immune Parameters of Subjects Who Were in Both Trials
Two subjects were in both the infection and vaccination studies, and show contrasting profiles that are instructive for both vaccine and infection statuses. Subject 009 reported never having flu or flu vaccine and was a negative control for the infection study. Prior to vaccination, this person had amongst the lowest Bmax, HAI, and Ka for all three viruses (H3N2, H1N1, swH1N1) of all ten subjects. Even so, her HAI was >40 against H3N2 (Supplemental Fig. 1, first time point) and in the infection study, she also had high T cell responses (Fig. 3), perhaps indicating a recent subclinical influenza infection. After seasonal vaccination, there were significant increases in BmaxH3N2, H1N1, swH1N1, KaH1N1, HAIH1N1, swH1N1, and IFNγ ELISPOT. After swH1N1 vaccination, there were significant increases in KaswH1N1, HAIswH1N1, and IFNγ ELISPOT. There was induction of swH1N1 cross-reactive antibodies after seasonal vaccination (Supplemental Fig. 1), boosted by the swH1N1 vaccine. This person now has good immunity in all antibody parameters against all viruses except KaH3N2. This excellent response to a single vaccination also suggests a previous subclinical exposure. We predicted that another H3N2 vaccination would improve KaH3N2, and in fall of 2010 KaH3N2 increased more than 10-fold after this subject received the trivalent 2010–2011 vaccine (data not shown).
Subject 082 has been frequently vaccinated and reported ILI in 2009. This person had good pre-vaccination BmaxH3N2,H1N1 and good HAIH3N2. Pre-vaccination swH1N1 antibody was quite high in Bmax but low in Ka and HAI, while ELISPOT and proliferation were borderline. We concluded this person did not have influenza in 2009, and indeed the rapid test for influenza A was negative at the time of illness. After seasonal vaccination, KaH3N2, H1N1 and HAIH3N2, H1N1 had significant increase, as did IFNγ ELISPOT. After swH1N1 vaccination, KaswH1N1 and HAIswH1N1 showed significant increase. Despite frequent vaccination, KaH3N2, H1N1 was low but improved after new seasonal vaccination. This person showed little cross-reactivity of seasonal H1N1 antibodies with swH1N1 (Supplemental Fig. 1)—the latter increased after swH1N1 vaccine. We predict this person will improve antibodies against swH1N1 when next vaccinated. These results illustrate that detailed analysis of different parameters allow assessment of a subject’s immune history and immune response.
Discussion
We undertook this study to address three goals: (1) to assess whether analyzing multiple parameters of immune responses to influenza vaccination and infection in people with varying histories of vaccination or infection has an advantage over evaluating HAI alone, (2) to determine if vaccination with the seasonal trivalent influenza vaccine induced cross-reactive immunity to swH1N1, and (3) to determine if the immune response against swH1N1 is higher after infection than after vaccination. Our subjects have variable histories of exposure to influenza infection or vaccination. The ubiquitous “influenza-like illness” may not result in a clinic visit or be followed up with virus identification, so the exact virus exposure of our subjects (or most of anyone’s subjects) cannot be known with certainty.
-
1.
Does Analysis of Multiple Immune Parameters Have an Advantage over HAI Alone?
The subjects in our study showed highly individual antibody and T cell responses, reflecting their previous vaccination or infection history as well as genetic and environmental differences. Responses to H1N1 and H3N2 components in the seasonal vaccine did not mirror each other (Supplemental Fig. 1). Although a vaccination should lead to exposure to the same amount of antigen from each of the three vaccine viruses, some subjects may have also been exposed to H1N1 or H3N2 viruses giving a differential memory pool. In addition, differences in responses to H3N2 versus seasonal H1N1 may be due to different antigen stabilities after vaccination, vaccine manufacturing processes, or to inherent sensitivity to one antigen over another in individual subjects. The inverse correlation between pre-vaccination levels of antibody and fold increase after vaccination seen in our previous studies [14, 15, 21] is recapitulated in this study (Fig. 1b), and also extends to T cell parameters (Figs. 2b, d). Thus, it can be misleading to conclude that an immune response to either vaccination or infection has not occurred based on a small or absent fold increase in Bmax, for example. In some subjects, the higher increase is in Ka and/or HAI. Conversely, a high Bmax, HAI, or IFNγ ELISPOT may be indicative of previous exposure to either virus or vaccine and does not necessarily indicate a response to a recent infection or vaccination unless it has increased from a baseline value or is accompanied by improvement in another parameter such as Ka. The results of this study clearly show that an increase in a single parameter, such as HAI, is not sufficient to assess a person’s immune response to infection, as only 2 out of 5 of the individuals for whom we had two time points showed ≥1.5-fold increase in HAI. In contrast, all 5 of these subjects showed ≥1.5-fold increase in Ka.
Baseline samples are not usually available in the case of influenza infection, so a different strategy is needed to evaluate whether or not a person has been infected. For HAI, a titer of ≥40 is generally accepted as evidence of good immunity to influenza, but there are no analogous values for Bmax, Ka or NAI. Therefore, to assess the likelihood of recent infection, we compared the values for each immune parameter with “threshold” values typical for healthy individuals with prior exposure to influenza viruses or vaccines based on our experience during a five year NIH-funded contract to evaluate immune responses to influenza vaccination. By combining the results from assays evaluating multiple immune parameters, one can make a reasonable judgment as to whether a given individual has been recently infected (Table IV).
-
2.
Cross-Reactivity Between Seasonal H1N1 and swH1N1
There are a number of reports in the literature, some conflicting, addressing the question of cross-reactivity between seasonal H1N1 and pandemic swH1N1. In sera stored before the emergence of swH1N1, there is little evidence of cross-reactive antibodies in children, but significant levels in people over the age of ∼60 [4], [22], [23]. People over the age of 55 who had received the 1976 vaccine showed higher neutralizing titers against the swH1N1 than those of similar age who had not, although the HAI titers were similar against seasonal and swH1N1 [9]. There is considerable antigenic and sequence similarity between classical swine viruses, such as A/New Jersey/76, the new pandemic virus, and the 1918 viruses. Indeed, the epitope of 1918 HA for antibody 2D1 that has been well characterized by X-ray crystallography of an antibody–HA complex is the same in the 2009 pandemic HA [5]. Examination of sequence alignments shows that the 2D1 epitope is largely mutated from PR/8/34 onwards in seasonal H1N1 viruses, but is preserved in New Jersey/76 and the pandemic swH1N1 viruses. For T cells, most individuals have abundant CD4 T cells that recognize cells infected with swH1N1, either from prior infection or from vaccination [24], and preexisting T cell memory for swH1N1 is of the same magnitude as for seasonal H1N1 [25]. The age range of our vaccine study group was 26–63 years and only the oldest person (102, age 63) showed a protective HAI before vaccination (HAI of three wells in Supplemental Fig. 1 corresponds to a titer of 40). As this subject did not receive the swine flu vaccine in 1976, she likely encountered the 2009 virus itself, or less likely, a swine H1N1 virus. It has been shown that people vaccinated with the A/New Jersey strain in 1976 have good cross-reactivity with swH1N1 [4]. There is evidence from serum samples stored before and after the pandemic of a significant level of subclinical infection with swH1N1 in multiple locations during 2009, with higher seroconversion rates in the young, who rarely showed preexisting antibodies against swH1N1, than in older people. The infection rate estimates are 20–30% over worldwide sites [6, 8, 10].
Studies in ferrets showed that the seasonal influenza vaccine did not induce functional antibodies against swH1N1 but did provide priming that allowed a rapid induction of protective antibodies after swH1N1 vaccination [26]. A/New Jersey/76 infection provided complete protection of ferrets against swH1N1 disease; there was an increase in antibody titers indicating a subclinical infection occurred [27]. Infection with seasonal H1N1, and to a lesser extent vaccination, lessened illness when ferrets were challenged with swH1N1, also likely to be due to priming [26, 28].
We saw clear cross-reactivity between swH1N1 and seasonal H1N1 in the several subjects who improved titers against swH1N1 after receiving seasonal trivalent vaccine (Supplemental Fig. 1). Considering a ≥1.5-fold change as meaningful, four of the ten subjects improved Bmax for swH1N1, six improved Ka and nine improved HAI. Priming in these cases was probably due to previous exposures to seasonal H1N1 and perhaps a more diverse memory bank than was seen in the naïve ferret experiments. These results are in accord with the several studies that show excellent response of humans to a single dose of swH1N1 vaccine [29, 30], suggesting that the “new” antigen was not totally new. Trials of H5N1 vaccine have shown poor responses, as might be expected for an antigen that is definitely new [31, 32].
As the swH1N1 vaccine was not available at the time our subjects were immunized with the seasonal influenza vaccine, and we did all of our T cell functional assays on freshly isolated cells, we were unable to assess whether immunization with the seasonal vaccine improved T cell responses to the swH1N1 vaccine. However, we did observe that T cell responses to whole swH1N1 virus were larger than to the vaccine, suggesting that exposure to even distantly related H1N1 viruses will provide some protection to a new virus, likely because the internal proteins are highly conserved.
-
3.
Comparison of Immune Responses to Influenza Vaccination vs. Infection
Overall, the magnitude of the humoral immune response to swH1N1 vaccination and swH1N1 infection as assessed by Bmax and HAI was similar in our subjects. Thus, we conclude that these aspects of the humoral immune response to influenza are predicated more on an individual’s previous exposure history and genetic and environmental influences than whether the boosting stimulus was vaccine or infection. However, the average final Ka was about 3-fold higher in the swH1N1 patients compared to the vaccinees, suggesting that higher affinity antibodies are generated after infection than vaccination. As expected, there was little response to NA after vaccination, as the amount of NA in vaccines is low. However, NAI activity was easily measured in all of our subjects with swN1H1 infection, suggesting that this is a useful second measure of virus exposure.
Although we had limited T cell data on subjects with swH1N1 infection, one subject (202) had an IFNγ ELISPOT response to whole virus that was >5-fold higher than the average response of our ten subjects to the swH1N1 vaccine. This result is probably because the T cell response to the vaccine is focused upon HA, while that to the whole virus includes responses to internal proteins.
In summary, although assessment of a single parameter (usually HAI) averaged over the whole population is an accepted measure of overall efficacy of an influenza vaccine before it can be licensed, valuable mechanistic information is lost when the results from hundreds of people are averaged. For this reason, our experiments used small numbers of subjects, each examined in detail for their antibody amount, antibody affinity, HAI, T cell function and, where appropriate, NAI, before and after vaccination or after infection. The highly individual response patterns can be deconvoluted by assessing multiple antibody and T cell parameters to identify those who have been infected with swH1N1 and to evaluate the vaccine response in a primed population.
Abbreviations
- APC:
-
Allophycocyanin
- CFSE:
-
Carboxyfluorescein succinimidyl ester
- HA:
-
Hemagglutinin
- ILI:
-
Influenza-like illness
- NA:
-
Neuraminidase
- swH1N1:
-
Swine-origin 2009 pandemic H1N1 human influenza virus
References
Gibbs AJ, Armstrong JS, Downie JC. From where did the 2009 ‘swine-origin’ influenza A virus (H1N1) emerge? Virol J. 2009;6:e207.
Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201.
Smith GJD, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–5.
Hancock K, Veguilla V, Lu X, Zhong W, Butler EN, Sun H, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009;361:1945–52.
Xu R, Ekiert DC, Krause JC, Hai R, Crowe JE, Wilson IA. Structural basis of preexisting immunity to the 2009 H1N1 pandemic influenza virus. Science. 2010;328:357–60.
Gilbert GL, Cretikos MA, Hueston L, Doukas G, O'Toole B, Dwyer DE. Influenza A (H1N1) 2009 antibodies in residents of New South Wales, Australia, after the first pandemic wave in the 2009 southern hemisphere winter. PLoS ONE. 2010;5:e12562.
Ikonen N, Strengell M, Kinnunen L, Osterlund P, Pirhonen J, Broman M, et al. High frequency of cross-reacting antibodies against 2009 pandemic influenza A(H1N1) virus among the elderly in Finland. Euro Surveill. 2010;15(5):pii=19478.
Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010;375:1100–8.
McCullers JA, Van De Velde L-A, Allison KJ, Branum KC, Webby RJ, Flynn PM. Recipients of vaccine against the 1976 “swine flu” have enhanced neutralization responses to the 2009 novel H1N1 influenza virus. Clin Infect Dis. 2010;50:1487–92.
Zimmer SM, Crevar CJ, Carter DM, Stark JH, Giles BM, Zimmerman RK, et al. Seroprevalence following the second wave of Pandemic 2009 H1N1 influenza in Pittsburgh, PA, USA. PLoS ONE. 2010;5:e11601.
Kumari K, Gulati S, Smith DF, Gulati U, Cummings RD, Air GM. Receptor binding specificity of recent human H3N2 influenza viruses. Virol J. 2007;4:42.
Gulati S, Smith DF, Air GM. Deletions of neuraminidase and resistance to oseltamivir may be a consequence of restricted receptor specificity in recent H3N2 influenza viruses. Virol J. 2009;6:22.
Subbarao EK, Kawaoka Y, Ryan-Poirier K, Clements ML, Murphy BR. Comparison of different approaches to measuring influenza A virus-specific hemagglutination inhibition antibodies in the presence of serum inhibitors. J Clin Microbiol. 1992;30:996–9.
Gulati U, Keitel WA, Air GM. Increased antibodies against unfolded viral antigens in the elderly after influenza vaccination. Influenza Other Respir Viruses. 2007;1:147–56.
Feng J, Gulati U, Zhang X, Keitel WA, Thompson DM, James JA, et al. Antibody quantity versus quality after influenza vaccination. Vaccine. 2009;27:6358–62.
Couch RB, Kasel J. Influenza. In: Lennette EH, Lennette DA, Lenette ET, editors. Diagnostic Procedures for Viral, Rickettsial and Chlamydial Infections. 7th ed. Washington, D.C.: American Public Health Association; 1995. p. 431–46.
Noah DL, Hill H, Hines D, White EL, Wolff MC. Qualification of the hemagglutination inhibition assay in support of pandemic influenza vaccine licensure. Clinical and vaccine immunology: CVI. 2009;16:558–66.
Aymard-Henry M, Coleman MT, Dowdle WR, Laver WG, Schild GC, Webster RG. Influenzavirus neuraminidase and neuraminidase-inhibition test procedures. Bull World Health Organ. 1973;48:199–202.
Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell. 1982;31:417–27.
Cate TR, Rayford Y, Niño D, Winokur P, Brady R, Belshe R, et al. A high dosage influenza vaccine induced significantly more neuraminidase antibody than standard vaccine among elderly subjects. Vaccine. 2010;28:2076–9.
Gulati U, Kumari K, Wu W, Keitel WA, Air GM. Amount and avidity of serum antibodies against native glycoproteins and denatured virus after repeated influenza whole-virus vaccination. Vaccine. 2005;23:1414–25.
Chi C-Y, Liu C-C, Lin C-C, Wang H-C, Cheng Y-T, Chang C-M, et al. Pre-existing antibody response against 2009 pandemic influenza H1N1 viruses in Taiwanese population. Clinical and vaccine immunology: CVI. 2010;17:1958–62.
Mak GC, Choy PWW, Lee WY, Wong AH, Ng KC, Lim W. Sero-immunity and serologic response to pandemic influenza A (H1N1) 2009 virus in Hong Kong. J Med Virol. 2010;82:1809–15.
Richards KA, Topham D, Chaves FA, Sant AJ. Cutting edge: CD4 T cells generated from encounter with seasonal influenza viruses and vaccines have broad protein specificity and can directly recognize naturally generated epitopes derived from the live pandemic H1N1 virus. J Immunol. 2010;185:4998–5002.
Greenbaum JA, Kotturi MF, Kim Y, Oseroff C, Vaughan K, Salimi N, et al. Pre-existing immunity against swine-origin H1N1 influenza viruses in the general human population. Proc Natl Acad Sci USA. 2009;106:20365–70.
Del Giudice G, Stittelaar KJ, van Amerongen G, Simon J, Osterhaus ADME, Stöhr K, et al. Seasonal influenza vaccine provides priming for A/H1N1 immunization. Sci Transl Med. 2009;1:12re1.
Min J-Y, Chen GL, Santos C, Lamirande EW, Matsuoka Y, Subbarao K. Classical swine H1N1 influenza viruses confer cross protection from swine-origin 2009 pandemic H1N1 influenza virus infection in mice and ferrets. Virology. 2010;408:128–33.
Ellebedy AH, Ducatez MF, Duan S, Stigger-Rosser E, Rubrum AM, Govorkova EA, et al. Impact of prior seasonal influenza vaccination and infection on pandemic A(H1N1) influenza virus replication in ferrets. Vaccine. 2010. doi:10.1016/j.vaccine.2010.08.067.
Greenberg ME, Lai MH, Hartel GF, Wichems CH, Gittleson C, Bennet J, et al. Response to a monovalent 2009 influenza A (H1N1) vaccine. N Engl J Med. 2009;361:2405–13.
Talaat KR, Greenberg ME, Lai MH, Hartel GF, Wichems CH, Rockman S, et al. A single dose of unadjuvanted novel 2009 H1N1 vaccine is immunogenic and well tolerated in young and elderly adults. J Infect Dis. 2010;202:1327–37.
Beigel JH, Voell J, Huang C-y, Burbelo PD, Lane HC. Safety and immunogenicity of multiple and higher doses of an inactivated influenza A/H5N1 vaccine. J Infect Dis. 2009;200:501–9.
Hayden FG, Howard WA, Palkonyay L, Kieny MP. Report of the 5th meeting on the evaluation of pandemic influenza prototype vaccines in clinical trials: World Health Organization, Geneva, Switzerland, 12–13 February 2009. Vaccine. 2009;27:4079–89.
Acknowledgments
The authors thank Ms. Stephanie McGee and Ms. Emily Griffith for the expert technical assistance. The authors also thank Virginia Roberts, LPN and Evan Vista, MD for the clinical recruiting and characterization. Virus growth and characterization were done by Mary Tappert and Shelly Gulati. This work was supported by NIH contract #HHSN266200500026C (N01-AI-50026; L.F.T.) and NIH grant AI50933 (G.M.A.).
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplemental Fig. 1
Individual antibody and T cell responses to immunization with the seasonal and swH1N1 influenza vaccines. All subjects were immunized with the 2009–2010 seasonal trivalent subunit influenza vaccine and with the swH1N1 vaccine approximately 6 weeks later. Blood samples were obtained on the days of vaccination (blood draws 1 and 3) and 2 weeks after each vaccination (blood draws 2 and 4). Antibody responses were evaluated by measuring Bmax, Ka, and HAI at each time point. T cell responses were assessed by measuring IFNγ production by ELISPOT and proliferation by CFSE dye dilution after culturing PBMCs in vitro with the vaccines. The blood draws are labeled “1, 2, 3, and 4” across the bottom of each panel and HAI is plotted as number of wells showing HA inhibition as in Fig. 1. (PPT 192 kb)
Rights and permissions
About this article
Cite this article
Air, G.M., Feng, J., Chen, T. et al. Individual Antibody and T Cell Responses to Vaccination and Infection with the 2009 Pandemic Swine-Origin H1N1 Influenza Virus. J Clin Immunol 31, 900–912 (2011). https://doi.org/10.1007/s10875-011-9563-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-011-9563-1