Abstract
Purpose
To determine the effect of the Orthopaedic Trauma Association (OTA) pain management guidelines for acute musculoskeletal injuries on opioid prescription sizes, pain control, and refills.
Methods
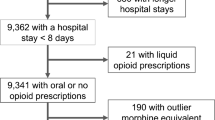
A prospective cohort study was performed at an academic urban level 1 trauma center. 90 patients undergoing outpatient orthopaedic trauma surgery were enrolled before and after the implementation of the OTA pain management guidelines. Adherence to guidelines, pain visual analog scale, and refills were recorded postoperatively and at the 2- and 6-week follow-up visit.
Results
After implementation of the guidelines, the number of patients receiving oxycodone decreased from 100 to 27%, with these patients receiving the less potent hydrocodone, instead. The discharge morphine equivalent dose (MED) decreased from a median (interquartile range) of 225 (169–300) to 140 mg (140–210) (p < 0.001). More patients required refills in the guidelines group (42% vs. 20%), resulting in no difference in total MED prescribed (210 (140–280) vs. 225 (169–307)). Adherence to the guidelines occurred in 66% of patients. As-treated analysis of patients with adherent and non-adherent prescriptions found no detectable difference in pain control, number of opioid pills used, or refills at the 2-week and 6-week follow-up.
Conclusions
In the midst of a national opioid crisis, adoption of the OTA’s pain management guidelines for orthopaedic trauma surgery warrants further research to determine if it’s implementation can reduce the size, variability, and duration of opioid prescriptions.
Level of evidence
Level II, prospective cohort.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Rudd RA, Aleshire N, Zibbell JE, Gladden RM (2016) Increases in drug and opioid overdose deaths—United States, 2000-2014. Cent Dis Control Prev Morb Mortal Wkly Rep 64:1378–1382
Morris BJ, Mir HR (2015) The opioid epidemic. J Am Acad Orthop Surg 23(5):267–271
Attum B, Rodriguez-Buitrago A, Harrison N et al (2018) Opioid prescribing practices by orthopaedic trauma surgeons after isolated femur fractures. J Orthop Trauma 32(3):e106–e111
Lindenhovious ALC, Helmerhorts GTT, Schnellen AC et al (2009) Differences in prescription of narcotic pain medication after operative treatment of hip and ankle fractures in the United States and the Netherlands. J. Trauma: Inj Infect Crit Care 67(1):160–164
Jaynstein J, Donnell A, Chambers L et al (2020) The effect of surgical pain severity, preoperative opioid use and patient characteristics on postoperative opioid prescriptions and refills in orthopedic surgery. Eur J Orthop Surg Traumatol 30(5):781–787
Nataraj N, Zhang K, Guy GP et al (2019) Identifying opioid prescribing patterns for high-volume prescribers via cluster analysis. Drug Alcohol Depend 197:250–254
Chou R, Gordon DB, De Leon-Casasola OA et al (2016) Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain 17(2):131–157
Hsu JR, Mir H, Wally MK et al (2019) Clinical practice guidelines for pain management in acute musculoskeletal injury. J Orthop Trauma 33(5):1
Hernandez NM, Parry JA, Taunton MJ (2017) Patients at risk: large opioid prescriptions after total knee arthroplasty. J Arthroplasty 32(8):2395–2398
Hernandez NM, Parry JA, Mabry TM et al (2018) Patients at risk: preoperative opioid use affects opioid prescribing, refills, and outcomes after total knee arthroplasty. J Arthroplasty 33(7):S142–S146
Stepan JG, Lovecchio FC, Premkumar A et al (2019) Development of an institutional opioid prescriber education program and opioid-prescribing guidelines. J Bone Jt Surg 101(1):5–13
Wyles CC, Hevesi M, Trousdale ER et al (2018) The 2018 Chitranjan S. Ranawat, MD Award: developing and implementing a novel institutional guideline strategy reduced postoperative opioid prescribing after TKA and THA. Clin Orthop Relat Res 477(1):104–113
Thiels CA, Hanson KT, Cima RR et al (2018) From data to practice: increasing awareness of opioid prescribing data changes practice. Ann Surg 267(3):e46–e47
Kahlenberg CA, Stepan JG, Premkumar A et al (2019) Institutional guidelines can decrease the amount of opioids prescribed after total joint replacement. HSS J ® 15(1):27–30
Helmerhorst GTT, Vranceanu AM, Vrahas M et al (2014) Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Jt Surg 96(6):495–499
Vranceanu AM, Bachoura A, Weening A et al (2014) Psychological factors predict disability and pain intensity after skeletal trauma. J Bone Jt Surg 96(3):e20
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no specific disclosures related to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Cyril Mauffrey has the following disclosures: Abbott: Other financial or material support; Carbofix: Research support; Current Opinion in Orthopaedics: Editorial or governing board; DePuy, A Johnson & Johnson Company: Other financial or material support; International Orthopaedics: Editorial or governing board; La Societe Internationale de Chirurgie Orthopedique et de Traumatologie: Board or committee member; Orthopaedic Trauma Association: Board or committee member; osteomed: Research support; Patient safety in surgery: Editorial or governing board; Springer: Publishing royalties, financial or material support; Stryker: Paid consultant; Unpaid consultant; The European journal of orthopaedic surgery and traumatology: Editorial or governing board. Joshua Parry has the following disclosures: The European journal of orthopaedic surgery and traumatology: Editorial or governing board. None of the remaining authors have anything to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chambers, L., Jaynstein, J., Parry, J.A. et al. The effect of the orthopaedic trauma association’s (OTA) pain management guidelines on opioid prescriptions, pain control, and refills in outpatient orthopaedic trauma surgery. Eur J Orthop Surg Traumatol 32, 237–242 (2022). https://doi.org/10.1007/s00590-021-02951-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02951-z