Abstract
BACKGROUND
Physician opinion can influence the prospects for health care reform, yet there are few recent data on physician views on reform proposals or access to medical care in the United States.
OBJECTIVE
To assess physician views on financing options for expanding health care coverage and on access to health care.
DESIGN AND PARTICIPANTS
Nationally representative mail survey conducted between March 2007 and October 2007 of U.S. physicians engaged in direct patient care.
MEASUREMENTS
Rated support for reform options including financial incentives to induce individuals to purchase health insurance and single-payer national health insurance; rated views of several dimensions of access to care.
MAIN RESULTS
1,675 of 3,300 physicians responded (50.8%). Only 9% of physicians preferred the current employer-based financing system. Forty-nine percent favored either tax incentives or penalties to encourage the purchase of medical insurance, and 42% preferred a government-run, taxpayer-financed single-payer national health insurance program. The majority of respondents believed that all Americans should receive needed medical care regardless of ability to pay (89%); 33% believed that the uninsured currently have access to needed care. Nearly one fifth of respondents (19.3%) believed that even the insured lack access to needed care. Views about access were independently associated with support for single-payer national health insurance.
CONCLUSIONS
The vast majority of physicians surveyed supported a change in the health care financing system. While a plurality support the use of financial incentives, a substantial proportion support single payer national health insurance. These findings challenge the perception that fundamental restructuring of the U.S. health care financing system receives little acceptance by physicians.
Similar content being viewed by others
INTRODUCTION
The number of uninsured Americans now stands at 47 million and rises yearly, along with the cost of health insurance1,2. Health care is once again a top domestic policy concern in public opinion polls and reform proposals were featured by the nearly all of the recent presidential candidates3,4. Physicians can have a substantial impact on the political prospects of health care reform, yet few recent data exist on their views on access to care or on specific health care reform proposals.
Current debate about health insurance reform by 2008 presidential candidates4, members of congress5 and prominent policy analysts6–8, and in many state health care reform efforts9, focus on the use of financial incentives to induce uninsured individuals to purchase private health insurance either through tax credits or via mandatory tax penalties. Republican reform proposals have focused on the use of refundable tax credits and tax exempt health savings accounts along with deregulation of insurance markets to promote the goals of greater competition, patient choice and insurance affordability. By contrast, many Democratic proposals focus on a mandate for individuals to acquire coverage (enforced by tax penalties) with subsidies for the poor, expansion of existing public programs, tighter regulation of insurance markets to ensure access to coverage regardless of health status and, often, an employer mandate to offer or contribute to the purchase of employees’ insurance4. Despite these competing philosophical approaches, both use financial incentives for individuals to expand private coverage (individual or employer based) with public coverage available for eligible groups only.
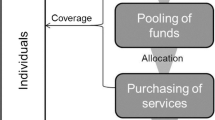
In contrast, proposals for a single-payer national health insurance (NHI) system would replace the current health financing system with a health plan covering all Americans with single-source financing by the government10,11. While such proposals have been proposed for many years, they are not at the center of the current health care reform debate. Such an approach is often regarded as politically unrealistic, because it lacks support among various stakeholders12; incremental reforms are often perceived as more readily attainable13–15.
Previous surveys of physician opinion on single-payer NHI have yielded variable results16–22. The only large nationally representative survey, conducted during 2002, found that 49% of physicians (59% in a recent update)23 supported “national health insurance”, not further defined; 26%, supported a single-payer NHI system24. To our knowledge, no national study has compared support for single-payer NHI with current reform proposals that are based on financial incentives (tax credits or penalties) to induce purchase of private health insurance.
We surveyed a nationally representative sample of practicing physicians regarding their support for single-payer NHI compared with proposals focusing on financial incentives to increase coverage. We also assessed physicians’ views regarding access to medical care in the U.S. health care system.
METHODS
Study Sample and Data Collection
In March 2007, we obtained from the American Medical Association’s (AMA) Master File, a random sample of 3,405 physicians in the U.S. who were engaged in direct patient care as their primary professional activity. The sample size was calculated to provide 90% power to detect specialty-related differences of 15% for our primary study question, assuming a 10% invalid address rate and 50% response rate.
We mailed the survey (with pre-paid postage) to physicians with a brief cover letter requesting study participation. The cover letter was signed by the chiefs of the departments of medicine, pediatrics, surgery and psychiatry at the authors’ hospital, as well as the lead study author (D.M.). Author hospital and medical school affiliations but no other organization or personal names appeared in the letter. For physicians who did not respond within one month, one additional mailing was done with a $1 bill enclosed. The post office returned 105 surveys as undeliverable, leaving a total of 3,300 physicians that received the survey. The survey was conducted between March 16 and October 28, 2007.
Questionnaire Development
We developed a six-item survey on physicians’ support for options to expand health insurance coverage including the status quo, single-payer NHI, and the use of monetary incentives (tax credits or tax penalties). We pre-tested the survey instrument and made four cycles of modifications based on iterative feedback received from five physicians in clinical practice.
We asked respondents to choose the single option they preferred: 1) “The current health care system, in which most people get their health insurance from private employers, but some people have no insurance”; 2) “A universal insurance program in which everybody is covered under a program like Medicare that is run by government and financed by taxpayers”; or 3) “The current health care system, with the addition of new tax credits for buying, or tax penalties for failing to buy, health insurance”. This question was adapted from one used in a recent ABC News / Kaiser Family foundation / CNN survey25 with the addition of the response category regarding tax credits and/or tax penalties.
We also assessed physicians’ views on access to medical care. Respondents were asked whether they agreed or disagreed with the statements: 1) “All Americans should receive needed medical care regardless of ability to pay”; 2) “Currently, people with health insurance have access to the medical care they need”; and 3) “Currently, people without health insurance have access to the medical care they need”. For each statement, respondents were asked to indicate whether they “agree strongly”, “agree somewhat”, “disagree somewhat” or “disagree strongly”.
We also asked respondents to indicate membership in the American Medical Association (AMA).
Finally, for both respondents and non-respondents, we obtained information on gender, geographic location, medical specialty, year of graduation from medical school, and type of practice (hospital-based vs. office-based) from the AMA Master File. We used the respondent’s ZIP code to assign region of the country according to the U.S. Census Bureau classification for region26. We also used ZIP code and Rural–Urban Continuum Codes developed by the Economic Research Service of the U.S. Department of Agriculture27 to assign rural vs. urban status.
Statistical Analysis
We assessed differences in physician support for health care financing options (current system vs. the current system with the addition of tax credits / penalties vs. single-payer NHI) and analyzed these differences according to gender, AMA membership, years of medical practice, medical specialty, type of practice, region, and urban/rural status. For all comparisons, we used the chi-square test for group comparisons, and considered a two-tailed p-value ≤ 0.05 to be statistically significant.
In order to assess whether physicians’ views about access to care are related to their support for a type of health care reform, we used logistic regression models to examine the independent relationship between agreement (agree strongly and agree somewhat combined) or disagreement (disagree strongly and disagree somewhat combined) with each of the three access to care statements and support for a single-payer system (compared with maintaining the current system or using tax credits/penalties). In each model we included terms for physician and practice characteristics that were significantly associated with support for a single-payer system. To identify variables for inclusion in these models, we used a stepwise selection scheme with entry criteria of p < 0.1; variables with a p < 0.05 were retained in the final model. The following were the terms in each final model: physician specialty, practice type, geographic region, number of years since medical school graduation, and membership in the AMA. Data were analyzed using SAS statistical software28.
For analyses of physician specialty, we grouped general internists, family practitioners, general practitioners, pediatricians (non-sub specialists) and geriatricians in the category “primary care.” We categorized medical and pediatric sub specialists as “medical subspecialty” physicians. All surgeons (e.g., orthopedics, general surgery, obstetrics and gynecology, ophthalmology and urology) were analyzed as a single group, as were psychiatrists. Specialties other than one of these were combined into a heterogeneous group, “other.”
In order to assess potential non-response bias in our sample, we compared the characteristics of respondents and non-respondents.
STUDY RESULTS
Response Rate
Of 3,300 physicians who received the survey, 1,675 responded (50.8% response rate).
Characteristics of Respondents
The demographic and professional characteristics of 1,675 respondents and 1,625 non-respondents are presented in Table 1. They did not differ significantly except by year of graduation; respondents graduated slightly earlier.
Views on Access to Care
The overwhelming majority of physicians (88.9%) agreed that all Americans should receive needed medical care regardless of ability to pay (Table 2). Two-thirds of respondents disagreed with the statement that people without health insurance have access to the medical care they need. One-fifth of respondents also disagreed that people with insurance have access to the medical care they need.
Support for Health Care Financing Options
Only 9.1% (95% confidence interval [CI], 7.7–10.5%) of U.S. physicians would preserve the status quo (Table 3). While a plurality (49.2%; 95% CI, 46.8–51.6%) support the current employer-based system with the addition of either tax credits or tax penalties, 41.6% (95% CI, 39.2–44.0%) of physicians support a single-payer NHI program that is run by the government and financed by taxpayers.
Support for health care financing options varied substantially according to characteristics of the respondents (Table 3). Physicians from the Northeast were most likely to support single-payer NHI (52.3% vs. other regions ranging from 37.1% to 39.1%). Physicians from the Midwest were least likely to prefer a change from the current financing system. Primary care, sub-specialist and psychiatric physicians were more likely to support single-payer NHI (48.0%, 46.5 and 63.4%, respectively), while surgeons and physicians in other specialties were more likely to support reform based on financial incentives (64.1% and 56.0%, respectively). Physicians with less than 30 years since medical school graduation were more likely to support financial incentives; those with 30 or more years’ experience were more likely to support single-payer NHI. Office-based physicians were more likely to support financial incentives and hospital-based physicians more likely to support single-payer NHI. Lastly, the majority of AMA members were supportive of financial incentives (55.4%) but among non-members, support for single-payer and financial incentives were nearly equal (44.6% vs. 46.0%).
Views on current access to care were associated with support for single-payer reform (Table 4). In unadjusted analyses, physicians who agreed with the statement that all Americans should receive needed medical care regardless of ability to pay were substantially more likely to support single-payer NHI than the alternatives (Odds Ratio [OR], 10.3 [95% CI, 5.8–19.3]), as were physicians who disagreed that people without health insurance have access to needed medical care (OR, 4.0 [95% CI, 3.1–5.1] and physicians who disagreed that people with health insurance have access to needed medical care (OR, 1.4 (1.1–1.8). Adjustment for physician and practice characteristics did not substantially alter these relationships except that the OR for this last analysis achieved only borderline significance.
DISCUSSION
Only a small fraction of U.S. physicians surveyed supported leaving the U.S. health care financing system as it is. Overall, a plurality supported modifying the current employer-based, private insurance system by the addition of either tax credits or tax penalties to expand coverage. A substantial minority reported prefering an entirely different health care financing system–a taxpayer-financed single-payer NHI program. Such reform was supported by a majority of Northeastern physicians, older physicians, and psychiatrists, and was also endorsed by a plurality of primary care physicians, hospital-based physicians, and medical subspecialists. We also found that the overwhelming majority of physicians believe that all Americans should have access to needed care regardless of ability to pay. Yet, the majority also believes that the uninsured lack such access and one fifth believed that even those with insurance lack adequate access.
To our knowledge, no recent published studies assess physician opinion on single-payer NHI or other financing reform in a nationally representative sample. A physician survey conducted 5 years ago showed that while nearly 50% of physicians “in principal” supported legislation to establish NHI, only 26% supported NHI with a single government payer that covers everyone (given only “yes” and “no” as response options)24. A recent update showed that support for NHI, not otherwise specified, has grown to 59% but opinions about single-payer financing of NHI were not assessed23. The 46% of physicians that support single payer NHI in our study is a significantly greater proportion than in the study of Ackerman et al.24 conducted 5 years earlier and may suggest that such support has grown. Because of the different wording of the questions used in these two surveys, however, definitive conclusions about changes in the level of such support are difficult to draw.
A plurality of respondents preferred the current system with the “addition of tax credits for buying, or tax penalties for failing to buy health insurance”. It is worth noting two points in interpreting this result. First, because of the complexity, and variability of each of these two reform approaches, we did not specify details of reform features that are often advocated as part of the tax credit approach (such as health savings accounts and deregulation of insurance markets) and the tax penalty approach (such as subsidies for the poor, expansion of existing public insurance programs, tighter regulation of insurance markets and sometimes, employer mandates) in this response option. This level of generality prevents us from drawing firm conclusions about potential differences in support for these specific reform features.
Second, while there are substantial differences between tax credit and tax penalty approaches, they are similar to the extent that they employ financial incentives to expand coverage within the existing employer-based, private insurance health care financing system. Because these were combined in a single response option, we interpret support for this option as support for either of these incremental approaches to reform compared with the more fundamental changes entailed in single-payer proposals or with no change (i.e., maintenance of the current system).
There are several potential reasons why a greater percentage of physicians indicated support for the use of financial incentives (tax credits or penalties) than for single-payer NHI. More physicians may simply believe in the greater effectiveness of incentive-based reform proposals to achieve increased coverage, decreased cost, improved quality and protect practice autonomy and compensation 8,29,30. Alternatively, physicians support for incentive-based reform options may be driven by the perception that they are more politically feasible and therefore more likely to result in the implementation of at least some health reform option, even if it may not be their first choice12. Our data do not allow us to determine the relative importance of these factors in determining physicians support for different reform options. As the level of physician support for single-payer NHI approaches that of its principal alternatives, it may be seen as a politically viable option as well.
Our finding that the belief that all Americans should receive needed medical care regardless of ability to pay was strongly associated with support for single-payer NHI is not surprising. Even among its detractors, single-payer NHI is widely believed to be more likely to achieve universal coverage than its principal alternatives. The majority in our sample do not believe that the uninsured have access to needed care and, again, it is not surprising that this belief was also associated with support for single payer NHI for the same reason. Hence, efforts to educate physicians about the limitations on access to care that are associated with being uninsured, such as those amply documented in the Institute of Medicine’s “Insuring Health” series31,32, might increase physician support for this option.
Physician support for single-payer NHI is somewhat lower than in public opinion polls which have consistently demonstrated majority support for NHI33,34 and, recently, single payer NHI in particular25. Although the majority of physicians in our survey believed that the uninsured lack access to needed care, one third did not. It is possible that physicians are more likely than the general public to believe that the uninsured can ultimately receive needed care for serious conditions though emergency departments and to equate this with access to needed care. Alternatively, physicians may simply be less willing to accept whatever trade-offs they may perceive (accurately or not) in implementing universal coverage (higher taxes, lower professional autonomy, etc.).
Our study has several limitations. First, our 50.8% response rate was modest, though typical for physician surveys. Although the non-respondents in this survey were very similar to our respondents, it is possible that physicians with a strong interest in health policy issues or strong views about reform options may have been more likely to respond. These physicians’ views may not be representative of all physicians.
Second, as with all surveys, question wording and response option content could have led to misinterpretation of question meaning or bias. In our question about support for health care financing reform (taken from a prior Kaiser / ABC News / CNN survey), the description of the current health care system in the “status quo” and “tax credit/penalty” response options was “in which most people get their insurance from private employers, but some have no insurance”. While few would disagree with the accuracy of this description, it is possible that the phrase “but some have no insurance” could overemphasize this negative attribute of the current system relative to the single-payer NHI response option which contained the phrase “in which everyone is covered”. However, the lack of access to health insurance in the current health care system has become a top issue on the minds of Americans nationally3 and is the key problem most reform proposals are designed to address. It seems unlikely, therefore, that the use of the phase “some have no insurance” to describe the current system would cause physicians who would otherwise support the status quo or incremental reform to change their response to support for single payer NHI, a fundamentally different approach.
Our survey showed that although a plurality of physicians favored incremental health care reform proposals based on the use of tax credits and penalties, a substantial proportion of physicians preferred an entirely different health care financing system–a government-run, taxpayer-financed single-payer NHI program. Physicians play a central role in the health care system and these views could be influential in reforming the financing of the American health care system.
References
DeNavas-Walt C, Proctor BD, Smith J. Income, Poverty, and Health Insurance Coverage in the United States: 2006. U.S. Census Bureau, Current Population Reports. Washington, DC: U.S. Government Printing Office, 2007.
Claxton G, Gabel J, DiJulio B, et al. Health benefits in 2007: premium increases fall to an eight-year low, while offer rates and enrollment remain stable. Health Aff (Millwood). 2007;26(5):1407–16.
Blendon RJ, Altman DE, Deane C, Benson JM, Brodie M, Buhr T. Health care in the 2008 presidential primaries. N Engl J Med. 2008;358(4):414–22.
Oberlander J. Presidential politics and the resurgence of health care reform. N Engl J Med. 2007;357(21):2101–4.
Commonwealth Fund website. An Analysis of Leading Congressional Health Care Bills, 2005–2007: PART I, Insurance Coverage. Sara R. Collins, Karen Davis, and Jennifer L. Kriss. March. 2007. Available at: http://www.commonwealthfund.org/usr_doc/Collins_conghltcarebillsinscoverage_1010.pdf?section=4039. Accessed December 31, 2008.
Schoen C, Davis K, Collins SR. Building blocks for reform: achieving universal coverage with private and public group health insurance. Health Aff (Millwood). 2008;27(3):646–57.
Halvorson GC, Crosson FJ, Zatkin S. A proposal to cover the uninsured in California. Health Aff (Millwood). 2007;26(1):w80–91.
Etheredge LM. Massachusetts reform plus President Bush’s tax credits: a national model? Health Aff (Millwood). 2006;25(6):w444–6.
National Governor’s Association Website. Leading the Way: State Health Reform Initiatives. July 11, 2007. Available at: http://www.nga.org/Files/pdf/0707HEALTHREFORM.PDF. Accessed December 31, 2008.
Himmelstein DU, Woolhandler S. A national health program for the United States: a physicians’ proposal. N Eng J Med. 1989;320:102–8.
Schiff GD, Bindman AB, Brennan TA. A better-quality alternative: single-payer national health system reform. JAMA. 1994;272:803–8.
Krugman P. Why not single-payer? New York Times 2007. Available at http://krugman.blogs.nytimes.com/2007/10/07/why-not-single-payer/. Accessed July 10, 2008.
Roper WL. Here we go again–lessons on health reform. Health Aff (Millwood). 2007;26(6):1551–2.
Hacker JS. Putting politics first. Health Aff (Millwood). 2008;27(3):718–23.
Antos J. Lessons from the Clinton plan: incremental market reform, not sweeping government control. Health Aff (Millwood). 2008;27(3):705–10.
Scanlan A, Zyzanski SJ, Flocke SA, Stange KC, Grava-Gubins I. A comparison of US and Canadian family physician attitudes toward their respective health-care systems. Med Care. 1996;34(8):837–44.
Simon SR, Pan RJ, Sullivan AM, et al. Views of managed care–a survey of students, residents, faculty, and deans at medical schools in the United States. N Engl J Med. 1999; 340(12):928–36.
Shearer S, Toedt M. Family physicians’ observations of their practice, well being, and health care in the United States. J Fam Pract. 2001;50:751–6.
Albers JM, Lathrop BP, Allison KC, Oberg CN, Hart JF. Single-payer, health savings accounts, or managed care? Minnesota physicians’ perspectives. Minn Med. 2007;90(2):36–40.
Millard PS, Konrad TR, Goldstein A, Stein J. Primary care physicians’ views on access and health care reform: the situation in North Carolina. J Fam Pract. 1993;37(5):439–44.
Malter AD, Emerson LL, Krieger JW. Attitudes of Washington State physicians toward health care reform. West J Med. 1994;161(1):29–33.
McCormick D, Himmelstein DU, Woolhandler S, Bor DH. Single-payer national health insurance. Physicians’ views. Arch Intern Med. 2004;164(3):300–4.
Carroll AE, Ackerman RT. Support for National Health Insurance among U.S. Physicians: 5 years later. Ann Intern Med. 2008;148(7):566–7.
Ackermann RT, Carroll AE. Support for national health insurance among U.S. physicians: a national survey. Ann Intern Med. 2003;139(10):795–801.
ABC News Website. Prescription for Change: Fixing American Health Care. October 16, 2006. Available at:http://abcnews.go.com/images/Politics/1021a1HealthCare.pdf. Accessed December 31, 2008.
U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau website. Census Regions and Divisions of the United States. September 19, 2007. Available at: http://www.census.gov/geo/www/us_regdiv.pdf. Accessed December 31, 2008.
United States Department of Agriculture Economic Research Service Website. Measuring rurality: rural-urban continuity codes. April 28, 2004. Available at:http://www.ers.usda.gov/briefing/rurality/ruralurbcon/. Accessed December 31, 2008.
SAS Software Version 9.1. Cary, NC: SAS Institute, 2007.
Palmisano DJ. Debating how to fix health insurance. Science. 2004;303(5663):1467–8. author reply 1467-8.
Oberlander J. Learning from failure in health care reform. N Engl J Med. 2007;357(17):1677–9.
Institute of Medicine. Committee on the Consequences of Uninsurance. Coverage Matters: Insurance and Health Care. Washington, DC: National Academies Press; 2001.
Institute of Medicine. Committee on the Consequences of Uninsurance. A Shared Destiny: Community effects of Underinsurance. Washington, DC: National Academies Press; 2003.
Blendon RJ, Benson JM. Americans’ views on health policy: a fifty-year historical perspective. Health Aff (Millwood). 2001;20(2):33–46.
Blendon RJ, Benson JM, DesRoches CM. Americans’ views of the uninsured: an era for hybrid proposals. Health Aff (Millwood). 2003;(Suppl Web Exclusives): W3-405-14.
Acknowledgements
Funding
The research was funded by internal funds of the Department of Medicine at the Cambridge Hospital.
Role of the sponsor
The sponsor had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, or preparation, review, or approval of the manuscript.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
McCormick, D., Woolhandler, S., Bose-Kolanu, A. et al. U.S. Physicians’ Views on Financing Options to Expand Health Insurance Coverage: A National Survey. J GEN INTERN MED 24, 526–531 (2009). https://doi.org/10.1007/s11606-009-0916-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-0916-x