Abstract
Cambodian immigrants are over 25 times more likely to have evidence of chronic hepatitis B infection than the general US population. Carriers of HBV are over 100 times more likely to develop liver cancer than non-carriers. Liver cancer incidence is the second leading cancer for Cambodian men and the sixth for Cambodian women. Despite this, this underserved population has received very little attention from health disparities researchers. Culturally and linguistically appropriate interventions are necessary to increase hepatitis B knowledge, serologic testing, and vaccination among Cambodian Americans. Eight group interviews were held with Cambodian American men (48) and women (49). Focus group discussion revealed unanticipated information about sociocultural influences on participants’ understanding about hepatitis B transmission, disease course, and prevention and treatment informed by humoral theories underlying Khmer medicine, by biomedicine, and by migration experiences. Our findings reveal the value of qualitative exploration to providing cultural context to biomedical information—a formula for effective health promotion and practice.
Similar content being viewed by others
Introduction
Hepatitis B virus (HBV) infections account for the majority (about 80%) of liver cancer deaths in the Asian community [9, 40]. Avoidable mortality from HBV related liver disease has been noted as one of the most important health disparities experienced by Asian Americans [43] and the President’s Advisory Commission on Asian Americans recently made recommendations for decreasing these health disparities [41]. HBV is highly preventable through screening and vaccination, and manageable through lifestyle changes and medication [9, 23].
Despite the fact that Cambodian immigrants are over 25 times more likely to have evidence of chronic hepatitis B infection than the general US population and over ten times more likely to be diagnosed with liver cancer [37, 41], this underserved population has received very little attention from health disparities researchers [11]. Liver cancer incidence is the second leading cancer for Cambodian men (51.0/100,000, 7.5 times greater than male non Hispanic White (NHW) rate) and the sixth leading cancer for women (14.2/100,000, 5.3 times greater than the female NHW rate) [23]. Cambodian refugees make up 1.8% of the Asian population in the US, with the majority having resettled in California, Washington, Texas, Pennsylvania, and Massachusetts [23]. Census data from 2000 and Census estimates from 2005 indicate that at least 25,000 Cambodians live in metropolitan Seattle-Tacoma, the site of our study [34, 38].
Ninety-nine percent of Cambodian Americans came to the US as refugees or immigrants over the last three decades, or are children of these immigrants [34]. The majority of Cambodians traveled to the US from Thai refugee camps where they spent from 1 to 10 years, enduring severe hunger and hardship, following the Khmer Rouge genocide (1975–1979) [3, 25]. Twenty percent of the population (1.5 million out of 8 million) was killed during the Khmer Rouge regime. Those who survived witnessed the deaths of their family members and loved ones and were subjected to starvation, exhaustion, relocation, forced labor, and “re-education” [7, 24]. This history of suffering has impacted reception of Cambodians into the US and their often troubling integration into the US medical system [33, 35, 39]. Understanding of this history, and its continuing relevance to daily lives and experiences of health and illness is an essential part of community-based health programs and culturally appropriate interventions focused on Cambodian-Americans [13, 16, 28, 29].
In the following, we report findings from the qualitative phase of a community-based participatory research (CBPR) study of hepatitis B in the Cambodian community in the Seattle-Tacoma metropolitan area of Washington State. The overall goal of our study was to contribute to the prevention of hepatitis B induced liver disease among Cambodian Americans. The specific objective of our study was to conduct a randomized controlled trial to evaluate the effectiveness of a culturally and linguistically appropriate lay health worker outreach intervention in improving levels of hepatitis B testing. The qualitative phase, reported here, was designed to identify unanticipated concerns and understandings about hepatitis B illness, testing, and vaccination. These data inform the design of quantitative surveys, lay health worker outreach plan, and educational materials used in the intervention.
While debates continue about what constitutes CBPR, there is basic agreement that CBPR in public health involves a systematic inquiry, with the collaboration of those affected by the health issue being studied, for the purposes of providing education or effecting change [12]. Israel has defined CBPR as a partnership approach to research that recognizes community members, organizational representatives, and researchers in all aspects of the process [18, 19]. Our study builds on over 10 years of research and health education collaboration between Harborview Medical Center, Fred Hutchison Cancer Research Center, and Seattle’s Cambodian Community. This community coalesced in the form of the Cambodian Community Coalition for partnership purposes in this study, including of members of the Cambodian Women’s Association, Chair of the Cambodian Cultural Heritage Association, Program Coordinator of the Khmer Community of Seattle-King County, medical interpreters, and public health case managers. Community members were also recruited as research assistants to aid in the collection and analysis of qualitative data.
Methods
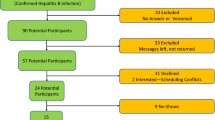
A convenience sample of 97 Cambodian men (48) and women (49) was recruited for participation in eight group interviews. Interview groups were segregated by age (20–39 and 40–64) and gender. This segregation influenced the manner in which the groups were conducted, and the language spoken. The groups held with men and women 40 and older were conducted in Khmer. Those with men and women 20–39 were conducted in a mixture of Khmer and English, depending on the comfort level of the speaker. Group interviews were facilitated by bilingual, bicultural research assistants and were recorded with the explicit consent of participants. All research activity was reviewed and approved by the Fred Hutchison Cancer Research Center Institutional Review Board for the Protection of Human Subjects. Recordings were translated into English for coding and analysis.
Focus groups were conducted in community centers and public libraries. Participants were recruited through community coalition members’ and research assistants’ social networks. To facilitate recruitment, participants were offered a small stipend ($20), and light refreshments. Eight focus groups were conducted on the topics of hepatitis B and liver cancer. The purpose of the groups was to generate discussion amongst group members about culturally informed understandings of health and illness; differences in health practices in the US and Cambodia; understandings of hepatitis B as an illness; understandings of hepatitis B testing; understandings of hepatitis B treatment; and feelings about and understandings of vaccination. At the close of each group, participants were asked individually about their hepatitis B testing status. Fifty-five percent of participants (n = 53) reported previous testing, 38% (n = 37) reported no prior testing, and 7% (n = 7) did not answer the question. Table 1 details demographic information on participants.
We followed standard qualitative analysis techniques in this study, including iterative data review, multiple coders, and “member checking” [4]. Transcripts from group interviews were reviewed by five members of the research team and coded by two. Each coder individually coded the transcript for concepts and themes. Other members of the research team reviewed each transcript and developed “summary documents” which highlighted new ideas and concepts, recurrent ideas and concepts, and patterns or themes noted across transcripts. These summary documents were shared among the team and discussed in group meetings following each set of group interviews, and prior to the next set. This scaffolding approach enabled the incorporation of findings into questions for subsequent groups. For example, once we started learning about the different ways stages of liver disease were described, we began probing around this topic to identify possible variations in understanding influenced by age or gender. Following this inductive approach meant that group interviews changed over time and did not always cover the same topics. The main themes identified in this collaborative analysis process, ongoing throughout the qualitative data collection phase, serve as the basis for development of intervention materials.
Results
Focus group discussions revealed social and cultural issues important to hepatitis B and liver cancer programs focused on Cambodian Americans. Participants discussed a range of understandings and concerns about hepatitis B illness, transmission and prevention, spanning from etiology informed by humoral theories underlying Khmer medicine to more biomedical understandings of disease course. When content was unclear, the interactive nature of the group discussion aided in bringing about a common understanding of concepts and perceptions, or the clarification that a common understanding did not exist within the group [36]. This became particularly important when trying to establish a common ground for discussing hepatitis B. It became clear from the outset that hepatitis was commonly understood as Chumnguh Thleum (liver disease) and Keut Leoung (yellow skin disease). Discussion within the groups clarified that there were variations on understanding of the different types of hepatitis (e.g., hepatitis A being the first stage of illness, leading to B, then to C, which is the worst) and symptom terminology (e.g., Krenn (tough liver), Teach Teuk (swollen belly), and Tleum Krin (dysfunctional liver)). Observation of the expression of opinions and views about the function of the liver and its varying stages of illness illustrated the wide range of understandings and the lack of consensus on terminology and perception, despite the opportunity for discussion. This lack of consensus provides an opportunity for appropriately framed education.
We categorized the content of these discussions into dominant themes about liver health and illness influenced by (1) Theravada Buddhist beliefs and practices, Khmer medicine, and experiences with/understandings of biomedicine (Therapeutic Pluralism); and (2) beliefs about hepatitis B transmission and causes embedded in personal experiences and socio-historical circumstances of migration (Transculturation).
Therapeutic Pluralism
Cultural practices and approaches to health and illness emanate from a combination of Theravada Buddhism, Khmer medicine, French medicine, and since resettlement, interactions with biomedical practitioners in the US. Theravada Buddhism emphasizes spiritual purification through individual good behavior and meritorious deeds [3, 15]. Suffering is a central notion; suffering is inevitable and elemental to happiness [30]. The physical body is viewed as in unity with the social self and the soul. After death, the soul separates from the body and continues existence, hopefully in a higher reincarnated form [35, p. 1253]. As Becker and others point out, the experience of the Khmer Rouge genocide created a crisis of meaning [3, 30]. The general concept of suffering, central to Khmer Buddhist beliefs, was completely inadequate to represent the “cataclysmic disruption that the genocide caused Cambodians and an entire way of life” [3, p. S84]. So while these beliefs remain foundational—illustrated in participants’ evocation of them (as one man told us when discussing how one stays healthy, “there are three things we should follow. They are Buddha, Dharma, and Sangkha” (FG 5 400))—they have shifted and transformed in response to socio-historical and personal experiences, as have attendant practices.
Khmer medicine is a product of medical beliefs and practices adapted from the 1000-year rule of the Chinese [8, 27] combined with Ayurvedic, animistic, and French pharmaceutical traditions [26, 42]. Medical anthropologists have recorded the practice of medical pluralism—the combining of different traditions of therapeutic practices by one person or in one system—in many groups and contexts throughout the world [20]. The experiences Cambodian-Americans shared in our group interviews are no exception. Participants discussed the use of dermabrasive techniques, the goals of which are to “rub out the wind” (Kyal, noxious vapors that invade the body and cause disease symptoms), including coining (Kos Kyal), pinching (Chap Kyal), and cupping (Chubb Kyal). These techniques are used to restore balance among elements of the body, and between the body and the environment, disrupted by hot and cold winds [31, 35]. Balance maintaining practices such as these and other dietary regimes are linked with social practices of commemorating dead ancestors. The belief that physical well-being is intimately connected with nurturing one’s social relations in this world and the next has been shown to be central to Khmer healing and health [35].
Participants in our group interviews were mixed on their feelings about dermabrasive practices, however, as many in the community had been criticized for their use and feared being prosecuted for abuse when treating their children with these methods. Some younger participants expressed distress about having been subjected to coining (Kos Kyal) when they were children, believing it was a form of abuse. Others adapted to the expectations of their new environments, only cupping (Chubb Kyal) and coining (Kos Kyal) below the neckline so the marks wouldn’t be visible while clothed. For example, one woman told us,
That’s why when I go to work my coworkers said I got beat up. When I did it the next time, I only did it in hidden parts of my body (FG W 032809: 1069–1072).
Men in one group discussed using coining and taking Advil to address different illnesses. Women in another group discussed taking Tylenol and Nyquil, running to “sweat out” illness, and eating garlic. Women also spoke of Kos Kyal (coining) instead of seeing the doctor when ill for fear of catching something from others in the waiting room. One woman noted how she combined and chose between over-the-counter medicine and coining depending on her symptoms:
If I’m not really sick, I just Kos Kyal or take some medicines. If Kos Kyal doesn’t make me feel better, I’ll take some medicines. If I just have a headache without fever, I’ll Kos Kyal. If I have fever too, I don’t Kos Kyal, I just take medicine (FG6 364–369).
According to humoral theories underlying Khmer medicine an appropriate hot–cold balance is requisite to maintain health. Disease may disturb this necessary balance [42]. As one participant stated, “If you have too much of anything, your heart can explode…It’s all about balance” (FG M 053009: 1739–1740). In response to sickness, or in order to avoid or prevent illness, hot and cold foods may be selected to prevent imbalances in the body, or to restore the sick body to health. Participants spoke of wine, oils, meats, and fried foods being hot and detrimental to liver health, and cooling vegetables such as bitter melon, Spey and Sdaow/Sdav (green vegetables), Khat Nah (Chinese broccoli), Tror Koun (morning glory), and soy milk as healing. A participant told us, “It seems like any cold food helps cure hepatitis or any other liver illness” (FG W 032809: 1737–1738).
The vulnerability caused by being out of balance and the interconnection of bodily systems endemic to Khmer medicine was expressed by one woman in terms of a weakened immune system, exemplifying the synergy between traditional etiology and biomedical understandings of susceptibility among our participants.
I think our immune system becomes weak when we have a disease, and that disease does not have to be hepatitis B. When our immune system becomes weak, we do not have antibody to protect us. So it’s easy for viruses to attack us. For example, if I had hepatitis B, it would be easy for me to catch a cold, cough, or headache (FG4 1169).
This synergy between biomedical concepts (antibodies, viruses, immune system) and tenets of Khmer medical theories (interconnectedness of bodily systems and surrounding environment, importance of balance in body and mind, influence of hot and cold) when speaking about preventing liver disease (Chumnguh Thleum) was also expressed in participants’ discussion of vitamins, exercise, and doctors visits alongside meditation and dermabrasive techniques. Several participants recited information received from hospital visits and doctors regarding hepatitis B transmission and disease progression, which they reinterpreted in an integrative manner reflective of their pluralistic practices. For example, one man said:
Yes, it [hepatitis] progresses from B to C. If we don’t wash hands, it could spread hepatitis A. For A, for example, the cook, who makes food for us, goes to the restroom and does not wash his hand or drop his sweat; this would definitely spread hepatitis A. If we do not check up or protect ourselves, later it will develop to B or C. For this disease, once we have A or B, it will develop to C (FG5 1214–1221).
Just as bodily systems are interconnected and mutually influential, types of hepatitis are interconnected and mutually influential.
A woman in another group reversed the order of severity implied by the progression discussed by others: “Hepatitis A is deadly. Hepatitis B, not very good. Hepatitis C, oh, you’re okay” (FG8 1002–1004). Another offered a different interpretation: “I don’t think it’s a progression. I think there’re different classes of them, different class, different categories. There’s a nurse that was saying that there’s different stages” (FG8 1206–1209). A woman from another group noted the relationship between the forms of hepatitis in the following:
A is on skin only. B reaches the liver. C is the worst. Our livers would be Krenn (tough, small, hard)…When the liver is Krenn, it becomes partially hard and it won’t excrete enough. We will be sick. That’s what I heard (FG6 802).
Participants discussed across groups that the eventual end to this progress was liver cancer (Moha reek Thleum), which to many of them was equivalent to death. As one woman stated when describing what hepatitis leads to, “It’s the breakdown of the liver…It’s the cancer of the liver” (FG W 053009: 1178–1179). Connected to these understandings of the different forms of hepatitis was the association between hepatitis and HIV/AIDS. In one group, hepatitis A was posited as a precursor to HIV/AIDS. In others, the two diseases, HIV and hepatitis, were conflated, due to their association with sexual transmission. As one woman shared,
I thought there’s no cure for AIDS yet and I thought AIDS was part of hepatitis. So, one form of hepatitis I didn’t think there’s a cure for it (FG 8 1475–1477).
In another group hepatitis B was equated with Tuberculosis.
Other research has noted Southeast Asian Understandings of the blood as a limited and non-regenerative quantity [31, 32]. Participants in our study noted that hepatitis B may be referred to as Rok (blood disease). People with hepatitis B may describe their illness in terms of bad blood, contaminated blood, or unclean blood and may attribute hepatitis to blood problems rather than the liver. As one participant noted, hepatitis B may be described as “white blood eats red blood disease” (Cheam Soh See Cheam Krohorm) (FG8 1058–1085). “When the red blood was eaten,” a man in another group interview said, “then our skin becomes pale” (FG M 042509: 0810–0812).
Transculturation: The Endurance of Memory
The connection between the living and the dead, the concept of suffering, and the experiences of the genocide and its aftermath form the basis of the connections participants made between personal experiences, socio-historical circumstances, and understandings of liver disease (Chumnguh Thleum). While we never asked directly about the genocide, memories and reflections of how different life was “before,” and how these differences informed illness prevalence were the backdrop to many of our discussions. As one young woman noted, “I know there are a lot of mental health issues. With my parents, my aunts and uncles…they have a lot of stress because they think about stuff too much. I don’t know if it’s the trauma or whatever…” (FG8 0135–0139). Another in the same group, referring to the lack of discussion within families about the effects of the war and her own grandparents’ experiences, noted, “They’re from the Khmer Rouge. I don’t know if it’s related to the trauma they went through or if it was a health issue or if it’s just part of aging” (FG8 0183–0187). Other participants evoked the genocide when referring to healing practices under the Khmer Rouge (medicinal teas) and testing for TB and hepatitis in Thai refugee camps.
Participants referred to their lives in Cambodia (Srok Khmer), their continuing connection with family there, and the persistence of cultural practices in the US when discussing their thoughts on the causes and spread of hepatitis. Anthropologists refer to these cultural change processes as transculturation—multidimensional cultural transformations including structural (historical, economic, social, political) and cultural contexts [1] as well as the fluidity of identity formation that accompanies cultural change [2]. Participants regularly mentioned the way people eat together and share food as particularly Khmer. At times, this was linked to explicit distinctions between hepatitis types (e.g., spreading hepatitis A through food sharing), while at other times food sharing was seen as the cause of liver disease (Chumnguh Thleum) as all hepatitis linked together in stages. As one woman stated,
You know how Khmer people eat like family style. Some families have like a dinner spoon. And some families just kind of use their own spoon, but everybody’s eating and just dipping in the same pot (FG W 053009: 1017–1020).
Another, reflecting on her friend’s family, noted:
Yes, my friend’s father has hepatitis B and he got cancer. It was apparently from him sharing chopsticks, food (FG W 053009: 1010–1012).
Several participants noted that the environment and way of life in Srok Khmer (Cambodia) might foster illnesses such as hepatitis. As one woman stated, “That’s why I think it’s common in Srok Khmer and maybe Asia, because the sanitation. Because you have the livestock, you have the chickens, you have the people living in very remote conditions. I think it’s the cleanliness and bacteria” (FG W 053009: 1242–1246). Others reported sending money back to Cambodia every month to pay for their children’s hepatitis treatments.
The transition to the US was noted as a process that predisposed people to either discovering that they had hepatitis or to potentially causing it. One man stated,
When people come here, they get sicker. When they’re in Srok Khmer, they have been doing this and that and they’re fine. So I guess, in a way, it’s a transition. Because you don’t really see that much in Srok Khmer about cancer, but as soon as you come here, you start getting the disease. So, there’s something to that. Whatever food we eat over here is totally different than the food they eat over there (FG M 053009: 1686–1695).
This shift in environment also influenced the efficacy of Khmer medicine. Some participants noted that Khmer medicine was no longer effective in the US; that the new environment called for new approaches to healing:
When we moved here we never used traditional medicine because it is not effective anymore. Since we eat new food, [we must] adjust to the new environment and new weather (FG M 030609: 0715–0717).
In the US, participants noted, people turn to the doctor when they have run out of other options. In Cambodia, they would go to the Kru Khmer (shaman, healer), use injections, and home remedies. “Some people pray, some would prefer traditional medicine. They just try all the available options” (FG M 030609: 0444–0445); options that differ depending on whether they are in the US or Cambodia.
Participants were very familiar with and receptive to the importance of vaccination as many had received numerous vaccinations as part of their resettlement experience. These were required, they noted, before they could enter the US. Also, the need to get vaccinations before returning to Cambodia was a source of knowledge. An older man noted “For those who visit Cambodia very often get vaccinated” (FG M 030609: 1131–1132). A young woman recounted her experience:
When I went to Srok Khmer, I was required to take two vaccinations…Hepatitis shot and vaccination. Down in the rural countryside they have malaria. From Srok Khmer is very high because Srok Khmer is not so sanitary, not very clean out there, and you don’t have a lot of the systems that we have here (FG8 0891–0901).
Continued connection to their homeland—through remittances, travel, regular communications, and memory—influenced understandings of and engagement with hepatitis vaccination programs and highlighted the fluid and integrative process of understandings of disease course and causation [5, 6, 21].
Discussion
Members of our research team conducted a community-based telephone survey to describe Cambodian American’s hepatitis B knowledge, testing, and vaccination levels in Seattle, WA in 2005–2006 [43]. This study found that less than one half (46%) of the study group (N = 111) had received a hepatitis B blood test, and about one third (35%) had been vaccinated against hepatitis B. Only 43% knew that Cambodian Americans are more likely to be infected with hepatitis B than Whites. Less than half of the respondents knew that hepatitis B could be spread during sexual intercourse (46%) and relatively few knew that hepatitis B could not be transmitted by eating food prepared by an infected person (28%) or by coughing and sneezing (32%) [43]. When compared with the 1999 survey of Cambodian women in Seattle, the 2005–2006 survey results indicate that improvements in hepatitis B testing levels have been modest. Specifically, 38% of Cambodian women who completed the survey reported having previously been tested for hepatitis B, compared to 46% of the Cambodian women who completed the 2005–2006 survey [43].
Other recent studies have also documented low hepatitis B testing rates and variable understandings of illness causes and transmission routes [9, 10, 14]. Analyzing REACH 2010 Risk Factor Survey Data from four US communities, Grytdal and colleagues showed that Cambodian Americans were less likely than Vietnamese Americans to have been tested for HBV. Specifically, only 49% of Cambodian Americans reported that they had ever been tested for HBV infection [14]. However, self-reported vaccination rates for Cambodian and Vietnamese Americans were very similar in this study [14]. Recent work in Lowell, MA, argues that outreach and education based on a recognition of community strengths, resources, and local context (e.g., historical context of migration and genocide) which builds upon community participation and partnership is a viable approach to health promotion with Cambodians in the United States [13].
Our findings indicate that participants hear and repeat biomedical information received from nurses and doctors regarding hepatitis B. They are largely integrated into the health care system in the Seattle-Tacoma area. However, as indicated in the quotes included in this paper, they reinterpret this information in an integrative manner that incorporates and is consistent with Khmer medical beliefs. Understanding this process is essential to developing appropriate health education. Qualitative research that encourages an understanding and reflection of participants’ experience and the meanings they give to these experiences (e.g., interacting with health care providers in the US, experiencing vaccination during refugee “processing”, or reflecting on Khmer medical practices in the US and in Thai refugee camps) is an essential foundation to outreach and education efforts focused on immigrant groups [5, 22].
A limitation and strength of this paper is its focus on understandings of hepatitis B and liver illness in a community of Cambodian immigrants living in Seattle-Tacoma. While not generalizable, this focus provides insights into the local sociocultural context of Cambodian immigrants in Seattle-Tacoma and local relevance for our intervention materials and outreach plan. The themes identified and reported here have emerged in various forms in previous studies [26, 35, 39, 42]. However, this is the first study to investigate therapeutic pluralism and transculturation processes with the aim of identifying understandings and practices for the treatment and prevention of hepatitis B-induced liver disease. As such, this effort is in keeping with the Institute of Medicine’s call for more focus on “qualitative, ethnographic research that examines the historical, social, and cultural contexts of diverse communities’ health behavior” [17] to adequately address disparities in health outcomes.
References
Abraido-Lanza, A. F., Armbrister, A., Florez, K. R., & Agirre, A. (2006). Toward a theory-driven model of acculturation in public health research. American Journal of Public Health, 96, 1342–1346.
Amaro, H., & de la Torre, A. (2003). Public health needs and scientific opportunities in research on Latinas. American Journal of Public Health, 92, 525–529.
Becker, G. (2002). Dying away from home: Quandaries of migration for elders in two ethnic groups. Journal of Gerontology: Social Sciences, 57(2), S79–S95.
Bernard, H. R., & Ryan, G. W. (2009). Analyzing qualitative data. Walnut Creek, CA: Sage Publications.
Burke, N. J., Jackson, C. J., Chan, H. C., Stackhouse, F., Nguyen, T., Chen, A., et al. (2004). “Honoring tradition, accepting new ways”: Development of a hepatitis B control intervention for Vietnamese immigrants. Ethnicity and Health, 9(2), 153–169.
Burke, N. J., Joseph, G., Pasick, R. J., & Barker, J. C. (2009). Theorizing social context: Re-thinking behavioral theory. Health Education and Behavior, 36(Suppl. 1), 55S–70S.
Chandler, D. (1991). The tragedy of Cambodian history: Politics, war, and revolution since 1945. New Haven, CT: Yale University Press.
Chandler, D. (Ed.). (2000). A history of Cambodia (3rd ed.). Boulder, CO: Westview Press.
Chiehwen, E. H., Chih-Hung, L., Hee-Soon, J., Yu-Wen, C., Bawa, J., Tillman, U., et al. (2007). Reducing liver cancer disparities: A community-based hepatitis B prevention program for Asian-American communities. Journal of the National Medical Association, 99(8), 900–907.
Colvin, H. M., & Mitchell, A. E. (Eds). (2009). Hepatitis and liver cancer: A national strategy for prevention and control for hepatitis B and C. Committee on the prevention and control of viral hepatitis infections: Institute of Medicine, http://www.nap.edu/catalog/12793.html.
Ghosh, C. (2003). Healthy people 2010 and Asian Americans/Pacific Islanders: Defining a baseline of information. American Journal of Public Health, 93, 2093–2098.
Green, L. W., George, M. A., Daniel, M., Frankis, C. J., Herbert, C. P., Bowie, W. R., et al. (2003). Guidelines for participatory research in health promotion. In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health. San Francisco: Jossey-Bass.
Grigg-Saito, D., Och, S., Liang, S., Toof, R., & Silka, L. (2008). Building on the strengths of a Cambodian refugee community through community-based outreach. Health Promotion Practice, 9(4), 415–425.
Grytdal, S. P., Liao, Y., Chen, R., Garvin, C. C., Grigg-Saito, D., Kagawa-Singer, M., et al. (2009). Hepatitis B testing and vaccination among Vietnamese- and Cambodian-Americans. Journal of Community Health, 34(3), 173–180.
Hopkins, M. C. (1996). Braving a new world: Cambodian (Khmer) refugees in an American city. Westport, CT: Bergin & Garvey.
Institute of Medicine. (2001). Unequal treatment: Confronting racial and ethnic disparities in healthcare, Vol. 564, p. 566.
Institute of Medicine. (2002). Committee on communication for behavior change in the 21st century: Improving the health of diverse populations. In Speaking of health: Assessing health communication strategies for diverse populations. Washington, DC: National Academies Press.
Israel, B. A., Schulz, A. J., Parker, E. A., Becker, A. B., Allen, A. J., & Guzman, J. R. (2003). Critical issues in developing and following community based participatory research principals. In M. Minkler & N. Wallerstein (Eds.), Community-based participatory research for health. San Francisco: Jossey-Bass.
Israel, B. A., Schulz, A. J., Parker, E. A., & Becker, A. B. (1998). Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health, 19, 173–202.
Johannessen, H., & Lazar, I. (Eds.). (2006). Multiple medical realities: Patients and healers in biomedical, alternative and traditional medicine. New York: Berghahn Books.
Joseph, G., Burke, N. J., Tuason, N., & Pasick, R. (2009). Perceived susceptibility and perceived benefits in the context of transculturation and transmigration. Health Education and Behavior, 36(Suppl. 1), 71S–90S.
Kagawa-Singer, M. (1998). Cancer and Asian American cultures. Asian American Pacific Islander. Journal of Health, 6(2), 383–399.
Kem, R., & Chu, K. C. (2007). Cambodian cancer incidence rates in California and Washington, 1998–2002. American Cancer Society. doi:10.1002/cncr.22914. www.interscience.wiley.com.
Kiernan, B. (1996). The Pol Pot regime: Race, power, and genocide in Cambodia under the Khmer Rouge, 1975–1979. New Haven, CT: Yale University Press.
Kiernan, B. (September 2004). Coming to terms with the past in Cambodia. History Today, 16–18.
Lewis, D. C. (2007). A hierarchy of medicine: Health strategies of elder Khmer refugees in the United States. The Qualitative Report, 12(2), 146–165. Retrieved [2010], from http://www.nova.edu/ssss/QR/QR12-2/lewis.pdf.
Lovell, M. L., Tran, T., & Nguyen, C. D. (1987). Refugee women: Lives in transition. International Social Work, 30, 317–325.
Mahloch, J., Jackson, J. C., Chitanorong, K., Sam, R., Ngo, L. S., & Taylor, V. M. (1999). Bridging culture through the development of a Cambodian cervical cancer screening video. Journal of Cancer Education, 14, 114.
Marin, G., Burhansstipanov, L., Connell, C., Gielen, A., Helitzer-Allen, D., Lorig, K., et al. (1995). A research agenda for health education among underserved populations. Health Education Quarterly, 22(3), 346–363.
Mortland, C. A. (1994). Khmer Buddhists in the United States: Ultimate questions. In M. M. Ebihara, C. A. Mortland, & J. Ledgerwood (Eds.), Cambodian culture since 1975: Homeland and exile (pp. 72–90). Ithaca, NY: Cornell University Press.
Muecke, M. A. (1983). Caring for Southeast Asian refugee patients in the USA. American Journal of Public Health, 73, 431.
Muecke, M. A. (1983). In search of Healers-Southeast Asian Refugees in the American healthcare system. In Cross-cultural medicine. West J Med, Vol. 139, pp. 835–840.
Muecke, M. A. (1995). Trust, abuse of trust, and mistrust among Cambodian refugee women: A cultural interpretation. In E. V. Daniel & J. C. Knudsen (Eds.), Mistrusting refugees (pp. 36–55). Berkeley: University of California Press.
Niedzwiecki, M., & Tuang, T. C. (2004). Southeast Asian American statistical profile. Washington, DC: Southeast Asian Resource Action Center.
Ong, A. (1995). Making the biopolitical subject: Cambodian immigrants, refugee medicine, and cultural citizenship in California. Social Science and Medicine, 40(9), 1243–1257.
Onwuegbuzie, A. J., Dickinson, W. B., Leech, N. L., Zoran, A. G. (2009). A qualitative framework for collecting and analyzing data in focus group research. International Journal of Qualitative Methods, 8(3), 1–21.
Perkins, C. I., Morris, C. R., Wright, W. E., & Young, J. L. (1995). Cancer incidence and mortality in California by detailed race/ethnicity, 1988–1992. Sacramento: California Department of Health Services.
Pfeifer, M. E. (2005). Census releases 2005 American community survey data for Southeast Asian Americans. Accessed 2007, from www.hmongstudies.org.
Pickwell, S. (1999). Multilevel healing pursuits of Cambodian refugees. Journal of Immigrant Health, 1, 165–179.
Pollack, H., Wan, K., Ramos, R., et al. (2006). Screening for chronic hepatitis B among Asian/Pacific Islander populations—New York City, 2005. MMWR. Morbidity and Mortality Weekly Report, 55, 505–509.
President’s Advisory Commission on Asian Americans, Pacific Islanders. (2003). Asian Americans and Pacific Islanders—Addressing health disparities: Opportunities for buildings a healthier America. Washington, DC: Department of Health and Human Services.
Sargent, C., & Marcucci, J. (1984). Aspects of Khmer medicine among refugees in urban America. Medical Anthropology Quarterly, 16(1), 7–9.
Taylor, V. M., Seng, P., Acorda, E., Sawn, L., & Li, L. (2009). Hepatitis B knowledge and practices among Cambodian immigrants. Journal of Cancer Education, 24(2), 100–104.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Burke, N.J., Do, H.H., Talbot, J. et al. Chumnguh Thleum: Understanding Liver Illness and Hepatitis B Among Cambodian Immigrants. J Community Health 36, 27–34 (2011). https://doi.org/10.1007/s10900-010-9277-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-010-9277-y