Abstract
BACKGROUND
This study seeks to determine whether antihypertensive medication refill adherence, ambulatory visits, and type of antihypertensive medication exposures are associated with decreased stroke and death for community-dwelling hypertensive patients.
METHODS
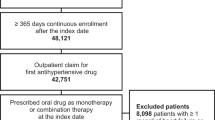
This retrospective cohort study included all chronic medication-treated hypertensives enrolled in Tennessee’s Medicaid program (TennCare) for 3–7 years during the period 1994–2000 (n = 49,479). Health care utilization patterns were evaluated using administrative data linked to vital records during a 2-year run-in period and 1- to 5-year follow-up period. Antihypertensive medication refill adherence was calculated using pharmacy records.
RESULTS
Associations with stroke and death were assessed using Cox proportional hazards modeling. Stroke occurred in 619 patients (1.25%) and death in 2,051 (4.15%). Baseline antihypertensive medication refill adherence was associated with decreased multivariate hazards of stroke [hazard ratio (HR) 0.91; 95% confidence interval (CI), 0.86–0.97 for 15% increase in adherence]. Adherence in the follow-up period was associated with decreased hazards of stroke (HR 0.92; CI 0.87–0.96) and death (HR 0.93; CI 0.90–0.96). Baseline ambulatory visits were associated with decreased death (HR 0.99; CI 0.98–1.00). Four major classes of antihypertensive agents were associated with mortality reduction. Only thiazide-type diuretic use was associated with decreased stroke (HR 0.89; CI 0.85–0.93).
CONCLUSIONS
Ambulatory visits and antihypertensive medication exposures are associated with reduced mortality. Increasing adherence by one pill per week for a once-a-day regimen reduces the hazard of stroke by 8–9% and death by 7%.

Similar content being viewed by others
References
Steiner JF, Koepsell TD, Fihn SD, Inui TS. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med Care. 1988;26(8):814–23.
Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40(7–8):1280–8.
Bailey JE, Lee MD, Somes GW, Graham RL. Risk factors for antihypertensive medication refill failure by patients under Medicaid managed care. Clin Ther. 1996;18(6):1252–62.
Choo PW, Rand CS, Inui TS, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37(9):846–57.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–30.
Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004;55(8):886–91.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med Care. 2008;46(11):1125–33.
Wetzels GE, Nelemans P, Schouten JS, Prins MH. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;22(10):1849–55.
Richter A, Anton SE, Koch P, Dennett SL. The impact of reducing dose frequency on health outcomes. Clin Ther. 2003;25(8):2307–35. discussion 6.
Kettani FZ, Dragomir A, Cote R, et al. Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke. 2009;40(1):213–20.
Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–7.
Ma J, Stafford RS. Screening, treatment, and control of hypertension in US private physician offices, 2003–2004. Hypertension. 2008;51(5):1275–81.
Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–98.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT). JAMA. 2002;288(23):2998–3007.
Connor J, Rafter N, Rodgers A. Do fixed-dose combination pills or unit-of-use packaging improve adherence? A systematic review. Bull World Health Organ. 2004;82(12):935–9.
Tang J, Wan JY, Bailey JE. Performance of comorbidity measures to predict stroke and death in a community-dwelling, hypertensive Medicaid population. Stroke. 2008;39(7):1938–44.
Ray WA. Policy and program analysis using administrative databases. Ann Intern Med. 1997;127(8 Pt 2):712–8.
Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30(4):736–43.
Benesch C, Witter DM Jr, Wilder AL, Duncan PW, Samsa GP, Matchar DB. Inaccuracy of the International Classification of Diseases (ICD-9-CM) in identifying the diagnosis of ischemic cerebrovascular disease. Neurology. 1997;49(3):660–4.
Leibson CL, Naessens JM, Brown RD, Whisnant JP. Accuracy of hospital discharge abstracts for identifying stroke. Stroke. 1994;25(12):2348–55.
Reker DM, Hamilton BB, Duncan PW, Yeh SC, Rosen A. Stroke: who’s counting what? J Rehabil Res Dev. 2001;38(2):281–9.
Marini C, Baldassarre M, Russo T, et al. Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology. 2004;62(1):77–81.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52.
Gil-Nunez AC, Vivancos-Mora J. Blood pressure as a risk factor for stroke and the impact of antihypertensive treatment. Cerebrovasc Dis. 2005;20(Suppl 2):40–52.
Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50(1):105–16.
Allison PD. Survival Analysis Using SAS: A Practical Guide. Cary: SAS Institute, Inc; 1995.
SAS Institute. Statistical Analysis System (SAS). In. 9.1 ed. Cary, NC; 2003.
Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165(10):1147–52.
Zhang X, Loberiza FR, Klein JP, Zhang MJ. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Methods Programs Biomed. 2007;88(2):95–101.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Amer Statist Assoc. 1958;53:457–81.
Vey N, Blaise D, Stoppa AM, et al. Bone marrow transplantation in 63 adult patients with acute lymphoblastic leukemia in first complete remission. Bone Marrow Transplant. 1994;14(3):383–8.
Xie J, Liu C. Adjusted Kaplan-Meier estimator and log-rank test with inverse probability of treatment weighting for survival data. Stat Med. 2005;24(20):3089–110.
Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120(1):26–32.
Elliott WJ, Plauschinat CA, Skrepnek GH, Gause D. Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med. 2007;20(1):72–80.
Therapeutics Initiative: Evidence Based Drug Therapy. Do Statins have a role in primary prevention? In: Therapeutics Letter; 2003.
Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75.
Gu Q, Burt VL, Paulose-Ram R, Yoon S, Gillum RF. High blood pressure and cardiovascular disease mortality risk among US adults: the third National Health and Nutrition Examination Survey mortality follow-up study. Ann Epidemiol. 2008;18(4):302–9.
Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527–35.
Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289(19):2534–44.
Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–98.
Stroupe KT, Teal EY, Tu W, Weiner M, Murray MD. Association of refill adherence and health care use among adults with hypertension in an urban health care system. Pharmacotherapy. 2006;26(6):779–89.
Thorpe CT, Bryson CL, Maciejewski ML, Bosworth HB. Medication acquisition and self-reported adherence in veterans with hypertension. Med Care. 2009;47(4):474–81.
Acknowledgments
This research was supported by a grant from the American Heart Association. The authors gratefully acknowledge the assistance of the TennCare Bureau of the State of Tennessee, Catherine Lewis and Deborah Gibson for their substantial editorial assistance, Grant Somes, PhD, and Andy Bush, PhD, for their assistance with the study design and analysis plan, and William Pulsinelli, MD, for contributing his advice and content expertise on the design and implementation of the study.
Conflicts of Interest
Dr. James Bailey has received a grant from Novo Nordisk, Inc., for reporting on diabetes quality of care, 2006–2008.
Jun Tang has been employed by Accredo Health Group, Inc., since 2007.
Dr. William Cushman has consulted for Sanofi-Aventis, Bristol-Myers Squibb, Novartis, Pfizer, Daiichi Sankyo, Forest, King Pharmaceuticals, Boehringer-Ingelheim, Roche, Takeda, Sciele, Pharmacopeia, and Gilead. He has received grants from Astra-Zeneca, Sanofi-Aventis, King, GlaxoSmithKline, and Novartis. He has a grant request pending with GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Additional information
Data for this study were also used in the following
Poster presentation. Academy Health, Washington DC, June 9, 2008. Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence protects community dwelling hypertensive people from strokes and death.
Tang, J, Wan, JY, and Bailey, JE. Performance of comorbidity measures to predict stroke and death in a community-dwelling, hypertensive Medicaid population. Stroke 2008;39:1938–1944.
This research was supported by a grant from the American Heart Association.
Rights and permissions
About this article
Cite this article
Bailey, J.E., Wan, J.Y., Tang, J. et al. Antihypertensive Medication Adherence, Ambulatory Visits, and Risk of Stroke and Death. J GEN INTERN MED 25, 495–503 (2010). https://doi.org/10.1007/s11606-009-1240-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1240-1