Opinion statement
Episodes of paroxysmal sympathetic hyperactivity, sometimes referred to as autonomic storms, are not uncommon in patients with severe traumatic brain injury. Their distinctive characteristics include fever, tachycardia, hypertension, tachypnea, hyperhidrosis, and dystonic posturing. The episodes may be induced by stimulation or may occur spontaneously. Their pathophysiology has not been fully elucidated, but the manifestations clearly indicate activation or disinhibition of sympathoexcitatory areas. These spells are often confused with seizures, leading to unnecessary treatment with antiepileptic drugs. General principles in the management of paroxysmal sympathetic hyperactivity include adequate hydration, exclusion of mimicking conditions (infection, pulmonary embolism, hydrocephalus, epilepsy), effective analgesia, and avoidance of triggers, when identified. The most useful pharmacologic agents are morphine sulfate and nonselective β-blockers (eg, propranolol). Intrathecal baclofen may be effective in refractory cases. Bromocriptine and clonidine are helpful in some patients, but their efficacy is less consistent. Early recognition and adequate treatment of paroxysmal sympathetic hyperactivity is important to avoid prolongation of the patient’s stay in the intensive care unit and to enable recovering patients to participate without restrictions in rehabilitation therapy.
Similar content being viewed by others
References and Recommended Reading
Boeve BF, Wijdicks EF, Benarroch EE, Schmidt KD: Paroxysmal sympathetic storms (“diencephalic seizures”) after severe diffuse axonal head injury. Mayo Clin Proc 1998, 73:148–152.
Audibert G, Charpentier C, Seguin-Devaux C, et al.: Improvement of donor myocardial function after treatment of autonomic storm during brain death. Transplantation 2006, 82:1031–1036.
Bullard DE: Diencephalic seizures: responsiveness to bromocriptine and morphine. Ann Neurol 1987, 21:609–611.
Rossitch E Jr, Bullard DE: The autonomic dysfunction syndrome: aetiology and treatment. Br J Neurosurg 1988, 2:471–478.
Blackman JA, Patrick PD, Buck ML, Rust RS Jr.: Paroxysmal autonomic instability with dystonia after brain injury. Arch Neurol 2004, 61:321–328.
Baguley IJ, Nicholls JL, Felmingham KL, et al.: Dysautonomia after traumatic brain injury: a forgotten syndrome? J Neurol Neurosurg Psychiatry 1999, 67:39–43.
Baguley IJ, Cameron ID, Green AM, et al.: Pharmacological management of dysautonomia following traumatic brain injury. Brain Inj 2004, 18:409–417.
Baguley IJ, Heriseanu RE, Felmingham KL, Cameron ID: Dysautonomia and heart rate variability following severe traumatic brain injury. Brain Inj 2006, 20:437–444.
Rabinstein AA: Paroxysmal sympathetic hyperactivity in the neurological intensive care unit. Neurol Res 2007, 29:680–682.
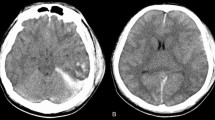
Fernandez-Ortega JF, Prieto-Palomino MA, Munoz-Lopez A, et al.: Prognostic influence and computed tomography findings in dysautonomic crises after traumatic brain injury. J Trauma 2006, 61:1129–1133.
Talman WT, Florek G, Bullard DE: A hyperthermic syndrome in two subjects with acute hydrocephalus. Arch Neurol 1988, 45:1037–1040.
Tong C, Konig MW, Roberts PR, et al.: Autonomic dysfunction secondary to intracerebral hemorrhage. Anesth Analg 2000, 91:1450–1451.
Rabinstein AA: Paroxysmal autonomic instability after brain injury [letter]. Arch Neurol 2004, 61:1625.
Wilkinson R, Meythaler JM, Guin-Renfroe S: Neuroleptic malignant syndrome induced by haloperidol following traumatic brain injury. Brain Inj 1999, 13:1025–1031.
Vincent FM, Zimmerman JE, Van Haren J: Neuroleptic malignant syndrome complicating closed head injury. Neurosurgery 1986, 18:190–193.
Chiolero RL, Breitenstein E, Thorin D, et al.: Effects of propranolol on resting metabolic rate after severe head injury. Crit Care Med 1989, 17:328–334.
Feibel JH, Baldwin CA, Joynt RJ: Catecholamine-associated refractory hypertension following acute intracranial hemorrhage: control with propranolol. Ann Neurol 1981, 9:340–343.
Do D, Sheen VL, Bromfield E: Treatment of paroxysmal sympathetic storm with labetalol. J Neurol Neurosurg Psychiatry 2000, 69:832–833.
Welle S, Schwartz RG, Statt M: Reduced metabolic rate during betaadrenergic blockade in humans. Metabolism 1991, 40:619–622.
Christin L, Ravussin E, Bogardus C, Howard BV: The effect of propranolol on free fatty acid mobilization and resting metabolic rate. Metabolism 1989, 38:439–444.
Head GA, Chan CK, Burke SL: Relationship between imidazoline and alpha2adrenoceptors involved in the sympathoinhibitory actions of centrally acting antihypertensive agents [review]. J Auton Nerv Syst 1998, 72:163–169.
Payen D, Quintin L, Plaisance P, et al.: Head injury: clonidine decreases plasma catecholamines. Crit Care Med 1990, 18:392–395.
Russo RN, O’Flaherty S: Bromocriptine for the management of autonomic dysfunction after severe traumatic brain injury. J Paediatr Child Health 2000, 36:283–285.
Cuny E, Richer E, Castel JP: Dysautonomia syndrome in the acute recovery phase after traumatic brain injury: relief with intrathecal Baclofen therapy. Brain Inj 2001, 15:917–925.
Becker R, Benes L, Sure U, et al.: Intrathecal baclofen alleviates autonomic dysfunction in severe brain injury. J Clin Neurosci 2000, 7:316–319.
Coffey RJ, Edgar TS, Francisco GE, et al.: Abrupt withdrawal from intrathecal baclofen: recognition and management of a potentially lifethreatening syndrome. Arch Phys Med Rehabil 2002, 83:735–741.
Turner MR, Gainsborough N: Neuroleptic malignant-like syndrome after abrupt withdrawal of baclofen. J Psychopharmacol 2001, 15:61–63.
Cunningham JA, Jelic S: Baclofen withdrawal: a cause of prolonged fever in the intensive care unit. Anaesth Intensive Care 2005, 33:534–537.
Baguley IJ, Heriseanu RE, Gurka JA, et al.: Gabapentin in the management of dysautonomia following severe traumatic brain injury: a case series. J Neurol Neurosurg Psychiatry 2007, 78:539–541.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rabinstein, A.A., Benarroch, E.E. Treatment of paroxysmal sympathetic hyperactivity. Curr Treat Options Neurol 10, 151–157 (2008). https://doi.org/10.1007/s11940-008-0016-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-008-0016-y