ABSTRACT
BACKGROUND
Teaching hospitals increasingly rely on transfers of patient care to another physician (hand-offs) to comply with duty hour restrictions. Little is known about the impact of hand-offs on medical students.
OBJECTIVE
To evaluate the impact of hand-offs on the types of patients students see and the association with their subsequent Medicine Subject Exam performance.
DESIGN
Observational study over 1 year.
PARTICIPANTS
Third-year medical students in an Inpatient Medicine Clerkship at five hospitals with night float systems.
MEASUREMENTS
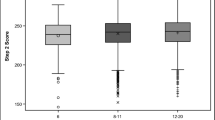
Primary outcome: Medicine Subject Exam at the end of the clerkship; explanatory variables: number of fresh (without prior evaluation) and hand-off patients, diagnoses, subspecialty patients, and full evaluations performed during the clerkship, and United Stated Medical Licensing Examination (USMLE) Step I scores.
MAIN RESULTS
Of the 2,288 patients followed by 89 students, 990 (43.3%) were hand-offs. In a linear regression model, the only variables significantly associated with students’ Subject Exam percentile rankings were USMLE Step I scores (B = 0.26, P < 0.001) and the number of full evaluations completed on fresh patients (B =0.20, P = 0.048; model r 2 = 0.58). In other words, for each additional fresh patient evaluated, Subject Exam percentile rankings increased 0.2 points. For students in the highest quartile of Subject Exam percentile rankings, only Step I scores showed a significant association (B = 0.22, P = 0.002; r 2 = 0.5). For students in the lowest quartile, only fresh patient evaluations demonstrated a significant association (B = 0.27, P = 0.03; r 2 = 0.34).
CONCLUSIONS
Hand-offs constitute a substantial portion of students’ patients and may have less educational value than “fresh” patients, especially for lower performing students.
Similar content being viewed by others
References
Accreditation Council for Graduate Medical Education. Common Program Requirements. Available at: http://www.acgme.org/acwebsite/dutyhours/dh_lang703.pdf; Accessed May 29, 2009.
Vidyarthi AR, Katz PP, Wall SD, Wachter RM, Auerbach AD. Impact of reduced duty hours on residents’ educational satisfaction at the University of California, San Francisco. Acad Med. 2006;81(1):76–81.
Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: Strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257–66.
Goldstein MJ, Kim E, Widmann WD, Hardy MA. A 360˚ evaluation of a night-float system for general surgery: A response to mandated work-hours reduction. Curr Surg. 2004;61(5):445–51.
Wallach SL, Alam K, Diaz N, Shine D. How do internal medicine residency programs evaluate their resident float experiences? South Med J. 2006;99(9):919–23.
Peterson LE, Johnson H, Pugno PA, Bazemore A, Phillips RL. Training on the clock: Family medicine residency directors’ responses to resident duty hours reform. Acad Med. 2006;81(12):1032–7.
Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between staff on internal medicine wards. Arch Intern Med. 2006;166:1173–7.
Fletcher K, Saint S, Mangrulkar RS. Balancing continuity of care with residents’ limited work hours: Defining the implications. Acad Med. 2005;80(1):39–43.
Kogan JR, Pinto-Powell R, Brown LA, Hemmer P, Bellini LM, Peltier D. The impact of resident duty hours reform on the internal medicine core clerkship: Results from the Clerkship Directors in Internal Medicine survey. Acad Med. 2006;81(12):1038–44.
Nixon LJ, Benson BJ, Rogers T, Sick BT, Miller WJ. Effects of Accreditation Council for Graduate Medical Education work restrictions on medical student experience. J Gen Intern Med. 2007;22:937–41.
Kogan JR, Bellini LM, Shea JA. The impact of resident duty hour reform in a medicine core clerkship. Acad Med. 2004;79(10S):S58–61.
White CB, Haftel HM, Purkiss JA, Schigelone AS, Hammoud MM. Multidimensional effects of the 80-hour work week at the University of Michigan Medical School. Acad Med. 2006;81(1):57–62.
Jagsi R, Shapiro J, Weinstein DF. Perceived impact of resident work hour limitations on medical student clerkships: A survey study. Acad Med. 2005;80(8):752–7.
Norman G. Building on experience: The development of clinical reasoning. N Engl J Med. 2006;335(21):2251–2.
Bowen J. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;335(21):2217–25.
Defer TM, Fazio SB. Clerkship Directors in Internal Medicine-Society of General Internal Medicine. Core medicine clerkship curriculum guide: A resource for teachers and learners, version 3.0. Available at: http://www.im.org/Resources/Education/Students/Learning/Pages/CDIM-SGIMCoreMedicineClerkshipCurriculum.aspx. Accessed May 29, 2009.
National Board of Medical Examiners. Subject Examination Program Information Guide. 2007; p. 9. Available at: http://www.nbme.org/PDF/2007subexaminfoguide.pdf. Accessed May 29, 2009.
Griffth CH III, Wilson JF, Haist SA, Ramsbottom-Lucier M. Do students who work with better housestaff in their medicine clerkships learn more? Acad Med. 1998;73(10):S57–9.
Griffith CH III, Wilson JF, Haist SA, Ramsbottom-Lucier M. Relationships of how well attending physicians teach to their students’ performances and residency choices. Acad Med. 1997;72(10):S118–20.
Acknowledgements
The authors acknowledge Kevin R. McCormick, MD (Highland Hospital), Walter Polashenski, MD (Rochester General Hospital), Philip Bonanni, MD (Unity Health), and Alan Kozak, MD (Mary Imogene Bassett Hospital) for their contributions to the data collection. There was no funding for this study.
Funding
None.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
An abstract from this paper was presented at the Clerkship Directors in Internal Medicine National Conference in October 2007 and is published in the proceedings of that conference.
Rights and permissions
About this article
Cite this article
Lang, V.J., Mooney, C.J., O’Connor, A.B. et al. Association Between Hand-off Patients and Subject Exam Performance in Medicine Clerkship Students. J GEN INTERN MED 24, 1018–1022 (2009). https://doi.org/10.1007/s11606-009-1045-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1045-2