ABSTRACT
BACKGROUND
Pay-for-performance programs could worsen health disparities if providers who care for disadvantaged patients face systematic barriers to providing high-quality care. Risk adjustment that includes sociodemographic factors could mitigate the financial incentive to avoid disadvantaged patients.
OBJECTIVE
To test for associations between quality of care and the composition of a physician’s patient panel.
DESIGN
Repeat cross-sectional analysis
PARTICIPANTS
Nationally representative sample of US primary care physicians responding to a panel telephone survey in 2000–2001 and 2004–2005
MAIN MEASURES
Quality of primary care as measured by provision of eight recommended preventive services (diabetic monitoring [hemoglobin A1c testing, eye examinations, cholesterol testing and urine protein analysis], cancer screening [screening colonoscopy/sigmoidoscopy and mammography], and vaccinations against influenza and pneumococcus) documented in Medicare claims data and the association between quality and the sociodemographic composition of physicians’ patient panels.
KEY RESULTS
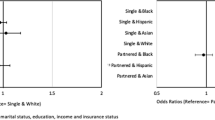
Across eight quality measures, physicians’ quality of care was not consistently associated with the composition of their patient panel either in a single year or between time periods. For example, a substantial number (seven) of the eighteen significant associations seen between sociodemographic characteristics and the delivery of preventive services in the first time period were no longer seen in the second time period. Among sociodemographic characteristics, panel Medicaid eligibility was most consistently associated with differences in the delivery of preventive services between time points; among preventive services, the delivery of influenza vaccine was most likely to demonstrate disparities in both time points.
CONCLUSIONS
In a Medicare pay-for-performance program, a better understanding of the effect of effect of patient panel composition on physicians’ quality of care may be necessary before implementing routine statistical adjustment, since the association of quality and sociodemographic composition is small and inconsistent. In addition, we observed improvements between time periods among physicians with varying panel composition.

Similar content being viewed by others
References
Casalino L, Elster A. Will pay for performance and quality reporting Affect health care disparities? Health Aff. 2007;26:W405–W414.
Smedley, B Stith Y and Nelson R, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington DC: The National Academies Press; 2003
Schneider EC, Zaslavsky A, Epstein A. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA. 2002;287:1288–1294.
Warner R. Does pay for performance steal from the poor and give to the rich? Ann Intern Med. 2010;153:340–341.
Jha A, Orav E, Epstein A. The effect of financial incentives on hospitals that serve poor patients. Ann Intern Med. 2010;153:299–306.
Bach P, Pham HH, Schrag D, Tate R, Hargraves JL. Primary care physicians who treat blacks and whites. New Engl J Med. 2004;351:575–584.
Hong C, Atlas S, Chang Y, Subramanian S, Ashburner J, Barry M, et al. Relationship between patient panel providers and primary care physician clinical performance rankings. JAMA. 2010;304:1107–1113.
Trivedi A, Zaslavsky A, Schneider E, Ayanian J. Trends in the quality of care and racial disparities in managed care. New Engl J Med. 2005;353:692–700.
Franks P, Fiscella K, Meldrum S. Racial disparities in the content of primary care visits. J Gen Intern Med. 2005;20:599–603.
Gornick M. A decade of research on disparities in Medicare utilization: lessons for the health and health care of vulnerable men. Am J Public Health. 2008;98(Supp 1):753–759.
Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA. 2005;294:473–481.
Kalbunde C, Potosky A, Legler J, Warren L. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267.
AQA Approved Quality Measures.http://www.aqaalliance.org/performancewg.htm, and NQF Endorsed Standards. http://qualityforum.org/Measures_List.aspx. Both viewed April 21, 2011.
Friedberg M, Safran D, Coltin K, Dresser M, Schneider E. Paying for performance in primary care: potential impact of practices and disparities. Health Aff. 2010;29(5):1–7.
Rosenthal M, Dudley R. Pay-for-performance: will the latest payment trend improve care? JAMA. 2007;297:740–744.
Fiscella K. Commentary—anatomy of racial disparity in influenza vaccination. HSR: Health Services Research. 2005;40:539–550.
Zhang J, Huang E, Drum M, Kirchhof A, Schlichting J, Schaefer C, et al. Insurance Status and Quality of Diabetes Care in Community Health Centers. Am J Public Health. 2008;99:742–747.
Broyles R, McAuley W, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. Journal of Health Care for the Poor and Underserved. 1999;10:186–200.
Millet C, Gray J, Wall M and Majeed A. Ethnic disparities in coronary heart disease management and pay for performance in the UK. J Gen Intern Med 24 (1): 8–13.
Millet C, Gray J, Saxena S, Netuveli G, Khunti K and Majeed A. Ethnic disparities and diabetes management and pay-for-performance in the UK: The Wandsworth Prospective Diabetes Study. PLoS Med 4(6): e191
Lauderdale DS, Goldberg J. The expanded racial and ethnic codes in the Medicare data files: their completeness of coverage and accuracy. Am J Publ Health. 1996;86:712–716.
Waldo DR. Accuracy and bias of race/ethnicity codes in the Medicare enrollment database. Health Care Financing Review Winter 2004–2005; 26: 61–71
Subramanian SV, Chen JT, Rekhopf DH, et al. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol. 2006;164:823–834.
Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–482.
Acknowledgements
This study was funded by the National Institutes of Health and the Robert Wood Johnson Foundation.
Disclaimer
This paper is based on work conducted before Dr. Pham joined the Center for Medicare & Medicaid Services (CMS), and does not reflect the policies or programs of CMS or of the Department of Health and Human Services.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Carrier, E.R., Schneider, E., Pham, H.H. et al. Association Between Quality of Care and the Sociodemographic Composition of Physicians’ Patient Panels: A Repeat Cross-Sectional Analysis. J GEN INTERN MED 26, 987–994 (2011). https://doi.org/10.1007/s11606-011-1740-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1740-7