Abstract
BACKGROUND
Chronic hepatitis B and hepatitis B-associated liver cancer is a major health disparity among Vietnamese Americans, who have a chronic hepatitis B prevalence rate of 7–14% and an incidence rate for liver cancer six times that of non-Latino whites.
OBJECTIVE
Describe factors associated with hepatitis B testing among Vietnamese Americans.
DESIGN
A population-based telephone survey conducted in 2007–2008.
PARTICIPANTS
Vietnamese Americans age 18–64 and living in the Northern California and Washington, DC areas (N = 1,704).
MAIN MEASURES
Variables included self-reports of sociodemographics, health care factors, and hepatitis B-related behaviors, knowledge, beliefs, and communication with others. The main outcome variable was self-reported receipt of hepatitis B testing.
KEY RESULTS
The cooperation rate was 63.1% and the response rate was 27.4%. Only 62% of respondents reported having received a hepatitis B test and 26%, hepatitis B vaccination. Only 54% knew that hepatitis B could be transmitted by sexual intercourse. In multivariable analyses, factors negatively associated with testing included: age 30–49 years, US residence for >10 years, less Vietnamese fluency, lower income, and believing that hepatitis B can be deadly. Factors positively associated with testing included: Northern California residence, having had hepatitis B vaccination, having discussed hepatitis B with family/friends, and employer requested testing. Physician recommendation of hepatitis B testing (OR 4.46, 95% CI 3.36, 5.93) and respondent's request for hepatitis B testing (OR 8.37, 95% CI 5.95, 11.78) were strongly associated with test receipt.
CONCLUSION
Self-reports of hepatitis B testing among Vietnamese Americans remain unacceptably low. Physician recommendation and patient request were the factors most strongly associated with test receipt. A comprehensive effort is needed to promote hepatitis B testing in this population, including culturally-targeted community outreach, increased access to testing, and physician education.
Similar content being viewed by others
INTRODUCTION
An estimated 350 million people worldwide are infected chronically with the hepatitis B virus (HBV), a leading preventable cause of death.1 Approximately 1.4 million Americans have chronic hepatitis B, and the prevalence will likely increase due to immigration from endemic areas.2 Since chronic hepatitis B is often asymptomatic, many infected people do not know they have it. Early diagnosis through blood tests is crucial, because it can lead to treatment (antiviral medications) and preventive measures (e.g., avoidance of alcohol and other liver toxins, vaccination for hepatitis A, and possibly screening for liver cancer) along with prevention of transmission by vaccination of contacts.3,4 Guidelines recommend that people born in endemic areas and US–born persons not vaccinated as infants whose parents were born in endemic regions be screened using blood tests for hepatitis B surface antigen (HBsAg) and surface antibody (anti-HBs).5
In the US, a majority of those with chronic hepatitis B are Asians.6 Among Asians, infection usually occurs in childhood, a pattern that leads to the development of liver cancer at an early age.7,8 HBV accounted for 80% of the liver cancer cases among Asian Americans.8 HBV testing among Asian and Pacific Islander adults is cost-effective, with an estimated incremental cost-effectiveness ratio of $36,088 per quality-adjusted life-years (QALY) for a screen-and-treat strategy and of $39,903 per QALY for a strategy of screening, treating those infected, and vaccination of close contacts. However, two-thirds of Asian Americans chronically infected with HBV are unaware of it.9
Vietnamese Americans are the second fastest growing Asian group, with a population over 1.25 million. 10,11 They face significant health barriers, including limited access and lack of health knowledge.12 Vietnamese Americans have a prevalence rate of chronic hepatitis B ranging from 7 to 14%.9,13-15 Liver cancer is the second leading cause of cancer deaths for Vietnamese Americans, second only to lung; the incidence rate of liver cancer is six times that of non-Latino whites.16
The largest populations of Vietnamese Americans are in California, Texas, Greater Washington DC/Maryland/Virginia, and Seattle/King County, WA.17 This article reports the results of a baseline telephone survey about HBV in population-based samples of Vietnamese Americans living in the San Francisco/San Jose metropolitan areas of Northern California (Vietnamese population 165,402) and the Greater Washington, DC/Maryland/Virginia metropolitan area (Vietnamese population 58,020) in 2007-2008.17 The goal was to describe HBV beliefs, knowledge, and testing behaviors across two large Vietnamese communities as part of the planning for a community-wide intervention program.
METHODS
Study Design
A population-based telephone survey was conducted in 2007-2008. Using a list of 55 Vietnamese surnames, an established method to obtain a representative sample of this population,18-20 a simple random sample of 10,150 numbers in telephone directories in Northern California and the Greater Washington, DC metropolitan areas was compiled. Survey eligibility criteria included: age 18 to 64, resident of either area, able to respond in Vietnamese or English, and self-identified as Vietnamese, Vietnamese American, or Chinese-Vietnamese. The Institutional Review Boards of the University of California, San Francisco and San Francisco State University (SFSU) approved the study protocols.
Response and Cooperation Rates
To assess eligibility, each number was called up to 15 times from 10 AM–9 PM Mondays-Saturdays. For each eligible number, unless there was a refusal, up to 33 calls were attempted in order to complete a survey. Of the 10,150 numbers, 3,139 (30.9%) were not eligible (11.3% non-working numbers, 5.5% not ethnically eligible, 5.5% not age eligible, 3.6% not language eligible, 4.1% business/government numbers, and 0.9% not in study area/other); 2,535 (25.0%) could not be assessed for eligibility (18.0% despite maximum number of call attempts, 5.7% hard refusals, and 1.3% on “never call” lists). There were 4,476 (44.1%) eligible numbers, among which 998 (9.8%) refused to participate, 1,774 (17.5%) neither refused nor completed survey while not at the maximum call attempts, and 1,704 (16.8%) completed the survey. The rates were similar for Northern California and Washington D.C., except that Washington D.C. had more telephone numbers that could not be assessed for eligibility despite 15 call attempts (1,529 vs. 295) while Northern California had more eligible households that neither refused nor completed the survey while not at the maximum call attempt (1,596 vs. 178).
The overall cooperation rate (number of completed interviews divided by number of eligibles and excluding those eligible but unable to be reached) was 63.1% (65.5% for Northern California and 60.7% for DC). Using the American Association for Public Opinion Research Response Rate 4 formula,21 the response rates were 27.4% overall, 25.8% for Northern California, and 29.3% for DC.
Survey Development and Administration
A 24-minute computer-assisted telephone interviewing (CATI) survey was developed in English by using previously tested instruments along with research team and focus group input. The survey was translated into Vietnamese, back-translated into English, and pilot-tested with 26 participants. Between October 2007 and February 2008, 18 bilingual interviewers at the Public Research Institute at San Francisco State University administered the final survey in the respondent’s language of choice (Vietnamese or English). Interviewers were trained to conduct the structured CATI survey in a standardized manner; they could call either region at any time and were monitored randomly for quality control.
Survey Measures and Variables
Measures were developed using the Health Behavior Framework (HBF), which represents a synthesis of some of the major theoretical formulations in the area of health behavior.22,23 Demographic factors included: geographic area, age, sex, highest level of education, annual household income, employment, marital status, birthplace, years in the US, and how well the respondent spoke Vietnamese. Birthplace was combined with length of US residence due to the small number (2.3%) who were born in the US, who were then categorized as having lived in the US for >10 years. Health and health care variables included: family history of hepatitis B, having a regular physician, ethnicity of regular physician, and health insurance status.
Individual HBF constructs included knowledge, beliefs, and communication regarding HBV testing. Eight questions concerned knowledge of HBV transmission: three incorrect modes (smoking cigarettes; sharing food, drink, or eating utensils; sneezing or coughing) and four correct modes (sexual intercourse; sharing or reusing needles; during childbirth; sharing toothbrushes), as well as the fact that an infected person who looks and feels healthy could spread the disease. The “transmission knowledge” score consisted of the number of correct answers (range 0–8). Perceived severity questions asked whether respondents thought that persons with HBV could be infected for life, if HBV could cause cancer, if someone could die from HBV, and if HBV could be treated. Stigma, a cultural factor, was measured by asking if people avoided HBV-infected persons. Questions about communication with others asked whether respondents had discussed HBV with their friends or family, if their physician had recommended they be tested, if their employer had asked they be tested, and if the respondent had asked to be tested. The outcome measure of hepatitis B test receipt was defined as a “Yes” response to: “Have you ever had a blood test to check for hepatitis B?”
Statistical Analysis
First, the two geographic areas were compared regarding all variables specified above using t-tests for continuous variables and chi-square tests for categorical variables. Then, a logistic regression model was employed to assess the relative contribution of HBF constructs in explaining variation in test receipt. The independent variables included: demographics and health care variables; transmission knowledge score, perceived severity, cultural factors, and hepatitis B-related communication with others. Initially both English and Vietnamese fluency were included as covariates, but English fluency was dropped from the models because it was not associated with test receipt. Statistical significance was assessed at the 0.05 level. Data were analyzed using SAS version 9.2 (SAS Institute, 2007).
RESULTS
Table 1 shows the sociodemographics of the 1,704 respondents by geographic areas. The mean age was 45.9 years (Standard Deviation [SD] =11.2); 56% were females. Most (98%) were foreign-born, with 80% having been US residents for >10 years; 72% spoke Vietnamese fluently. Nearly 85% had health insurance, and 71%, a regular physician. Compared to Northern California respondents, DC respondents were more likely to be male, highly educated, employed, and to have a higher income and a regular physician.
Hepatitis B-related beliefs, knowledge, and behaviors for the entire sample are shown in Table 2. Of all respondents, 17.7% reported a family history of hepatitis B and 61.6% reported having had a hepatitis B test. Among those who reported having received a test, 4.5% reported that they still had HBV, 67.6% reported they did not have it, 16.3% reported they were immune to it, 4.5% reported that they had it but were no longer infectious, and 7.1% did not know their results.
Only 26.5% had been vaccinated against hepatitis B. Most (91.8%) believed that hepatitis B can be fatal. Few (14.6%) believed that it was untreatable, and 38.7% thought that people avoided those infected with hepatitis B. Half (52.7%) knew that HBV infection could be lifelong, and most knew that it could cause cancer (81.1%). Knowledge about some correct modes of transmission was moderate to high: 84.6% knew about sharing needles; 68.2%, about sharing toothbrushes; and 77%, about childbirth. However, only 54.3% knew about sexual intercourse as a mode of transmission. Knowledge about the incorrect modes of transmission was less, with 46.7% knowing that HBV was not acquired by smoking cigarettes, 47.8%, not from someone who sneezes, and 32.8%, not from sharing food or eating utensils. Two-thirds (68.8%) knew that someone who appeared healthy could transmit HBV. The mean knowledge score (range 0-8) was 4.8 (SD = 1.7). Approximately 45% reported having discussed hepatitis B with their family members or friends, 40% reported their physicians recommended testing, and 36% reported asking their physicians for testing.
Northern California respondents were more likely than DC respondents to report having had a family history of HBV (20.6% vs. 14.8%, p < 0.01) and having had a hepatitis B test (65.3% vs. 57.7%, p < 0.01) but not for hepatitis B vaccination (26.9% vs. 26.0%, p = 0.75). There were no differences in beliefs and knowledge, except Northern California respondents were slightly more likely to think that people avoided those who had hepatitis B (41.1% vs. 36.3%, p = 0.04) and less likely to know that HBV cannot be transmitted by smoking cigarettes (43.6% vs. 49.8%, p = 0.01). More Northern California than DC respondents reported that their physicians had recommended testing (44.9% vs. 35.8%, p < 0.01), and that they had asked their physicians for testing (39.4% vs. 33.0%, p < 0.01).
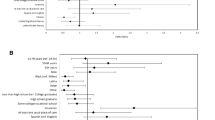
Table 3 shows the multivariable model for hepatitis B test receipt among all respondents. Sociodemographic factors significantly associated with self-report of hepatitis B testing included being in Northern California (Odds Ratio [OR] 1.37, 95% Confidence Interval [CI] 1.05, 1.77), aged 30-49 (OR 0.68, CI 0.52, 0.90), speaking Vietnamese less than fluently (OR 0.68, CI 0.51, 0.90), having lived in the US >10 years (OR 0.66, CI 0.47, 0.93). Those reporting a lower household income were less likely to report hepatitis B testing. Sex, marital status, and education were not associated with testing. Among health and health care variables, only reporting a hepatitis B vaccination was associated with testing (OR 1.86, CI 1.35, 2.55).
One belief about HBV was associated with testing—those who believed that people could die from HBV were less likely to have been tested (OR 0.47, CI 0.30, 0.75). Knowledge variables were not associated with testing; transmission knowledge score had a borderline significant association (OR 1.05, CI 0.97, 1.14). In an exploratory model that did not include the communication variables (data not shown), transmission knowledge score was associated with testing (OR 1.15, CI 1.07, 1.23). When we added the communication variables successively, the transmission knowledge score remained significant until respondent request for hepatitis B testing was added.
In the full model in Table 3, those who had discussed hepatitis B testing with family or friends (OR 1.34, CI 1.01, 1.78) and those whose employer had requested that they be tested (OR 2.05, CI 1.09, 3.87) were more likely to have had testing. Physician recommendation for hepatitis B testing was strongly associated with test receipt (OR 4.46, CI 3.36, 5.93). Respondent request for hepatitis B testing was also strongly associated with test receipt (OR 8.37, CI 5.95, 11.78).
DISCUSSION
This study shows that the rate of self-reported hepatitis B testing among Vietnamese Americans is low at 62%. Factors related to lack of testing in multivariable analysis included living in the DC area, age 30–49 years, having lived in the US for >10 years, speaking Vietnamese less than fluently, having a lower household income, and thinking that HBV can be deadly. Factors most strongly associated with testing were physician recommendation and respondent request for it.
The reported testing rate of 62% is comparable to two population-based face-to-face surveys in Seattle (64% among 345 Vietnamese men and 68% among 370 Vietnamese women).24,25 A population-based study conducted in 2006 of 1,696 Vietnamese Americans in King County, WA, three counties in CA (Los Angeles, Orange, and Santa Clara) and Lowell, MA reported a testing rate of 62.6%.26 These studies also used self-reports, though the validity of such self-reports is unknown. Among Chinese Americans, self-reports of hepatitis B testing may be unreliable 27. Self-reports may lead to over-reporting due to respondents’ confusing hepatitis B testing with tuberculosis (TB) testing (because of the use of the letter “B”) or, confusing it with other routine blood tests (such as liver function, diabetes, or cholesterol tests), or having a heath care provider order an incorrect screening test (i.e., not ordering HBsAg). Self-reports may lead to under-reporting due to respondents’ having been tested for hepatitis B but not being informed of results, or not remembering the testing. However, unless under-reporting is more common than over-reporting, based on the similar rates in this study and the other three population-based studies, up to two-thirds of Vietnamese Americans reported having received a hepatitis B screening test.
Knowledge of modes of transmission was high for sharing needles and childbirth, moderate for sharing toothbrushes, but low for sexual intercourse. Given the high prevalence of HBV in this population and the high infectivity, the limited knowledge about modes of transmission, particularly for sexual intercourse, is concerning. In addition, a majority of respondents in this and other studies thought incorrectly that food or respiratory droplets could spread HBV; they may undertake the wrong preventive behaviors. The rate of hepatitis B vaccination receipt was disappointingly low at 26%; a 2006 study also documented a low vaccination rate (36%).26 Thus, prevention of hepatitis B transmission remains a priority in this population, with a need for better education about safer sex and better vaccination coverage.
In multivariable analyses, those who lived in the US for >10 years and those who spoke Vietnamese less than fluently were less likely to have had hepatitis B testing. This seems surprising since recent Vietnamese immigrants are less likely to receive other preventive services.28,29 It is unlikely that they were tested in Vietnam since efforts to control HBV there have been focused on infant vaccination (started only in 2003) and there is no coordinated testing program.30 One possible explanation may be that efforts to promote testing and vaccination in the US have focused on more recent immigrants. Since 1996, US immigration laws have required hepatitis B vaccination for those applying for immigration to the US.31 Although this requirement does not apply to refugees at entry, it does apply to those adjusting their status to permanent residence. In addition, recent immigrants may be receiving medical care in immigrant and/or refugee clinics, where the providers may be more aware of the need for hepatitis B testing in this population.
Knowledge of transmission was associated with hepatitis B testing in exploratory models but not when respondents' request for the test was added. This suggests that those with the most knowledge about transmission were more likely to request the test. The only belief that was significant was the belief that hepatitis B can be deadly, and it was associated with lack of testing. This is the opposite of what has been found in other studies of Asian Americans.24,32,33 Further research is needed to understand if this question is a measure of fatalism or perceived severity and if such constructs work differently among different Asian populations.
Having health insurance or a regular doctor was not associated with hepatitis B testing, but physician recommendation was strongly associated with testing, a finding similar to prior studies among Vietnamese and other Asian American groups.24,25,32,34 This indicate that having access to health care is not sufficient; having a physician who is informed enough to offer hepatitis B testing is crucial. The factor most strongly associated with hepatitis B testing was respondent request for it, a finding that was found among Chinese Americans in Seattle; the association of request with receipt has been found for other preventive services among Vietnamese Americans.34-36 Informing Vietnamese Americans about hepatitis B and empowering them to ask their physician for the test through a media campaign may be one way to increase the rate of hepatitis B testing. Another potential intervention would be to educate physicians about the need for hepatitis B testing and how to offer the test in a culturally appropriate manner to this patient population. These findings and recommendations are consistent with the conclusions and recommendations made by the Institute of Medicine in its recent report on hepatitis B.2
In addition to self-reporting, this study has several limitations. Survey questions do not clarify if testing was performed in the US or elsewhere (though the primary goal of this baseline study was to identify factors associated with non-receipt of testing). It is a cross-sectional study and thus no causal inferences can be made. The use of telephone (landline) surveys potentially limits the generalizability of the study findings. There has been no study conducted on differences between Vietnamese Americans who do not have landlines compared to those who do. Other limitations to generalizability are the limited response rates and the fact that characteristics of non-respondents were not assessed. Low response rates do raise questions of non-respondent bias. Response rates to community-wide telephone surveys have been declining, and the response rates in this study is comparable to studies such as the California Health Interview Survey (26.9% in 2005 and 18.7% in 2007) and the Behavioral Risk Factor Surveillance System Survey (24.1% for California, 19.9% for DC in 2007).37,38 Nonetheless, this study was a population-based survey of two major population centers of Vietnamese in America, and the findings may be more generalizable than other studies limited to a single area. Limited comparisons to the 2000 Census data for the Vietnamese in the US show that the sample had a higher proportion of women and higher educational level but similar in proportion of those who were foreign-born and in household income.
There is general consensus that there is a need for innovative and effective outreach programs to target at-risk populations about hepatitis B.2 However, the literature on effective outreach interventions to promote hepatitis B testing among Asian Americans remains sparse.39 We have previously shown in controlled trials among Vietnamese Americans that culturally targeted health education can improve receipt of screening tests such as the Pap test and mammography 29,40-43 and receipt of hepatitis B vaccination among children.44 The low rate of hepatitis B testing reported by Vietnamese American adults in this study reinforces the need for interventions to educate this population about hepatitis B, including its transmission, testing and vaccination,39,45 and to educate their physicians about the importance of offering hepatitis B testing to this population. Such efforts are currently being implemented,22,23,39 and the findings of from this study will help to create effective interventions to reduce the burden of hepatitis B among Asian Americans.
References
Weiss RA, McMichael AJ. Social and environmental risk factors in the emergence of infectious diseases. Nat Med. 2004;10(12 Suppl):S70–6.
Institute of Medicine. Hepatitis and liver cancer: a national strategy for prevention and control of hepatitis B and C. Washington, DC: The National Academies Press; 2010.
Kemp W, Pianko S, Nguyen S, Bailey MJ, Roberts SK. Survival in hepatocellular carcinoma: impact of screening and etiology of liver disease. J Gastroenterol Hepatol. 2005;20(6):873–81.
Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130(7):417–22.
Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50(3):661–2.
Centers for Disease Control and Prevention. Notice to readers: national hepatitis B initiative for Asian Americans/Native Hawaiian and other Pacific Islanders. Morb Mortal Wkly Rep. 2009;58(18):503.
Hsieh CC, Tzonou A, Zavitsanos X, Kaklamani E, Lan SJ, Trichopoulos D. Age at first establishment of chronic hepatitis B virus infection and hepatocellular carcinoma risk. a birth order study. Am J Epidemiol. 1992;136(9):1115–21.
Hwang SJ, Tong MJ, Lai PP, Ko ES, Co RL, Chien D, Kuo G. Evaluation of hepatitis B and C viral markers: clinical significance in Asian and Caucasian patients with hepatocellular carcinoma in the United States of America. J Gastroenterol Hepatol. 1996;11(10):949–54.
Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–40.
Reeves TJ, Bennett CE. The Asian and Pacific Islander Population in the United States. Washington, DC: Census Bureau. Current Population Reports; 2003:20–540.
U.S. Census Bureau. The American community-Asians: 2004. the American community survey reports. Washington, DC: Department of Commerce; 2007.
McPhee SJ. Caring for a 70-year-old Vietnamese woman. JAMA. 2002;287(4):495–504.
Goodman RA, Sikes RK. Hepatitis B markers in Southeast Asian refugees [letter]. JAMA. 1984;251(16):2086.
Klontz KC. A program to provide hepatitis B immunoprophylaxis to infants born to HBsAg-positive Asian and Pacific Island women. West J Med. 1987;146(2):195–9.
Centers for Disease Control and Prevention. Screening for hepatitis B virus infection among refugees arriving in the United States, 1979-1991. MMWR Morb Mortal Wkly Rep. 1991;40(45):784–6.
Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U S. Cancer Causes Control. 2008;19(3):227–56.
U.S. Census Bureau. American Community Survey. 201. Selected population profile in the United States. Population group: Vietnamese alone. Data Set: 2005-2007 American Community Survey 2003-year estimates. Available at: http://factfinder.census.gov. Accessed January, 2010.
Swallen KC, Glaser SL, Stewart SL, West DW, Jenkins CN, McPhee SJ. Accuracy of racial classification of Vietnamese patients in a population-based cancer registry. Ethn Dis. 1998;8(2):218–27.
Lauderdale DS, Kestenbaum B. Mortality rates of elderly Asian American populations based on Medicare and Social Security data. Demography. 2002;39(3):529–40.
Taylor VM, Nguyen TT, Hoai Do H, Li L, Yasui Y. Lessons learned from the application of a Vietnamese surname list for survey research. J Immigr Minor Health. 2009. doi:10.1007/s10903-009-9296-x
The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 4th ed. Lenexa: AAPOR; 2006.
Maxwell AE, Bastani R, Chen MS, Jr, Nguyen TT, Stewart SL, Taylor VM. Constructing a theoretically-based set of measures for liver cancer control research studies. Prev Med. 2010;50(1–2):68–73.
Bastani R, Glenn BA, Taylor VM, Chen MS, Jr, Nguyen TT, Stewart SL, Maxwell AE. Integrating theory into community interventions to reduce liver cancer disparities: the health behavior framework. Prev Med. 2010;50(1–2):63–7.
Taylor VM, Yasui Y, Burke N, Nguyen T, Chen A, Acorda E, Choe JH, Jackson JC. Hepatitis B testing among Vietnamese American men. Cancer Detec Prev. 2004;28(3):170–7.
Taylor VM, Yasui Y, Burke N, Choe JH, Acorda E, Jackson JJC. Hepatitis B knowledge and testing among Vietnamese-American women. Ethn Dis. Autumn. 2005;15(4):761–7.
Grytdal SP, Liao Y, Chen R, Garvin CC, Grigg-Saito D, Kagawa-Singer M, Liang S, McPhee SJ, Nguyen TT, Tran JH, Gallagher KM. Hepatitis B testing and vaccination among Vietnamese- and Cambodian-Americans. J Commun Health. 2009;34(3):173–80.
Taylor VM, Hislop TG, Tu SP, Teh C, Acorda E, Yip MP, Woodall E, Yasui Y. Evaluation of a Hepatitis B lay health worker intervention for Chinese Americans and Canadians. J Commun Health. 2009;34(3):1625–72.
McPhee SJ, Bird JA, Davis T, Ha NT, Jenkins CN, Le B. Barriers to breast and cervical cancer screening among Vietnamese-American women. Am J Prev Med. 1997;13(3):205–13.
Nguyen TT, McPhee SJ, Gildengorin G, Nguyen T, Wong C, Lai KQ, Lam H, Mock J, Luong TN, Bui-Tong N, Ha-Iaconis T. Papanicolaou testing among Vietnamese Americans: results of a multifaceted intervention. Am J Prev Med. 2006;31(1):1–9.
Hipgrave DB, Nguyen TV, Vu MH, Hoang TL, Do TD, Tran NT, Jolley D, Maynard JE, Biggs BA. Hepatitis B infection in rural Vietnam and the implications for a national program of infant immunization. Am J Trop Med Hyg. 2003;69(3):288–94.
Centers for Disease Control and Prevention. Cost of vaccinating refugees overseas versus after arrival in the United States, 2005. Morb Mortal Wkly Rep. 2008;57(9):229–32.
Bastani R, Glenn BA, Maxwell AE, Jo AM. Hepatitis B testing for liver cancer control among Korean Americans. Ethn Dis. 2007;17(2):365–73.
Ma GX, Fang CY, Shive SE, Toubbeh J, Tan Y, Siu P. Risk perceptions and barriers to Hepatitis B screening and vaccination among Vietnamese immigrants. J Immigr Minor Health. 2007;9(3):213–20.
Coronado GD, Taylor VM, Tu SP, Yasui Y, Acorda E, Woodall E, Yip MP, Li L, Hislop TG. Correlates of hepatitis B testing among Chinese Americans. J Commun Health. 2007;32(6):379–90.
Nguyen TT, McPhee SJ, Nguyen T, Lam T, Mock J. Predictors of cervical Pap smear screening awareness, intention, and receipt among Vietnamese-American women. Am J Prev Med. 2002;23(3):207–14.
Taylor VM, Yasui Y, Burke N, Nguyen T, Acorda E, Thai H, Qu P, Jackson JC. Pap testing adherence among Vietnamese American women. Cancer Epidemiol Biomark Prev. 2004;13(4):613–9.
California Health Interview Survey. CHIS 2007 methodology series: report 4 – response rates. Los Angeles: UCLA Center for Health Policy Research; 2009.
Centers for Disease Control and Prevention. 2007 Behavioral Risk Factor Surveillance System summary data quality report. Available at ftp://ftp.cdc.gov/pub/Data/Brfss/2007SummaryDataQualityReport.pdf, accessed January 18, 2010.
Nguyen TT, Taylor V, Chen MS Jr, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge, and screening among Asian Americans. J Cancer Educ. 2007;22(4):266–72.
Jenkins CN, McPhee SJ, Bird JA, Pham GQ, Nguyen BH, Nguyen T, Lai KQ, Wong C, Davis TB. Effect of a media-led education campaign on breast and cervical cancer screening among Vietnamese-American women. Prev Med. 1999;28(4):395–406.
Nguyen TT, McPhee SJ, Bui-Tong N, Luong TN, Ha-Iaconis T, Nguyen T, Wong C, Lai KQ, Lam H. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Care Poor Underserved. 2006;17(2 Suppl):31–54.
Mock J, McPhee SJ, Nguyen T, Wong C, Doan H, Lai KQ, Nguyen KH, Nguyen TT, Bui-Tong N. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97(9):1693–700.
Nguyen TT, Le G, Nguyen T, Le K, Lai K, Gildengorin G, Tsoh J, Bui-Tong N, McPhee SJ. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med. 2009;37(4):306–13.
McPhee SJ, Nguyen T, Euler GL, Mock J, Wong C, Lam T, Nguyen W, Nguyen S, Huynh Ha MQ, Do ST, Buu C. Successful promotion of hepatitis B vaccinations among Vietnamese-American children ages 3 to 18: results of a controlled trial. Pediatrics. 2003;111(6 Pt 1):1278–88.
Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): how can we do better for this special population? Am J Gastroenterol. 2008;103(7):1824–33.
Acknowledgement
The preparation of this paper was funded in part through grants from the National Cancer Institute Center to Reduce Cancer Health Disparities (U01 CA 114640) and P01 CA109091-01A1 funded jointly by the National Cancer Institute and the National Center on Minority Health and Health Disparities. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies.
Conflict of Interest
There is no conflict of interest reported by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
The preparation of this paper was funded in part through grants from the National Cancer Institute Center to Reduce Cancer Health Disparities (U01 CA 114640) and P01 CA109091-01A1 funded jointly by the National Cancer Institute and the National Center on Minority Health and Health Disparities.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Nguyen, T.T., McPhee, S.J., Stewart, S. et al. Factors Associated with Hepatitis B Testing Among Vietnamese Americans. J GEN INTERN MED 25, 694–700 (2010). https://doi.org/10.1007/s11606-010-1285-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1285-1