Abstract
Background
Although early recognition and treatment of diabetes may be essential to prevent complications, roughly one-fifth of diabetes remains undiagnosed.
Objective
Examine cardio-metabolic risk factors and their control in non-Hispanic white (NHW), non-Hispanic black (NHB) and Mexican American (MA) individuals with undiagnosed diabetes.
Design
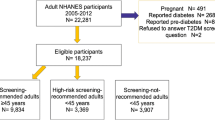
Nationally representative cross-sectional study of participants in the National Health and Nutrition Examination Survey (NHANES) continuous cycles conducted 1999 through 2008.
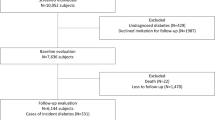
Participants
Of 22,621 non-pregnant individuals aged ≥20 years, 2521 had diagnosed diabetes. Of the remaining 20,100 individuals, 17,963 had HbA1c measured, 551 of whom were classified as having undiagnosed diabetes and comprise the study population.
Main Measures
Undiagnosed diabetes was defined as HbA1c ≥ 6.5% without a self-report of physician diagnosed diabetes. Cardio-metabolic risk factor control was examined using regression methods for complex survey data.
Key Results
Among individuals with undiagnosed diabetes, mean HbA1c level was 7.7% (95% CI: 7.5, 7.9), 19.3% (95% CI: 14.2, 24.3) smoked, 59.7% (95% CI: 54.5, 64.8%) had hypertension and 96.5% (95% CI: 94.6, 98.4%) had dyslipidemia. Lipid profiles were remarkably different across racial-ethnic groups: NHB had the highest LDL- and HDL-cholesterol, but the lowest triglycerides, while MA had the highest triglycerides and the lowest LDL-cholesterol. After adjusting for age, sex, NHANES examination cycle and use of either blood pressure or lipid medication, the odds of having blood pressure ≥130/80 mmHg was higher in NHB [1.92 (95% CI: 1.09, 3.55)] than NHW, while the odds of having LDL-cholesterol >100 mg/dl was higher in NHW[2.93 (95% CI: 1.37, 6.24)] and NHB[3.34 (95% CI: 1.08, 10.3)] than MA.
Conclusions
In a nationally representative sample of individuals with undiagnosed diabetes, cardio-metabolic risk factor levels were high across all racial/ethnic groups, but NHB and MA had poorer control compared to NHW. Interventions that target identification of diabetes and treatment of cardio-metabolic risk factors are needed.
Similar content being viewed by others
References
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–139.
Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559.
Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. N Engl J Med. 2000;342(6):381-9. PMCID: 2630213.
Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–2653. PMCID: 2637991.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. PMCID: 27454.
American Diabetes Association. Standards of medical care in diabetes--2010. Diabetes Care. 2010;33 Suppl 1:S11-61. PMCID: 2797382.
Cowie CC, Rust KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care.33(3):562-8.
Cowie C. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health and Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263–1268.
Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care. 2009;32(2):287–294.
Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994. Diabetes Care. 1998;21(4):518–524.
Chaturvedi N, McKeigue PM, Marmot MG. Resting and ambulatory blood pressure differences in Afro-Caribbeans and Europeans. Hypertension. 1993;22(1):90–96.
Zoratti R, Godsland IF, Chaturvedi N, Crook D, Stevenson JC, McKeigue PM. Relation of plasma lipids to insulin resistance, nonesterified fatty acid levels, and body fat in men from three ethnic groups: relevance to variation in risk of diabetes and coronary disease. Metabolism. 2000;49(2):245–252.
Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988-1994. Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2001;49(2):109–116.
Schmidt MI, Duncan BB, Watson RL, Sharrett AR, Brancati FL, Heiss G. A metabolic syndrome in whites and African-Americans. The Atherosclerosis Risk in Communities baseline study. Diabetes Care. 1996;19(5):414–418.
Lackland DT, Orchard TJ, Keil JE, Saunders DE Jr, Wheeler FC, Adams-Campbell LL, et al. Are race differences in the prevalence of hypertension explained by body mass and fat distribution? A survey in a biracial population. Int J Epidemiol. 1992;21(2):236–245.
Keil JE, Sutherland SE, Hames CG, Lackland DT, Gazes PC, Knapp RG, et al. Coronary disease mortality and risk factors in black and white men. Results from the combined Charleston, SC, and Evans County, Georgia, heart studies. Arch Intern Med. 1995;155(14):1521–1527.
Harris MI, Hadden WC, Knowler WC, Bennett PH. Prevalence of diabetes and impaired glucose tolerance and plasma glucose levels in U.S. population aged 20-74 yr. Diabetes. 1987;36(4):523–534.
Cooper RS, Liao Y, Rotimi C. Is hypertension more severe among U.S. blacks, or is severe hypertension more common? Ann Epidemiol. 1996;6(3):173–180.
Ford ES. Trends in the control of risk factors for cardiovascular disease among adults with diagnosed diabetes: findings from the National Health and Nutrition Examination Survey 1999-2008*. J Diabetes. 2011;3(4):337–347.
Tull ES, Roseman JM. Diabetes in African Americans. In: National Diabetes Data Group. Diabetes in America. 2nd ed. Bethesda (MD): National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases [NIH Publication No. 95–1468]; 1995. pp. 613–30.
Geiss LS, Herman WH, Smith P. Moratlity in non-insulin-dependant diabetes. In : National Diabetes Data Group, ed Diabetes in America: Bethesda, MD: US Dept of HEalth and Human Services, Public Health Service. National Institutes of Health; 1995. p. 233-57.
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. 2011 [updated 2011; cited 2011 04/05/2011]; Available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS. Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care. 2010;33(10):2184–2189. PMCID: 2945158.
Selvin E, Steffes MW, Gregg E, Brancati FL, Coresh J. Performance of A1C for the classification and prediction of diabetes. Diabetes Care. 2011;34(1):84–89.
Boltri JM, Okosun IS, Davis-Smith M, Vogel RL. Hemoglobin A1c levels in diagnosed and undiagnosed black, Hispanic, and white persons with diabetes: results from NHANES 1999-2000. Ethn Dis. 2005;15(4):562–567.
Twombly JG, Long Q, Zhu M, Wilson PW, Narayan KM, Fraser LA, et al. Diabetes care in black and white veterans in the southeastern U.S. Diabetes Care. 2010;33(5):958–963.
Fagot-Campagna A, Narayan KM, Hanson RL, Imperatore G, Howard BV, Nelson RG, et al. Plasma lipoproteins and incidence of non-insulin-dependent diabetes mellitus in Pima Indians: protective effect of HDL cholesterol in women. Atherosclerosis. 1997;128(1):113–119.
Haffner SM, Mykkanen L, Festa A, Burke JP, Stern MP. Insulin-resistant prediabetic subjects have more atherogenic risk factors than insulin-sensitive prediabetic subjects: implications for preventing coronary heart disease during the prediabetic state. Circulation. 2000;101(9):975–980.
McPhillips JB, Barrett-Connor E, Wingard DL. Cardiovascular disease risk factors prior to the diagnosis of impaired glucose tolerance and non-insulin-dependent diabetes mellitus in a community of older adults. Am J Epidemiol. 1990;131(3):443–453.
Medalie JH, Papier CM, Goldbourt U, Herman JB. Major factors in the development of diabetes mellitus in 10,000 men. Arch Intern Med. 1975;135(6):811–817.
Mykkanen L, Kuusisto J, Pyorala K, Laakso M. Cardiovascular disease risk factors as predictors of type 2 (non-insulin-dependent) diabetes mellitus in elderly subjects. Diabetologia. 1993;36(6):553–559.
Hunt KJ, Williams K, Rivera D, O'Leary DH, Haffner SM, Stern MP, et al. Elevated carotid artery intima-media thickness levels in individuals who subsequently develop type 2 diabetes. Arterioscler Thromb Vasc Biol. 2003;23(10):1845–1850.
Mykkanen L, Haffner SM, Kuusisto J, Pyorala K, Laakso M. Microalbuminuria precedes the development of NIDDM. Diabetes. 1994;43(4):552–557.
Hu FB, Stampfer MJ, Haffner SM, Solomon CG, Willett WC, Manson JE. Elevated risk of cardiovascular disease prior to clinical diagnosis of type 2 diabetes. Diabetes Care. 2002;25(7):1129–1134.
Nichols GA, Arondekar B, Herman WH. Medical care costs one year after identification of hyperglycemia below the threshold for diabetes. Med Care. 2008;46(3):287–292.
Nichols GA, Brown JB. Higher medical care costs accompany impaired fasting glucose. Diabetes Care. 2005;28(9):2223–2229. PMCID: 1383774.
Koopman RJ, Mainous AG, 3 rd, Liszka HA, Colwell JA, Slate EH, Carnemolla MA, et al. Evidence of nephropathy and peripheral neuropathy in US adults with undiagnosed diabetes. Ann Fam Med. 2006;4(5):427-32. PMCID: 1578655.
Borg R, Vistisen D, Witte DR, Borch-Johnsen K. Comparing risk profiles of individuals diagnosed with diabetes by OGTT and HbA1c The Danish Inter99 study. Diabet Med. 2010;27(8):906–910.
Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The Economic Burden Of Diabetes. Heal Aff. 2010;29(2):1–7.
Zhang Y, Dall TM, Mann SE, Chen Y, Martin J, Moore V, et al. The economic costs of undiagnosed diabetes. Popul Health Manag. 2009;12(2):95–101.
Acknowledgment
This material is based upon work supported in part by the Office of Research and Development, Department of Veterans Affairs, and the Ralph H. Johnson VAMC. Further support is provided through VA HSR&D REAP Award (grant #IIR-06-219) as well as the National Center on Minority Health and Health Disparities (R01-MD004251). The funding agency did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the U.S. Department of Veterans Affairs.
All authors had access to the data and contributed to the manuscript.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hunt, K.J., Gebregziabher, M. & Egede, L.E. Racial and Ethnic Differences in Cardio-Metabolic Risk in Individuals with Undiagnosed Diabetes: National Health and Nutrition Examination Survey 1999–2008. J GEN INTERN MED 27, 893–900 (2012). https://doi.org/10.1007/s11606-012-2023-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2023-7