Abstract
Objectives
To conduct a systematic review to address the following key questions: (1) what interventions have been successful in improving access for veterans with reduced health care access? (2) Have interventions that have improved health care access led to improvements in process and clinical outcomes?
Data Sources
OVID MEDLINE, CINAHL, PsychINFO.
Study Eligibility Criteria, Participants, and Interventions
English language articles published in peer-reviewed journals from 1990 to June 2010. All interventions designed to improve access to health care for US veterans that reported the impact of the intervention on perceived (e.g., satisfaction with access) or objective (e.g., travel time, wait time) access were included.
Appraisal and Synthesis Methods
Investigators abstracted data on study design, study quality, intervention, and impact of the intervention on access, process outcomes, and clinical outcomes.
Results
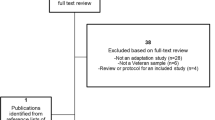
Nineteen articles (16 unique studies) met the inclusion criteria. While there were a small number of studies in support of any one intervention, all showed a positive impact on either perceived or objective measures of access. Implementation of Community Based Outpatient Clinics (n = 5 articles), use of Telemedicine (n = 5 articles), and Primary Care Mental Health Integration (n = 6 articles) improved access. All 16 unique studies reported process outcomes, most often satisfaction with care and utilization. Four studies reported clinical outcomes; three found no differences.
Limitations
Included studies were largely of poor to fair methodological quality.
Conclusions and Implications of Key Findings
Interventions can improve access to health care for veterans. Increased access was consistently linked to increased primary care utilization. There was a lack of data regarding the link between access and clinical outcomes; however, the limited data suggest that increased access may not improve clinical outcomes. Future research should focus on the quality and appropriateness of care and clinical outcomes.

Similar content being viewed by others
References
Agency for Healthcare Research and Quality. 2007 National Healthcare Disparities Report. Rockville, MD: US Department of Health and Human Services, Agency for Healthcare Research and Quality, AHRQ Pub. No. 08–0041, February 2008.
Demakis JG. “Rural Health-Improving Access to Improve Outcomes.” Management Brief, Health Services Research & Development Service, No. 13:1–3, Jan 2000.
Institute of Medicine Committee on Monitoring Access to Personal Healthcare Services. In: Millman M, ed. Access to healthcare in America. Washington, DC: National Academy Press; 1993.
Miller LJ. “Improving Access to Care in the VA Health System: A progress report.” FORUM, VA Health Services Research & Development Service, June 2001.
Fortney J. “A Re-conceptualization of Access for 21stCentury Healthcare.” Oral presentation given to the VA Health Services Research & Development Service Timely Topics of Interest Cyber Seminar Series, August 2010.
Mayo-Smith MF. “Access Issues Within VA Offer Challenges Research Opportunities.” FORUM, VA Health Services Research & Development Service, July 2008.
Weeks WB. “Access to Care: A VA Research Agenda.” FORUM, VA Health Services Research & Development Service. July 2008.
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3S):21–35.
Fortney JC, Borowsky SJ, et al. VA community-based outpatient clinics: access and utilization performance measures. Med Care. 2002;40:561–9.
Fortney JC, Maciejewski ML, et al. Does improving geographic access to VA primary care services impact patients' patterns of utilization and costs? Inquiry. 2005;42:29–42.
Fortney JC, Steffick DE, et al. Are primary care services a substitute or complement for specialty and inpatient services? Health Serv Res. 2005;40:1422–42.
Borowsky SJ, Nelson DB, et al. VA community-based outpatient clinics: performance measures based on patient perceptions of care. Med Care. 2002;40:578–86.
Morgester WA, Biggs CJ. Community-based VHA clinics: effect on patient satisfaction and resource utilization. J Healthc Qual. 2002;24:34–8.
Shiner B, Watts BV, et al. Access to what? An evaluation of the key ingredients to effective advanced mental health access at a VA medical center and its affiliated community-based outreach clinics. Mil Med. 2009;174:1024–32.
Watts BV, Shiner B, et al. Outcomes of a quality improvement project integrating mental health into primary care. Qual Saf Healthcare. 2007;16:378–81.
Druss BG, Rohrbaugh RM, et al. Integrated medical care for patients with serious psychiatric illness. Arch Gen Psychiat. 2001;58:861–8.
Saxon AJ, Malte CA, et al. Randomized trial of onsite versus referral primary medical care for veterans in addictions treatment. Med Care. 2006;44:334–42.
Blue-Howells J, McGuire J, et al. Co-location of healthcare services for homeless veterans: a case study of innovation in program implementation. Soc Work Healthcare. 2008;47:219–231.
McGuire J, Gelberg L, et al. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Admin Policy Ment Health. 2009;36:255–64.
Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health. 2009;15:830–9.
Whited JD, Hall RP, Foy ME, Marbrey LE, Grambow SC, Dudley TK, Datta SK, Simel DL, Oddone EZ. Patient and clinician satisfaction with a store-and-forward teledermatology consult system. Telemed J E Health. 2004;10:422–31.
Whited JD, Hall RP, Foy ME, Marbrey LE, Grambow SC, Dudley TK, Datta S, Simel DL, Oddone EZ. Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8(3):313–21.
Wakefield BJ, Buresh KA, et al. Interactive video specialty consultations in long-term care. J Am Geriatr Soc. 2004;52:789–93.
Wilkins E, et al. Feasibility of virtual wound care. Adv Skin Wound Care. 2007;20:275–8.
Weinberger M, Oddone EZ, et al. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. New Engl J Med. 1986;334:1441–7.
Wray NP, Weiss TW, Menke TJ, Gregor PJ, Ashton CM, Christian CE, Hollingsworth JC. Evaluation of the VA mobile clinics demonstration project. J Healthc Manag. 1999;44:133–47.
Rodriguez KL, Appelt CJ, et al. African American veterans’ experiences with mobile geriatric care. J Healthcare Poor Underserved. 2007;18:44–53.
Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. J Telemed Telecare. 2007;13:142–7.
Bauer MS, McBride L, et al. Impact of an easy-access VA clinic-based program for patients with bipolar disorder. Psychiatr Serv. 1997;48:491–6.
Bauer MS, McBride L, et al. Collaborative care for bipolar disorder: part II. Impact on clinical outcome, function, and costs. Psychiatr Serv. 2006;57:937–45.
Boutelle KN, Dubbert P, et al. A pilot study evaluating a minimal contact telephone and mail weight management intervention for primary care patients. Eat Weight Disord. 2005;10:e1–5.
Chumbler NR, Chuang HC, Wu SS, Wang X, Kobb R, Haggstrom D, Jia H. Mortality risk for diabetes patients in a care coordination, home-telehealth programme. J Telemed Telecare. 2009;15:98–101.
Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG, Rosenthal GE. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed J E Health. 2008;14:753–61.
Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, Barrett D, Knowles F 3rd, Hauser P. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiat. 2004;161:1471–6.
Dobscha SK, Corson K, Perrin NA, Hanson GC, Leibowitz RQ, Doak MN, Dickinson KC, Sullivan MD, Gerrity MS. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301:1242–52.
Dobscha SK, Corson K, Hickam DH, Perrin NA, Kraemer DF, Gerrity MS. Depression decision support in primary care: a cluster randomized trial. Ann Intern Med. 2006;145:477–87.
Hedrick SC, Chaney EF, Felker B, Liu CF, Hasenberg N, Heagerty P, Buchanan J, Bagala R, Greenberg D, Paden G, Fihn SD, Katon WJ. Effectiveness of collaborative care depression treatment in Veterans' Affairs primary care. Gen Intern Med. 2003;18:9–16.
Oslin DW, Sayers S, Ross J, Kane V, Ten Have T, Conigliaro J, Cornelius J. Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosom Med. 2003;65:931–7.
Felker BL, Barnes RF, Greenberg DM, Chaney EF, Shores MM, Gillespie-Gateley L, Buike MK, Morton CE. Preliminary outcomes from an integrated mental health primary care team. Psychiatr Serv. 2004;55:442–4.
Ross JT, TenHave T, Eakin AC, Difilippo S, Oslin DW. A randomized controlled trial of a close monitoring program for minor depression and distress. J Gen Intern Med. 2008 Sep;23:1379–85. Epub 2008 May 23.
Acknowledgements
This report is based on research conducted by the Evidence-based Synthesis Program (ESP) Center located at the Minneapolis VA Health Care System, Minneapolis, MN, funded by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development. The findings and conclusions in this document are those of the author(s) who are responsible for its contents; the findings and conclusions do not necessarily represent the views of the Department of Veterans Affairs or the United States government. Therefore, no statement in this article should be construed as an official position of the Department of Veterans Affairs. This material is the result of work supported with resources and the use of facilities at the Minneapolis VA Medical Center, Minneapolis, MN. Dr. Kehle is supported by a VA Health Services Research & Development Career Development Award.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 62 kb)
Rights and permissions
About this article
Cite this article
Kehle, S.M., Greer, N., Rutks, I. et al. Interventions to Improve Veterans’ Access to Care: A Systematic Review of the Literature. J GEN INTERN MED 26 (Suppl 2), 689 (2011). https://doi.org/10.1007/s11606-011-1849-8
Published:
DOI: https://doi.org/10.1007/s11606-011-1849-8