Abstract
Purpose
To investigate the co-influences of age and morbidity severity on physical health in adult family practice populations.
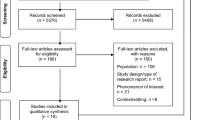
Methods
Morbidity data in a 12-month period for 7,833 older English consulters aged 50 years and over and 6,846 Dutch consulters aged 18 years and over was linked to their physical health status obtained from cross-sectional health surveys. Individual patients were categorised using 78 consulting morbidities classified by a chronicity measure (acute, acute-on-chronic and chronic) into an ordinal scale of morbidity severity ranging from single to multiple chronicity groups. Associations between morbidity severity, age and SF-12 Physical Component Summary (PCS) score were assessed using linear regression methods.
Results
Increased age and higher morbidity severity were significantly associated with poorer physical health. Of the explained total variance in adjusted PCS scores, an estimated 43% was attributed to increasing age, 40% to morbidity severity and 17% to deprivation for English consulters; the figures were 21, 42 and 31%, respectively for Dutch consulters. The largest differences in PCS scores between severity categories were observed in the younger age groups.
Conclusions
Morbidity severity and age mainly act separately in adversely influencing physical health. In ageing populations who will experience higher multimorbidity, this study underlines the importance that health care and public health will need to address morbidity severity and ageing as related but distinct issues.


Similar content being viewed by others
References
Seeman, T. E., Guralnik, J. M., Kaplan, G. A., Knudson, L., & Cohen, R. (1989). The health consequences of multiple morbidity in the elderly. The Alameda County study. Journal of Aging and Health, 1(1), 50–66. doi:10.1177/089826438900100104.
Brayne, C., Matthews, F. E., McGee, M. A., & Jagger, C. (2001). Health and ill-health in the older population in England and Wales. The Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Age and Ageing, 30(1), 53–62. doi:10.1093/ageing/30.1.53.
Starfield, B. (2006). Threads and yarns: Weaving the tapestry of comorbidity. Annals of Family Medicine, 4(2), 101–103. doi:10.1370/afm.524.
Verbrugge, L. M., & Jette, A. M. (1994). The disablement process. Social Science and Medicine, 38(1), 1–14. doi:10.1016/0277-9536(94)90294-1.
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D., & Anderson, G. (2004). Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 59(3), 255–263.
Kroenke, K., & Price, R. K. (1993). Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Archives of Internal Medicine, 153(21), 2474–2480. doi:10.1001/archinte.153.21.2474.
van den Akker, M., Buntinx, F., Metsemakers, J. F., Roos, S., & Knottnerus, J. A. (1998). Multimorbidity in general practice: Prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. Journal of Clinical Epidemiology, 51(5), 367–375. doi:10.1016/S0895-4356(97)00306-5.
Starfield, B., Lemke, K. W., Herbert, R., Pavlovich, W. D., & Anderson, G. (2005). Comorbidity and the use of primary care and specialist care in the elderly. Annals of Family Medicine, 3(3), 215–222. doi:10.1370/afm.307.
Fortin, M., Bravo, G., Hudon, C., Lapointe, L., Almirall, J., Dubois, M. F., et al. (2006). Relationship between multimorbidity and health-related quality of life of patients in primary care. Quality of Life Research, 15(1), 83–91. doi:10.1007/s11136-005-8661-z.
Hoffman, C., Rice, D., & Sung, H. Y. (1996). Persons with chronic conditions. Their prevalence and costs. Journal of the American Medical Association, 276(18), 1473–1479. doi:10.1001/jama.276.18.1473.
Hardy, S. E., Dublin, J. A., Holford, T. R., & Gill, T. M. (2005). Transitions between states of disability and independence among older persons. American Journal of Epidemiology, 161(6), 575–584. doi:10.1093/aje/kwi083.
Rockwood, K., & Mitnitski, A. (2007). Frailty in relation to the accumulation of deficits. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 62(7), 722–727.
Guccione, A. A., Felson, D. T., Anderson, J. J., Anthony, J. M., Zhang, Y., Wilson, P. W., et al. (1994). The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. American Journal of Public Health, 84(3), 351–358. doi:10.2105/AJPH.84.3.351.
Fried, L. P., Bandeen-Roche, K., Kasper, J. D., & Guralnik, J. M. (1999). Association of comorbidity with disability in older women: The Women’s Health and Aging Study. Journal of Clinical Epidemiology, 52(1), 27–37. doi:10.1016/S0895-4356(98)00124-3.
Kadam, U. T., Croft, P. R., & North Staffordshire GP Consortium Group. (2007). Clinical multimorbidity and physical function in older adults: A record and health status linkage study in general practice. Family Practice, 24(5), 412–419. doi:10.1093/fampra/cmm049.
Wolff, J. L., Starfield, B., & Anderson, G. (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine, 162(20), 2269–2276. doi:10.1001/archinte.162.20.2269.
Guralnik, J. M., Ferrucci, L., Penninx, B. W., Kasper, J. D., Leveille, S. G., Bandeen-Roche, K., et al. (1999). New and worsening conditions and change in physical and cognitive performance during weekly evaluations over 6 months: The Women’s Health and Aging Study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 54(8), M410–M422.
Kadam, U. T., Jordan, K., & Croft, P. R. (2005). Clinical comorbidity was specific to disease pathology, psychologic distress, and somatic symptom amplification. Journal of Clinical Epidemiology, 58(9), 909–917. doi:10.1016/j.jclinepi.2005.02.007.
Kadam, U. T., Jordan, K., & Croft, P. R. (2006). A comparison of two consensus methods for classifying morbidities in a single professional group showed the same outcomes. Journal of Clinical Epidemiology, 59(11), 1169–1173. doi:10.1016/j.jclinepi.2006.02.016.
Kadam, U. T., Schellevis, F. G., van der Windt, D. A. W. M., de Vet, H. C. W., Bouter, L. M., & Croft, P. R. (2008). Morbidity severity classifying routine consultations from English and Dutch general practice indicated physical health status. Journal of Clinical Epidemiology, 61(4), 386–393. doi:10.1016/j.jclinepi.2007.05.014.
Jinks, C., Jordan, K., Ong, B. N., & Croft, P. (2004). A brief screening tool for knee pain in primary care (KNEST). 2. Results from a survey in the general population aged 50 and over. Rheumatology (Oxford, England), 43(1), 55–61. doi:10.1093/rheumatology/keg438.
Thomas, E., Wilkie, R., Peat, G., Hill, S., Dziedzic, K., & Croft, P. (2004). The North Staffordshire Osteoarthritis Project—NorStOP: Prospective, 3-year study of the epidemiology and management of clinical osteoarthritis in a general population of older adults. BMC Musculoskeletal Disorders, 5, 2. doi:10.1186/1471-2474-5-2.
Westert, G. P., Schellevis, F. G., de Bakker, D. H., Groenewegen, P. P., Bensing, J. M., & van der Zee, J. (2005). Monitoring health inequalities through general practice: The Second Dutch National Survey of General Practice. European Journal of Public Health, 15(1), 59–65. doi:10.1093/eurpub/cki116.
Harding, A., & Stuart-Buttle, C. (1998). The development and role of the Read Codes. Journal of American Health Information Management Association, 69(5), 34–38.
Bentsen, B. G. (1986). International classification of primary care. Scandinavian Journal of Primary Health Care, 4(1), 43–50. doi:10.3109/02813438609013970.
Ware, J. E., Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483. doi:10.1097/00005650-199206000-00002.
Jenkinson, C., Layte, R., Jenkinson, D., Lawrence, K., Petersen, S., Paice, C., et al. (1997). A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health Medicine, 19(2), 179–186.
Townsend, P., Phillimore, P., & Beattie, A. (1988). Health and deprivation: Inequality and the north. London: Croom Helm.
Mitnitski, A., Song, X., & Rockwood, K. (2007). Improvement and decline in health status from late middle age: Modeling age-related changes in deficit accumulation. Experimental Gerontology, 42(11), 1109–1115.
O’Halloran, J., Miller, G. C., & Britt, H. (2004). Defining chronic conditions for primary care with ICPC-2. Family Practice, 21(4), 381–386. doi:10.1093/fampra/cmh407.
Schram, M. T., Frijters, D., van de Lisdonk, E. H., Ploemacher, J., de Craen, A. J., de Waal, M. W., et al. (2008). Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. Journal of Clinical Epidemiology, 61(11), 1104–1112. doi:10.1016/j.jclinepi.2007.11.021.
Acknowledgements
UTK is currently funded by a National Institute for Health Research Post-Doctoral Fellowship, and was funded by the Medical Research Council (MRC) Training Fellowship in Health Services Research at the start of this work. Project funding was from the Claire Wand Fund, North Staffordshire Primary Care Research Consortium, MRC Programme grant and NHS Research and Development funds.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Examples of the morbidities classified with a 1-year period of prevalence for English and Dutch samples (Table 4).
Appendix 2
Comparison of sub-groups of the study to the overall groups (Table 5).
Rights and permissions
About this article
Cite this article
Kadam, U.T., Schellevis, F.G., Lewis, M. et al. Does age modify the relationship between morbidity severity and physical health in English and Dutch family practice populations?. Qual Life Res 18, 209–220 (2009). https://doi.org/10.1007/s11136-009-9442-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-009-9442-x