Abstract
Background
Serious mental illness often is associated with an increased risk of diabetes and sub-optimal diabetes care.
Objective
To examine diabetes prevalence and care among Medicaid patients from one county mental health system.
Design
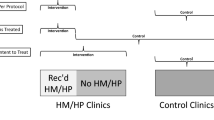
Retrospective cohort study combining county records and 12 months of state Medicaid claims.
Subjects
Patients ages 18 to 59 receiving mental health services between November 1 and 14, 2004.
Measurements
Dependent variables were glycolated hemoglobin A1C (HbA1c) testing, lipid testing, and eye examinations. Psychiatric status was assessed by second generation antipsychotic prescription (SGA) and low Global Assessment of Functioning (GAF) score.
Results
Among psychiatric patients, 482 (11.8%) had diabetes. Among those with diabetes, 47.3% received annual HbA1c testing, 56.0% lipid testing, and 31.7% eye examinations. Low GAF scores were associated with lower likelihood of lipid testing (OR 0.43). SGA prescription reduced the likelihood of HbA1c testing (OR 0.58) but increased the likelihood of eye examinations (OR 2.02). Primary care visits were positively associated with HbA1c and lipid testing (ORs 5.01 and 2.21, respectively). Patients seen by a fee-for-service psychiatrist were more likely to have lipid testing (OR 2.35) and eye examinations (OR 2.03).
Conclusion
Among Medicaid psychiatric patients, worse diabetes care was associated with SGA prescription, more serious psychiatric symptoms, and receiving psychiatric care only in public mental health clinics. Diabetes care improved when patients were seen by fee-for-service psychiatrists or primary care physicians. Further study is needed to identify methods for improving diabetes care of public mental health patients.
Similar content being viewed by others
References
Long SK, Coughlin TA, Kendall SJ. Access to care among disabled adults on Medicaid. Health Care Financ Rev. 2002;23:159–73.
Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis [serial online]. 2006. Available at: http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm. Accessed on April 20, 2008.
Weitoft GR, Gullberg A, Rosen M. Avoidable mortality among psychiatric patients. Soc Psychiatry Psychiatr Epidemiol. 1998;33:430–7.
Dixon L, Weiden P, Delahanty J, et al. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26:903–12.
Van Winkel R, De Hert M, Van Eyck D, et al. Prevalence of diabetes and the metabolic syndrome in a sample of patients with bipolar disorder. Bipolar Disord. 2008;10:342–8.
Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabetes Care. 2008;31:105–7.
Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(Suppl 1):20–7.
Guo JJ, Keck PEJ, Corey-Lisle PK, et al. Risk of diabetes mellitus associated with atypical antipsychotic use among Medicaid patients with bipolar disorder: A nested case-control study. Pharmacotherapy. 2007;27:27–35.
Morrato EH, Newcomer JW, Allen RR, Valuck RJ. Prevalence of baseline serum glucose and lipid testing in users of second-generation antipsychotic drugs: A retrospective, population-based study of Medicaid claims data. J Clin Psychiatry. 2008;69:316–22.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29:725–31.
Kilbourne AM, Welsh D, McCarthy JF, Post EP, Blow FC. Quality of care for cardiovascular disease-related conditions in patients with and without mental disorders. J Gen Intern Med. 2008;23:1628–33.
Frayne SM, Halanych JH, McDonald DR, et al. Disparities in diabetes care: Impact of mental illness. Arch Internal Med. 2005;165:2631–8.
Lin EHB, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60.
Krein SL, Bingham CR, McCarthy JF, Mitchinson A, Payes J, Valenstein M. Diabetes treatment among VA patients with comorbid serious mental illness. Psychiatr Serv. 2006;57:1016–21.
Whyte S, Penny C, Phelan M, Hippisley-Cox J, Majeed A. Quality of diabetes care in patients with schizophrenia and bipolar disorder: Cross-sectional study. Diabet Med. 2007;24:1442–8.
Rosenheck RA, Stolar M. Access to public mental health services: Determinants of population coverage. Med Care. 1998;36:503–12.
Piette JD. Perceived access problems among patients with diabetes in two public systems of care. J Gen Intern Med. 2000;15:797–804.
Sambamoorthi U, Olfson M, Wei W, Crystal S. Diabetes and depression care among Medicaid beneficiaries. J Health Care Poor Underserved. 2006;17:141–61.
Andersen RM, Davidson PL. Improving Access to Care in America: Individual and Contextual Indicators. In: Andersen RM, Rice TH, Kominski GF, eds. Changing the U.S. Health Care System. 3rd ed. San Francisco: Jossey-Bass; 2007:3–32.
Gelberg L, Andersen RM, Leake B. The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302.
Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41:275–87.
Harris K. Personal communication, email from San Bernardino County Department of Behavioral Health Research and Evaluation section, November 29, 2007.
Cunningham P, McKenzie K, Taylor EF. The struggle to provide community-based care to low-income people with serious mental illness. Health Aff (Millwood). 2006;25:694–705.
Tungstrom S, Soderberg P, Armelius BA. Relationship between the Global Assessment of Functioning and other DSM axes in routine clinical work. Psychiatr Serv. 2005;56:439–43.
Meduru P, Helmer D, Rajan M, Tseng C-L, Pogach L, Sambamoorthi U. Chronic illness with complexity: Implications for performance measurement of optimal glycemic control. J Gen Intern Med. 2007;22(Suppl 3):408–18.
Kerr EA, Heisler M, Krein SL, et al. Beyond comorbidity counts: How do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22:1635–40.
U.S. Department of Health and Human Services. Healthy People 2010. Available at: http://www.healthypeople.gov/Document/tableofcontents.htm#uih. Accessed on May 14, 2008.
Goldberg RW, Kreyenbuhl JA, Medoff DR, et al. Quality of diabetes care among adults with serious mental illness. Psychiatr Serv. 2007;58:536–43.
Saaddine JB, Cadwell B, Gregg EW, et al. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med. 2006;144:465–74.
Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry. 2004;161:1334–49.
Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2008.
Glazier RH, Bajcar J, Kennie NR, Wilson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29:1675–88.
Druss BG. Improving medical care for persons with serious mental illness: Challenges and solutions. J Clin Psychiatry. 2007;68(Supplement 4):40–4.
Koran LM, Sox HC, Marton KI, et al. Medical evaluation of psychiatric patients. Arch Gen Psychiatry. 1989;46:733–40.
Mayberg SW. California’s Community Mental Health Performance Outcome Report, Fiscal Year 2002–2003: California Department of Mental Health; March 2003.
Labby D, Spofford M, Robinson J, Ralston R. The economics of depression in primary care: Defragmentation in the Oregon Medicaid market. Adm Policy Ment Health. 2006;33:39–42.
Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289:434–41.
Rittenhouse DR, Robinson JC. Improving quality in Medicaid: The use of care management processes for chronic illness and preventive care. Med Care. 2006;44:47–54.
The California Medi-Cal Type 2 Diabetes Study Group. Closing the gap: Effect of diabetes case management on glycemic control among low-income ethnic minority populations. Diabetes Care. 2004;27:95–103.
Grazier KL, Hegedus AM, Carli T, Neal D, Reynolds K. Integration of behavioral and physical health care for a Medicaid population through a public-public partnership. Psychiatr Serv. 2003;54:1508–12.
Klein J. Use of Medi-Cal managed care encounter data for research purposes. Sacramento, CA: California Department of Health Services; January, 2002.
Salsberry PJ, Chipps E, Kennedy C. Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatr Serv. 2005;56:458–62.
Moos RH, Nichol AC, Moos BS. Global Assessment of Functioning ratings and the allocation and outcomes of mental health services. Psychiatr Serv. 2002;53:730–7.
Frank RG, Glied S. Changes in mental health financing since 1971: Implications for policymakers and patients. Health Aff (Millwood). 2006;25:601–13.
Acknowledgements
This research was supported, in part, by a seed grant from the Loma Linda University School of Public Health Center for Health Research.
Conflict of Interest
None of the authors, Jim E. Banta, Elaine H. Morrato, Scott W. Lee, and Mark G. Haviland report a conflict of interest. There was no external funding; the internal seed grant was used to purchase the state Medicaid data. None of the authors receives funding directly from either the State Department of Health Services or the County of San Bernardino.
Author information
Authors and Affiliations
Corresponding author
Additional information
Portions of this work were presented June 2007 at the AcademyHealth Annual Research Meeting in Orlando, Florida and November 2007 at the American Public Health Association’s 135th Annual Meeting, in Washington, DC. (PowerPoint file for the latter posted on APHA website.)
Partial funding for this project was provided by a seed grant from the Loma Linda University School of Public Health Center for Health Research.
Rights and permissions
About this article
Cite this article
Banta, J.E., Morrato, E.H., Lee, S.W. et al. Retrospective Analysis of Diabetes Care in California Medicaid Patients with Mental Illness. J GEN INTERN MED 24, 802–808 (2009). https://doi.org/10.1007/s11606-009-0994-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-0994-9