Abstract
Purpose
Modern neuraxial labour analgesia reflects a shift in obstetrical anesthesia thinking – away from a simple focus on pain relief towards a focus on the overall quality of analgesia. However, advances in the methods used to measure outcomes have not kept pace with clinical progress, and these approaches must evolve to facilitate meaningful assessment of the advances provided towards the quality of analgesia. Developing a tool to measure the quality of neuraxial labour analgesia that research has achieved is best guided by women’s perspectives. As the initial step in developing an instrument to quantitatively measure quality neuraxial labour analgesia, this qualitative descriptive study explored childbearing women’s experiences and perspectives regarding this subject.
Methods
Twenty-eight postpartum women, all delivering with neuraxial labour analgesia, were recruited from three hospitals in the greater Toronto area. Twenty-five women described a priori plans to use neuraxial labour analgesia, or they described themselves as having been open to the idea. Women’s experiences and perspectives of neuraxial labour analgesia were explored in focus groups and in-depth interviews ≤72 hr following childbirth.
Results
Four major themes emerged: 1)The Enormity of Labour Pain; 2) Fear and Anxiety Related to Epidural Pain Relief; 3) What Women Value about Epidural Pain Relief; and 4) The Relative Value of Achieving Epidural Pain Relief vs Avoidance of Epidural Drug Side Effects. Participants broadly described quality neuraxial labour analgesia as pain relief without side effects. Responses affirmed the importance of traditionally measured outcomes as attributes of quality neuraxial labour analgesia, e.g., pain relief and side effects, as well as the overall importance of pain control during labour and delivery. For research to capture the experience of quality neuraxial labour analgesia, findings suggest that this outcome involves physical, cognitive, and emotional dimensions that must be measured. The findings further suggest an important relationship between each of these dimensions and perceptions of control.
Conclusions
Women’s perspectives must be incorporated into the assessment of quality neuraxial labour analgesia in order for research to measure this outcome in a meaningful manner. Study findings have important implications for scale development, interpretation of existing research, and antenatal education.
Résumé
Objectif
L’analgésie neuraxiale moderne pour le travail obstétrical reflète un changement dans la façon de penser l’anesthésie obstétricale. Cette nouvelle manière de penser s’éloigne du simple objectif de soulagement de la douleur pour se tourner davantage vers un objectif de qualité globale de l’analgésie. Toutefois, les progrès apportés aux méthodes d’évaluation des devenirs ont pris du retard par rapport aux progrès cliniques; ces approches se doivent d’évoluer afin de faciliter une évaluation pertinente des progrès en matière de qualité de l’analgésie. Si l’on souhaite mettre au point un outil pour mesurer la qualité de l’analgésie neuraxiale pour le travail obstétrical atteinte grâce à la recherche, il importe de s’appuyer sur les attentes des femmes. Cette étude descriptive et qualitative a exploré les expériences et les attentes des femmes enceintes. Il s’agit de la première étape dans la mise au point d’un instrument de mesure quantitative de l’analgésie neuraxiale de qualité pour le travail obstétrical.
Méthode
Vingt-huit femmes en post-partum, ayant toutes accouché avec une analgésie neuraxiale pour le travail obstétrical, ont été recrutées dans trois hôpitaux de la région du Grand Toronto. Vingt-cinq de ces femmes ont fait état de plans a priori impliquant le recours à une analgésie neuraxiale pour le travail obstétrical, ou se sont décrites comme étant ouvertes à cette idée. Les expériences et attentes des femmes concernant l’analgésie neuraxiale pour le travail obstétrical ont été examinées dans des groupes de discussion et des entretiens approfondis ≤72 h après l’accouchement.
Résultats
Quatre grands thèmes sont apparus: 1) l’énormité de la douleur liée au travail obstétrical; 2) la peur et l’anxiété associées au soulagement de la douleur par péridurale; 3) ce que les femmes apprécient du soulagement de la douleur; et 4) la valeur relative d’un soulagement de la douleur par péridurale par rapport au fait d’éviter les effets secondaires associés au médicament de la péridurale. Les participantes ont pour la plupart décrit une analgésie neuraxiale pour le travail obstétrical de qualité comme un soulagement de la douleur sans effets secondaires. Les réponses ont confirmé l’importance des résultats traditionnellement mesurés en tant qu’attributs d’une analgésie neuraxiale pour le travail obstétrical de qualité, par exemple le soulagement de la douleur et les effets secondaires, ainsi que l’importance globale du contrôle de la douleur pendant le travail et l’accouchement. Si l’on veut que nos recherches saisissent ce qui est nécessaire à une analgésie neuraxiale de qualité pour le travail obstétrical, nos résultats suggèrent que ce devenir doit inclure des dimensions physiques, cognitives et émotionnelles qu’il faut mesurer. Nos résultats suggèrent également qu’il existe une relation importante entre chacune de ces dimensions et les perceptions de contrôle.
Conclusion
Les attentes des femmes doivent être intégrées dans l’évaluation de la qualité d’une analgésie neuraxiale pour le travail obstétrical afin de mesurer ce devenir de façon pertinente. Les résultats de cette étude ont des implications de taille en ce qui touche à la mise au point d’une échelle, à l’interprétation des recherches existantes et à l’éducation prénatale.
Similar content being viewed by others
The advent of modern neuraxial labour analgesia reflects a paradigm shift in thinking in obstetrical anesthesia – away from a solitary focus on pain relief towards a focus on pain control associated with minimal drug-related side effects – namely, towards a focus on the overall quality of analgesia provided. To achieve this purpose, a variety of interventions have evolved over the past two decades, including use of low doses of local anesthetic/opioid drug mixtures, combined spinal epidural (CSE) analgesia, and patient-controlled epidural analgesia (PCEA). These innovations have changed the landscape of labour and delivery pain relief dramatically, providing women with increased mobility, sensation, and control over their own pain treatment compared with traditional local anesthetic-based epidural pain relief.1 - 4
While there is little doubt that modern neuraxial labour analgesia has improved the pain relief experience, numerous issues bar meaningful outcome assessment in trials, and the degree to which different approaches have advanced the quality of labour and delivery analgesia cannot be compared directly one with the other. One such issue is the lack of guidance provided by women’s perspectives related to which outcomes must be measured as important markers of clinical progress. The need for an improvement in incorporating childbearing women’s views into measuring outcomes leaves the validity (meaningfulness) of current research open to challenge and the overall importance of the demonstrated differences open to interpretation.5 - 8 Furthermore, use of satisfaction, a multi-dimensional measure commonly included as a surrogate marker for the overall adequacy of pain relief, is also problematic. Numerous issues have been described regarding the reliability and validity of the information obtained using this measure in obstetric patients, including paradoxical findings of high levels of pain in association with high levels of satisfaction.9 Taken in their totality, these observations suggest that labour analgesia research is best served by direct measurement and comparison of the overall quality of analgesia achieved in clinical trials.
Qualitative descriptive research is the recommended first step in health instrument development, and it is necessary to ensure that outcome measurement meaningfully reflects the experiences and perspectives of those for whom it is intended.10 , 11 We conducted a qualitative descriptive study to explore childbearing women’s experiences and perspectives of neuraxial labour pain relief, including the aspects they valued and disliked and those they viewed as part of quality analgesia for labour and delivery. This study represents the first in a series of studies conducted to develop a tool to measure the quality of neuraxial analgesia achieved in labour analgesia trials.
Methods
Sampling
Following research ethics board approval in each participating institution, postpartum women were recruited from three hospitals (one teaching, two large communities) with a combined delivery rate of >10,000 births per annum. The hospitals were located in the northern, eastern, and central regions of the greater Toronto area. All of the women provided written informed consent. A purposeful representative sampling strategy was used to permit exploration of a broad spectrum of women’s labour epidural analgesia experiences.12 - 14 This strategy provided a sampling of women of mixed parity who had experienced the spectrum of delivery methods. Eligibility criteria included: 1) American Society of Anesthesiologists status I-II; 2) fluency in English; 3) receipt of an epidural or CSE during the current labour; and 4) delivery within the previous 72 hr. Exclusion criteria included evidence or history of maternal cognitive impairment or neonatal death during the current pregnancy.
Screening occurred on postpartum wards in each institution, with all potentially eligible patients identified by the charge nurse on any given day when recruitment was occurring. The screening was followed by a review of the patient’s medical record to ensure eligibility and an invitation to participate in the study. All potentially eligible postpartum women were approached. The women were given the option to participate in a focus group or in an in-depth interview depending on the number of women recruited on any given day. Tiredness was the most common reason given for refusal. The sampling was terminated when little new information was retrieved. Recruitment occurred from September 18, 2003 to January 9, 2004.
Data collection
All participants completed a demographic survey and participated in one of five focus groups or in one of fifteen one-to-one in-depth interviews. All sessions were conducted within 72 hr of delivery and prior to discharge from hospital. Focus groups ranged in size from two to four participants and lasted approximately 1.5 to 2 hr. In-depth interviews lasted from 45 min to one hour. All sessions were conducted using a semi-structured interview guide (see Box 1) and were audiotaped and transcribed verbatim. Member checking (verification of the investigator’s interpretation of the findings with participants) was undertaken at the end of each focus group and interview. Researchers debriefed and reviewed field notes after each session. The results of each session informed subsequent sessions, enabling the researchers to probe newly identified or rich topics in subsequent groups. The same trained moderator (P.A.) and assistant moderator (J.Y.) facilitated all of the sessions. Additional details relating to labour and delivery management were collected from the women’s medical records. This manuscript presents findings from key questions about the aspects of neuraxial labour analgesia that women valued and disliked and those aspects they viewed as a part of ideal or quality neuraxial pain relief during labour and delivery. Findings from other questions will be reported at a later date.
Data analysis
Qualitative content analysis, the strategy of choice for qualitative descriptive studies, was used to analyze the data.11 , 15 , 16 All transcripts were reviewed as soon as available, and data collection and analysis were undertaken concurrently. The transcripts were reviewed independently and coded by two researchers (P.A., C.K.L.) with the assistance of NVIVO QSR 2.0.Footnote 1 Style code editing was implemented whereby codes were derived inductively from the data.17 Initially, specific words and phrases were coded that described aspects of the women’s experiences. Memos were made while coding to facilitate making inferences from the data.12 Next, codes reflecting similar ideas within and across the focus groups and the in-depth interviews were clustered into categories (themes). The researchers (P.A., C.K.L.) then compared their codes and emerging themes and established inter-rater consensus. Categories of related themes were then combined to obtain broad overarching themes that gave a holistic view of the data.11 , 18
Results
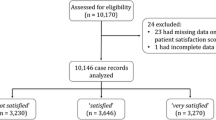
Fifty-nine of the 79 women whose charts were screened met study eligibility criteria. Reasons for ineligibility included lack of fluency in English (n = 13) and not receiving epidural analgesia for labour (n = 7). A total of 28 women participated in the study, which represented 50% of those eligible in the teaching hospital (22/44) and 40% (6/15) of those eligible in community hospitals. Demographic characteristics of the participants are presented in Table 1. Roughly equal numbers of primiparous and multiparous women participated. Most of the women were either university or community college educated with household incomes >$80,000 CDN per year and delivered in a teaching hospital. All women received neuraxial analgesia for labour with most receiving it from 3-4 cm of cervical dilatation. Thirty-nine percent (11/28) of the women underwent induction of labour, and 64% (18/28) of the labours were augmented with oxytocin and/or amniotomy. Forty-six percent (13/28) of the women delivered spontaneously.
Drugs and methods of maintenance of neuraxial analgesia are described for each participating institution (Table 2). Two study sites provided the women with PCEA combined with a continuous background epidural infusion. One community hospital did not offer PCEA and provided maintenance of analgesia using a continuous epidural infusion only. In all settings, additional rescue boluses of epidural medication were available and provided by either nurses or anesthesiologists. Twenty-five of the 28 participants either knew that they desired neuraxial analgesia ahead of labour or noted that they were open to receiving it if they felt it necessary. These women were very positive about their pain relief and the necessity of having it available during childbirth.
Four major themes, each with 2-5 subthemes, emerged from the data: 1) The Enormity of Labour Pain; 2) Fear and Anxiety Related to Epidural Pain Relief; 3) The Value that Women Place on Epidural Pain Relief; and 4) The Relative Value of Achieving Epidural Pain Relief vs Avoidance of Epidural Drug Side Effects. Themes were intertwined and interacting, but they are presented separately below for the purposes of presentation.
Theme 1: The enormity of labour pain (Box 2)
This theme described participants’experiences as they struggled to deal with pain over the course of labour. The first subtheme was “An Unbearable Level of Pain” (Box 2), which described the nature of the pain participants encountered. Many (17/28) women voiced that they were already close to or beyond their ability to cope by the time they decided to have epidural analgesia. The second subtheme was, “An Inability to Focus”, which described the impact of pain on women’s mental capacity to focus and process information. The third subtheme, “The Struggle to Maintain Self-control” described the difficulties women encountered in maintaining mental and emotional control in the face of severe pain.
Theme 2: Fear and anxiety related to epidural pain relief (Box 3)
The second major theme captured the spectrum of fears related to pain relief for childbirth. Its four subthemes are illustrated by quotes in Box 3. The first was “Being Able to Freely Choose Epidural Relief.” Participants described a variety of circumstances associated with anxiety over their ability to freely choose neuraxial pain relief. These occurred when they felt their choice for pain relief opposed views of family members, their physicians, or other health care providers. Women shared that they valued being in an environment where they felt that their choice for pain relief was supported. Most (25/28) participants shared that they had either planned to have epidural analgesia a priori or described themselves as open to having it prior to labour onset. One (nulliparous) participant voiced disappointment over her use of epidural analgesia. She expressed fears over potential problems with long-term back pain and her belief that she had received epidural pain relief because of insufficient nursing support.
The second subtheme was “Apprehension over Access and Availability of Epidural Pain Relief.” Participants, particularly multiparous women, described apprehension over having ready access to epidural pain relief if and when they chose it. Their concerns related to arriving at hospital with enough time to have an epidural, the availability of the anesthesiologist, and availability and accessibility of epidural analgesia services at the hospital where they planned to deliver.
The third subtheme, “Apprehension over the Effects of the Epidural on Labour Progress,” described the variety of concerns expressed by participants relating to the impact of epidural pain relief on labour progress. These concerns included the epidural’s effect on the speed of labour progress, their ability to push and participate, and its potential impact on mode of delivery.
The fourth subtheme, “Fears Related to Epidural Insertion,” described a spectrum of concerns relating to epidural placement, including the pain of insertion, long-term back pain, nerve injury, and paralysis. Concerns were voiced most commonly by primiparous patients. Multiparous women related concerns more often about timely access to epidural pain relief than about side effects, citing their own good experiences or the good experiences of friends as reassuring.
Theme 3: What women value about epidural pain relief (Box 4)
This theme was composed of five subthemes that captured the variety of ways participants described the impact of epidural analgesia on their labour and delivery experiences (Box 4). The first subtheme, “Pain Relief Restores Feelings of Internal Control and the Ability to Focus,” described the value of epidural pain relief on participants’ abilities to cope with pain and to focus on the birth itself. The second subtheme, “Modern Neuraxial Analgesia Permits Participation and Control,” described participants’ perspectives on the use of PCEA. Women who had received PCEA voiced that they liked the control it had afforded them over their pain, stressing their fear and anxiety over breakthrough pain and the importance of preventing it. Parturients from the hospital where PCEA was not available shared a variety of beliefs, including a desire to receive PCEA in the future, fear regarding their ability to use it effectively, and fear regarding their ability to use PCEA safely. The third subtheme, “The Value of Pain Relief that Preserves Bodily Sensations of Labour Progress,” described, in a variety of ways, that women did not want to feel pain; however, they valued being able to feel other sensations that reassured them of labour progress, e.g., tightening of contractions (without pain) or the urge to push. They shared that preservation of these sensations allowed them to participate in the birth experience. The fourth subtheme was “The Value of Pain Relief that Preserves Mobility and Strength”. Women shared that they valued pain relief but also valued mobility and feeling that they were able to push effectively. Complete immobility was associated with discomfort, anxiety, and fear, whereas intermediate levels of mobility (bending knees, moving feet) were described as more acceptable. The fifth subtheme, “Pain Relief Improves Women’s Labour and Delivery Experiences,” described the variety of ways that participants expressed what they valued about having neuraxial pain relief as part of their childbirth experience, including the psychological relief associated with pain control and an improved ability to focus on and enjoy the birth experience.
Theme 4: The relative value of epidural pain relief vs avoidance of epidural drug side effects (Box 5)
The fourth major theme included two subthemes and captured women’s perspectives on the importance of ensuring pain relief over common epidural side effects. Box 5 presents quotes illustrating these subthemes. The first subtheme was “Pain Control is Most Important.” The majority (27/28) of participants voiced that they valued pain control, including prevention of breakthrough pain, more highly than avoiding common drug-related side effects associated with epidural analgesia. The second subtheme was “The Relative Importance of Preserving Strength and Mobility over Avoidance of other Epidural Drug Side Effects.” Once pain was assured, most women (24/28) shared that they valued preservation of strength and mobility more highly than avoidance of other side effects, such as heavy numbness, itching, or the inability to urinate. Preserved strength was associated with improved bodily control and a sense of being able to participate more actively in the birth process. Heavy motor block, while acceptable if necessary to prevent high levels of pain, was associated with varying levels of anxiety in some women. Opioid-induced itching and difficulties with urination were described by many participants as being of lesser importance than other epidural drug side effects.
Discussion
This study was conducted as the first step in the development of a multidimensional tool to measure the quality of neuraxial labour analgesia achieved in clinical trials. We explored parturient perspectives and experiences to help ensure that the instrument, which ultimately will be developed, will reflect all of the important dimensions that constitute quality analgesia for childbearing women. Significant differences have been shown to exist between patient and health provider ratings regarding the value of a given health state, and as a general rule, research supports use of tools that reflect patient perspectives.19
Multidimensional instruments have been developed and validated for use in many areas of health research, but they are not commonly available in obstetrical anesthesia.19 - 22 These types of tools permit assessment of various dimensions of health (physical, mental, emotional) in various forms (health profiles, health indices). By generating a summation of the scores for each dimension of quality into a global score (index of the quality achieved), a health index can be used to compare directly the overall quality of health (or analgesia) achieved in a given treatment arm. By integrating patient-perceived benefits and harms into a single score, global measures, such as the overall quality of analgesia achieved over a given time interval, are likely to provide the best means of assessing the overall importance of subtle and/or complex combinations of findings in neuraxial labour analgesia trials.19 , 23
Participants in this study provided valuable insights into the dimensions that should be measured to capture quality neuraxial labour analgesia as a research outcome. While women described quality neuraxial labour analgesia as pain relief without side effects, their responses indicated the need to capture information broadly as it relates to cognitive, emotional, and physical dimensions of this outcome. Responses also suggested an important relationship between these dimensions and perceptions of control.
Within the physical dimension, participants affirmed the importance of traditionally measured attributes, i.e., pain/pain relief and minimization of motor and sensory block and pruritus. Responses suggested that the methods currently used to measure these outcomes require modification, e.g., the language used for description and the perspective of assessment, to capture information that reflects women’s experiences more meaningfully. Women’s discussions further suggested specific attributes relating to control that should be measured within this dimension. These attributes included pain control/ prevention of breakthrough pain, participation in pain control, mobility, and the degree to which analgesia regimens permit preservation of the bodily sensations of labour progress, including those that permit participation in the birth without pain.
Similarly, participants’ responses suggested the need to capture information relating to cognitive and emotional dimensions of quality neuraxial analgesia as well as regarding a relationship between these dimensions and perceptions of control. The latter was demonstrated by responses suggesting that pain control improved women’s abilities to function in the cognitive dimension, i.e., to focus, process, and respond appropriately to information and to cope with less control in the physical dimension, e.g., immobility. Conversely, women’s experiences of poor quality analgesia were associated with loss of control in both emotional, e.g., fear and anxiety, and cognitive dimensions.
These findings, as well as other work, support the need for more direct capture of information related to women’s perceptions of participation and control during labour and delivery.24 , 25 Our findings and those of othersFootnote 2 , 26 further suggest that this information is necessary to allow neuraxial labour analgesia research to demonstrate the many advances that currently are evident only at the clinical level. Capture of this information is also needed to guide interpretation of the overall importance of the findings in modern labour analgesia trials and clinical care. It should not be assumed, however, that these are the only issues that exist with measurement in labour analgesia trials. Additional issues include the need to standardize outcomes between studies, the need to optimize the methods used to scale responses, the need for validated tools to measure outcomes in some dimensions, e.g., mobility, as well as the need to modify tools used in other dimensions, e.g., labour pain.9 , 24 These issues must also be addressed to provide a solid foundation for evidence-based practice in labour and delivery analgesia.
Lastly, this qualitative study provides important additional insights into the perspectives of women who have either made the decision to receive neuraxial labour analgesia a priori or describe themselves as open to having it if they feel the need during childbirth. Previous work has suggested that pain relief by itself does not guarantee satisfaction with the childbirth experience and that satisfaction in this context is multi-dimensional, relating more to maternal expectations, their supports (including the quality of the relationship between women and their caregivers), and perceived control.9 , 25 - 28 These findings were interpreted to suggest that women do not value pain relief during labour and delivery and that they do not have expectations related to it.29 , 30 The latter interpretation is not supported by our findings. The majority of women in this study shared that they valued pain relief highly and described that pain relief had improved their abilities to cope and to focus on the birth experience. Participants in this study also related that they valued quality relationships with caregivers and had expectations related to pain relief. They shared that a supportive childbirth environment was one that also supported them in their choices related to pain relief. Multiparas, in particular, described expectations and fears related to the accessibility and timely availability of epidural pain relief as well as the importance of being able to freely choose it without health care providers and others making them feel as if they had “wimped out” or had “given up some prize”. Fear of pain and previous experiences with inadequate pain control during labour and delivery have been associated with fear of childbirth and the decision to undergo elective Cesarean delivery.31
Overall, our study findings provide valuable insights into childbearing women’s perspectives regarding the characteristics that constitute quality neuraxial labour analgesia, suggesting the dimensions and specific attributes that must be measured in order to capture this outcome in research. Further work is needed to explore and validate these findings. In addition, this study provides important information related to the perspectives of women who desire or are open to neuraxial labour analgesia, including their expectations and fears surrounding pain relief. These findings have implications for interpretation of existing research as well as antenatal education.
A strength of this study includes using women, who recently delivered with neuraxial labour analgesia, as authorities whose experiences and perspectives could provide insight into the characteristics that constitute quality neuraxial labour analgesia. Women were interviewed shortly after delivery when their experiences were still fresh in their memories. In addition, the participants represented women who had experienced different methods of childbirth and who had both positive and negative experiences with epidural analgesia. Other strengths of this study are the steps undertaken to promote precise and exacting standards. The research team included individuals from different disciplinary backgrounds in order to minimize potential bias ensuing from a single disciplinary perspective. Inter-rater reliability checks were undertaken to ensure consistency in coding. The development of codes and themes were derived inductively from the data, and an extensive audit trail was maintained to document key methods and decisions and the rationale for these.
Limitations are also present. Although not all women were native English speakers, participation required fluency in English. Non-English speaking women might have had different expectations and experiences. Participants delivered in hospitals in a large urban centre where epidural services are readily available. The experiences of women receiving neuraxial analgesia in smaller community hospitals might be different. Notably, some women in our study who resided in small towns shared that they had opted for care in a teaching hospital because of limited access to such resources. Most participants had attended university or a community college and might have different expectations than women who were less educated. Women who were too tired to participate in the study may also have had different experiences and perspectives than the participants. Finally, a second interview with the women, particularly those who had operative deliveries, may have allowed for more in-depth insights into their experiences to emerge.
Notes
QSR International Pty, L. (2002). QSR NVivo 2.0 (Version 2.0) [Computer software].
Gallo A, Faron S. The Use of Patient Controlled Epidural Compared to Continuous Infusion Epidural Analgesia and the Effect in Childbirth Satisfaction 17th International Nursing Research Congress Focusing on Evidence-Based Practice; 19-22 July 2006; Montreal, Quebec, Canada. Available from: CNS http://stti.confex.com/stti/congrs06/techprogram/paper_29819.htm (accessed September, 2009).
References
Birnbach DJ. Advances in labour analgesia. Can J Anesth 2004; 51: R50-2.
Eltzschig HK, Lieberman ES, Camann WR. Regional anesthesia and analgesia for labor and delivery. N Engl J Med 2003; 348: 319-32.
Gambling DR, Yu P, Cole C, McMoreland GH, Palmer L. A comparative study of patient controlled epidural analgesia (PCEA) and continuous infusion epidural analgesia (CIEA) during labour. Can J Anaesth 1988; 35: 249-54.
van der Vyver M, Halpern S, Joseph G. Patient-controlled epidural analgesia versus continuous infusion for labour analgesia: a meta-analysis. Br J Anaesth 2002; 89: 459-65.
Halpern SH, Breen TW, Campbell DC, et al. A multicenter, randomized, controlled trial comparing bupivacaine with ropivacaine for labor analgesia. Anesthesiology 2003; 98: 1431-5.
Hepner DL, Gaiser RR, Cheek TG, Gutsche BB. Comparison of combined spinal-epidural and low dose epidural for labour analgesia. Can J Anesth 2000; 47: 232-6.
Purdie NL, Grady EM. Comparison of patient controlled epidural bolus administration of 0.1% ropivacaine and 0.1% levobupivacaine, both with 0.0002% fentanyl, for analgesia during labour. Anaesthesia 2004; 59: 133-7.
Boselli E, Debon R, Cimino Y, Rimmele T, Allaouchiche B, Chassard D. Background infusion is not beneficial during labor patient-controlled analgesia with 0.1% ropivacaine plus 0.5 microg/ml sufentanil. Anesthesiology 2004; 100: 968-72.
Robinson PN, Salmon P, Yentis SM. Maternal satisfaction. Int J Obstet Anesth 1998; 7: 32-7.
Streiner DL, Norman GR. Devising the items. In: Streiner DL, Norman GR (Eds). Health Measurement Scales - A Practical Guide to Their Development and Use, 2nd ed. Oxford: Oxford University Press; 2003: 14-28.
Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000; 23: 334-40.
Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed. Thousand Oaks, CA: Sage Publication; 1994.
Patton MQ. Qualitative Evaluation and Research Methods. 2nd ed. Newsbury Park, CA: Sage Publications; 1990.
Sandelowski M. Sample size in qualitative research. Res Nurs Health 1995; 18: 179-83.
Altheide DL. Ethnographic content analysis. Qualitative Sociology 1987; 10: 65-77.
Morgan DL. Qualitative content analysis: a guide to paths not taken. Qual Health Res 1993; 3: 112-21.
Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999. p. 134.
Hungler BP, Beck CT, Polit DF. Essentials of Nursing Research: Methods, Appraisals and Utilization, 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001.
Bowling A. Theory of measurement. In: Bowling A (Ed.). Measuring Health. A Review of Quality of Life Measurement Scales, 2nd ed. Buckingham, UK: Open University Press; 2001.
McDowell I. Measuring Health. A Guide to Rating Scales and Questionnaires, 3rd ed. UK: Oxford University Press; 2006.
Bowling A. Measuring Disease, 2nd ed. Buckingham, UK, Open University Press; 2001
Melzack R. The short-form McGill Pain Questionnaire. Pain 1987; 30: 191-7.
McQuay H, Moore A. Pain measurement, study design and validity. In: McQuay, Moore (Eds). An Evidence-Based Resource for Pain Relief. Oxford, UK, 1998: 15
Angle P, Kiss A, Yee J, Halpern S, Murthy Y. The new labor pain scale (LPS): description and properties. Can J Anesth 2006; 53(supplement 1): 26225.
Hodnett E, Simmons-Tropea DA. The Labour Agentry Scale: psychometric properties of an instrument measuring control during childbirth. Res Nurs Health 1987; 10: 301-10.
Collis RE, Davies DW, Aveling W. Randomised comparison of combined spinal-epidural and standard epidural analgesia in labour. Lancet 1995; 345: 1413-6.
Morgan BM, Bulpitt CJ, Clifton P, Lewis PJ. Analgesia and satisfaction in childbirth (the Queen Charlotte’s 1000 Mother Survey). Lancet 1982; 302: 808-10.
Hodnett ED. Pain and women’s satisfaction with the experience of childbirth: a systematic review. Am J Obstet Gynecol 2002; 186: S160-72.
Hodnett ED, Osbourne RW. Effects of continuous intrapartum professional support on childbirth outcomes. Res Nurs Health 1989; 12: 289-97.
Torvaldsen S, Roberts CL, Bell JC, Raynes-Greenow CH. Discontinuation of epidural analgesia late in labour for reducing the adverse delivery outcomes associated with epidural analgesia. Cochrane Database Syst Rev 2004; (4): CD004457
Saisto T, Halmesmaki E. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand 2003; 82: 201-8.
Acknowledgements
This research was supported in part by the R A Gordon Clinical Research Award, Canadian Anesthesiologists’ Society, the Department of Anesthesia, Women’s College Hospital, Toronto, and by The Perinatal Program, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Canada. The authors also thank the women who participated in this study.
Conflicts of interest
None declared.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2010; 57(5).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Angle, P., Landy, C.K., Charles, C. et al. Phase 1 development of an index to measure the quality of neuraxial labour analgesia: exploring the perspectives of childbearing women. Can J Anesth/J Can Anesth 57, 468–478 (2010). https://doi.org/10.1007/s12630-010-9289-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9289-1