Abstract
Background
Bariatric surgery is the most effective weight loss treatment, yet few studies have reported on short- and long-term outcomes postsurgery.
Methods
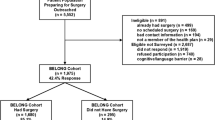
Using claims data from seven Blue Cross/Blue Shield health plans serving seven states, we conducted a non-concurrent, matched cohort study. We followed 22,693 persons who underwent bariatric surgery during 2003–2007 and were enrolled at least 6 months before and after surgery. Using logistic regression, we compared serious and less serious adverse clinical outcomes, hospitalizations, planned procedures, and obesity-related co-morbidities between groups for up to 5 years.
Results
Relative to controls, surgery patients were more likely to experience a serious [odds ratio (OR) 1.9; 95% confidence interval (CI) 1.8–2.0] or less serious (OR 2.5, CI 2.4–2.7) adverse clinical outcome or hospitalization (OR 1.3, CI 1.3–1.4) at 1 year postsurgery. The risk remained elevated until 4 years postsurgery for serious events and 5 years for less serious outcomes and hospitalizations. Some complication rates were lower for patients undergoing laparoscopic surgery. Planned procedures, such as skin reduction, peaked in postsurgery year 2 but remained elevated through year 5. Surgery patients had a 55% decreased risk of obesity-related co-morbidities, such as type 2 diabetes, in the first year postsurgery, which remained low throughout the study (year 5: OR 0.4, CI 0.4–0.5).
Conclusions
While bariatric surgery is associated with a higher risk of adverse clinical outcomes compared to controls, it also substantially decreased obesity-related co-morbidities during the 5-year follow-up.



Similar content being viewed by others
References
U.S. Obesity Trends from 1985 to 2005. http://www.cdc.gov/obesity/data/trends.html#State. Accessed 15 June 2010.
Obesity and overweight—facts. http://www.who.int/features/factfiles/obesity/en/. Accessed 18 Feb 2011.
Davis MM, Slish K, Chao C, et al. National trends in bariatric surgery, 1996–2002. Arch Surg. 2006;141(1):71–4.
Li Z, Maglione M, Tu W, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med. 2005;142(7):532–46.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142(7):547–59.
Agren G, Narbro K, Jonsson E, et al. Cost of in-patient care over 7 years among surgically and conventionally treated obese patients. Obes Res. 2002;10(12):1276–83.
Angus LD, Cottam DR, Gorecki PJ, et al. DRG, costs and reimbursement following Roux-en-Y gastric bypass: an economic appraisal. Obes Surg. 2003;13(4):591–5.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240(3):416–23.
Cooney RN, Haluck RS, Ku J, et al. Analysis of cost outliers after gastric bypass surgery: what can we learn? Obes Surg. 2003;13(1):29–36.
Courcoulas A, Perry Y, Buenaventura P, et al. Comparing the outcomes after laparoscopic versus open gastric bypass: a matched paired analysis. Obes Surg. 2003;13(3):341–6.
Courcoulas A, Schuchert M, Gatti G, et al. The relationship of surgeon and hospital volume to outcome after gastric bypass surgery in Pennsylvania: a 3-year summary. Surgery. 2003;134(4):613–21.
Encinosa WE, Bernard DM, Chen CC, et al. Healthcare utilization and outcomes after bariatric surgery. Med Care. 2006;44(8):706–12.
Encinosa WE, Bernard DM, Du D, et al. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47(5):531–5.
Encinosa WE, Bernard DM, Steiner CA, et al. Use and costs of bariatric surgery and prescription weight-loss medications. Health Aff (Millwood). 2005;24(4):1039–46.
Flum DR, Salem L, Elrod JA, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA. 2005;294(15):1903–8.
Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54.
Gallagher SF, Banasiak M, Gonzalvo JP, et al. The impact of bariatric surgery on the Veterans Administration healthcare system: a cost analysis. Obes Surg. 2003;13(2):245–8.
Liu JH, Zingmond D, Etzioni DA, et al. Characterizing the performance and outcomes of obesity surgery in California. Am Surg. 2003;69(10):823–8.
Livingston EH, Liu CY, Glantz G, et al. Characteristics of bariatric surgery in an integrated VA Health Care System: follow-up and outcomes. J Surg Res. 2003;109(2):138–43.
Martin LF, Tan TL, Horn JR, et al. Comparison of the costs associated with medical and surgical treatment of obesity. Surgery. 1995;118(4):599–606.
Narbro K, Agren G, Jonsson E, et al. Sick leave and disability pension before and after treatment for obesity: a report from the Swedish Obese Subjects (SOS) study. Int J Obes Relat Metab Disord. 1999;23(6):619–24.
Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279–89.
Nguyen NT, Paya M, Stevens CM, et al. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg. 2004;240(4):586–93.
Sampalis JS, Sampalis F, Christou N. Impact of bariatric surgery on cardiovascular and musculoskeletal morbidity. Surg Obes Relat Dis. 2006;2(6):587–91.
Sampalis JS, Liberman M, Auger S, et al. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes Surg. 2004;14(7):939–47.
Sjostrom L, Gummesson A, Sjostrom CD, et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 2009;10(7):653–62.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294(15):1909–17.
Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA. 2005;294(15):1918–24.
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—Executive summary. Bethesda, MD:NHLBI; 2002).
Clark JM, Chang HY, Bolen SD, Shore AD, Goodwin SM, Weiner JP. Development of a Claims-Based Risk Score to Identify Obese Individuals. Popul Health Manag. 2010;13:201–7
Spencer EA, Appleby PN, Davey GK, et al. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5(4):561–5.
Nyholm M, Gullberg B, Merlo J, et al. The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring). 2007;15(1):197–208.
Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80(1):27–38.
Starfield B, Weiner J, Mumford L, et al. Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res. 1991;26(1):53–74.
Weiner JP, Starfield BH, Steinwachs DM, et al. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29(5):452–72.
Rosenbaum P. Observational studies. 2nd ed. New York: Springer; 2002.
Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Obesity (Silver Spring). 2009;17 Suppl 1:S1–S70.
Conflicts of Interest
None for any of the authors.
Funding/Support
This study was funded by unrestricted research grants from Ethicon Endo-Surgery, Inc. (a Johnson & Johnson company); Pfizer, Inc.; and GlaxoSmithKline. In-kind support was provided by the BlueCross BlueShield Association and the seven local Blue Cross Blue Shield plans participating in this project. Dr. Bolen’s salary was supported on the following two grants during part of the time she was working on this project: NIH/NCI 5R25T CA111898-04 and RR KL204990. Grant number RR KL204990 was from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The publication’s contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Role of the Sponsor
The funding and collaborating organizations were kept informed of the study’s progress and shared their expertise on certain aspects of the study. In addition, preliminary findings were shared with them, and they were invited to review the manuscript. However, they did not have any direct role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation or approval of the manuscript.
Additional Contributions
We thank the Blue Cross and Blue Shield plans and the many staff members at these sites who actively contributed to this study by providing data and expert advice regarding use of these data. These organizations included Blue Cross Blue Shield of Tennessee, Highmark Blue Cross Blue Shield (of Pennsylvania), Blue Cross Blue Shield of Michigan, Blue Cross Blue Shield of North Carolina Independence Blue Cross (of Pennsylvania), Wellmark Blue Cross and Blue Shield of Iowa, Wellmark Blue Cross and Blue Shield of South Dakota, and Blue Cross Blue Shield of Hawaii.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bolen, S.D., Chang, HY., Weiner, J.P. et al. Clinical Outcomes after Bariatric Surgery: A Five-Year Matched Cohort Analysis in Seven US States. OBES SURG 22, 749–763 (2012). https://doi.org/10.1007/s11695-012-0595-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0595-2