Abstract
Purpose
Retethering of the cord can occur after the initial untethering surgery. Typical neurological manifestations indicative of cord tethering are often difficult to determine in pediatric patients. Patients who had a primary untethering operation are likely to present with some degree of neurological deficits from a previous tethering event, and urodynamic studies (UDSs) and spine images are frequently abnormal. Therefore, more objective tools to detect retethering are needed. This study sought to delineate the characteristics of EDS of retethering, and therefore, could support the diagnosis of retethering.
Methods
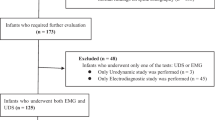
Among 692 subjects who had an untethering operation, data from 93 subjects who had been suspected of retethering clinically were retrospectively extracted. The subjects were divided into two groups, a retethered group, and a non-progression group, according to whether or not surgical interventions had been performed. Two consecutive EDSs, clinical findings, spine magnetic resonance imaging scans, and UDSs before the development of new tethering symptoms were reviewed and compared.
Results
In the electromyography (EMG) study, the appearance of abnormal spontaneous activity (ASA) in new muscles was prominent in the retethered group (p < 0.01). The loss of ASA was more pronounced in the non-progression group (p < 0.01). Specificity and sensitivity of EMG for retethering were 80.4 and 56.5%, respectively. In the nerve conduction study, the two groups did not show differences. The size of fibrillation potential was not different between the groups.
Conclusions
To provide support for a clinician’s decision on retethering, EDS could be an advantageous tool with high specificity when the results are compared to previous EDS results. Routine follow-up EDS post-operatively is recommended as a baseline for comparison at the time when retethering is clinically suspected.




Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data Availability
The datasets from the current study are not publicly available because it is used for further analysis, but are available from the corresponding author on reasonable request.
References
Al-Holou WN, Muraszko KM, Garton HJ, Buchman SR, Maher CO (2009) The outcome of tethered cord release in secondary and multiple repeat tethered cord syndrome. J Neurosurg Pediatr 4:28–36
Alzahrani A, Alsowayan O, Farmer J-P, Capolicchio J-P, Jednak R, El-Sherbiny M (2016) Comprehensive analysis of the clinical and urodynamic outcomes of secondary tethered spinal cord before and after spinal cord untethering. J Pediatr Urol 12(2):101.e1-101.e6. https://doi.org/10.1016/j.jpurol.2015.08.011
Bademci G, Saygun M, Batay F, Cakmak A, Basar H, Anbarci H, Unal B (2006) Prevalence of primary tethered cord syndrome associated with occult spinal dysraphism in primary school children in Turkey. Pediatr Neurosurg 42:4–13
Balasubramaniam C, Laurent J, McCluggage C, Oshman D, Cheek W (1990) Tethered-cord syndrome after repair of meningomyelocele. Childs Nerv Syst 6:208–211
Bowman RM, Mohan A, Ito J, Seibly JM, McLone DG (2009) Tethered cord release: a long-term study in 114 patients. J Neurosurg Pediatr 3:181–187
Cha S, Wang K-C, Park K, Shin H-I, Lee JY, Chong S, Kim K (2018) Predictive value of intraoperative bulbocavernosus reflex during untethering surgery for post-operative voiding function. Clin Neurophysiol 129:2594–2601
Clark VL, Kruse JA (1990) Clinical methods: the history, physical, and laboratory examinations. JAMA 264:2808–2809
Giddens JL, Radomski SB, Hirshberg ED, Hassouna M, Fehlings M (1999) Urodynamic findings in adults with the tethered cord syndrome. J Urol 161:1249–1254
Hall WA, Albright AL, Brunberg JA (1988) Diagnosis of tethered cords by magnetic resonance imaging. Surg Neurol 30:60–64
Hanson P, Rigaux P, Gilliard C, Biset E (1993) Sacral reflex latencies in tethered cord syndrome. Am J Phys Med Rehabil 72:39–43
Hayashi T, Takemoto J, Ochiai T, Kimiwada T, Shirane R, Sakai K, Nakagawa H, Tominaga T (2013) Surgical indication and outcome in patients with postoperative retethered cord syndrome. J Neurosurg Pediatr 11:133–139
Hellstrom WJ, Edwards MS, Kogan BA (1986) Urological aspects of the tethered cord syndrome. J Urol 135:317–319
Hendrick EB, Hoffman HJ, Humphreys RP (1983) The tethered spinal cord. Neurosurgery 30:457–463
Hsieh MH, Perry V, Gupta N, Pearson C, Nguyen HT (2006) The effects of detethering on the urodynamics profile in children with a tethered cord. J Neurosurg Pediatr 105:391–395
Kang PB (2007) Pediatric nerve conduction studies and EMG. In: Blum AS, Rutkove SB (eds) The clinical neurophysiology primer. Springer Science & Business Media, pp 369–389
Kaplan WE, Mclone DG, Richards I (1988) The urological manifestations of the tethered spinal cord. J Urol 140:1285–1288
Khoury AE, Hendrick EB, McLorie GA, Kulkarni A, Churchill BM (1990) Occult spinal dysraphism: clinical and urodynamic outcome after division of the filum terminale. J Urol 144:426–428
Kraft GH (1990) Fibrillation potential amplitude and muscle atrophy following peripheral nerve injury. Muscle & Nerve: Official J Am Ass Electrodiagnostic Med 13:814–821
Lew SM, Kothbauer KF (2007) Tethered cord syndrome: an updated review. Pediatr Neurosurg 43:236–248
McGirt MJ, Mehta V, Garces-Ambrossi G, Gottfried O, Solakoglu C, Gokaslan ZL, Samdani A, Jallo GI (2009) Pediatric tethered cord syndrome: response of scoliosis to untethering procedures. J Neurosurg Pediatr 4:270–274
Muller MP, Tomlinson G, Marrie TJ, Tang P, McGeer A, Low DE, Detsky AS, Gold WLJCid, (2005) Can routine laboratory tests discriminate between severe acute respiratory syndrome and other causes of community-acquired pneumonia? Clin Infect Dis 40:1079–1086
Nafissi S, Niknam S, Hosseini SS (2012) Electrophysiological evaluation in lumbosacral radiculopathy. Iranian J Neurol 11:83
Nazar GB, Casale AJ, Roberts G, Linden D (1995) Occult filum terminale syndrome. Pediatr Neurosurg 23:228–235
Pang D, Wilberger JE (1982) Tethered cord syndrome in adults. J Neurosurg 57:32–47
Pouratian N, Elias WJ, Jane JA, Phillips LH (2010) Electrophysiologically guided untethering of secondary tethered spinal cord syndrome. Neurosurg Focus 29:E3
Raghavan N, Barkovich AJ, Edwards M, Norman D (1989) MR imaging in the tethered spinal cord syndrome. Am J Roentgenol 152:843–852
Roy MW, Gilmore R, Walsh JW (1986) Evaluation of children and young adults with tethered spinal cord syndrome. Utility of spinal and scalp recorded somatosensory evoked potentials. Surg Neurol 26:241–248
Samuels R, McGirt MJ, Attenello FJ, Ambrossi GLG, Singh N, Solakoglu C, Weingart JD, Carson BS, Jallo GI (2009) Incidence of symptomatic retethering after surgical management of pediatric tethered cord syndrome with or without duraplasty. Childs Nerv Syst 25:1085
Sendromlu YTK, Veriler HE (2010) Electrophysiological findings in patients with adult tethered cord syndrome. Turk Neurosurg 20:16–20
Shurtleff D, Duguay S, Duguay G, Moskowitz D, Weinberger E, Roberts T, Loeser J (1997) Epidemiology of tethered cord with meningomyelocele. Eur J Pediatr Surg 7:7–11
Sisson DF, Siegel J (1989) Chloral hydrate anesthesia: EEG power spectrum analysis and effects on VEPs in the rat. Neurotoxicol Teratol 11:51–56
Tamaki N, Shirataki K, Kojima N, Shouse Y, Matsumoto S (1988) Tethered cord syndrome of delayed onset following repair of myelomeningocele. J Neurosurg 69:393–398
Wee A (2002) Surface compound action potentials recorded from different locations on the anterior tibial muscle. Electromyogr Clin Neurophysiol 42:119–123
Whittle IR, Johnston IH, Michael B (1987) Short latency somatosensory-evoked potentials in children—part 1 normative data. Surg Neurol 27:9–18
Winston K, Hall J, Johnson D, Micheli L (1977) Acute elevation of intracranial pressure following transection of nonfunctional spinal cord. Clin Orthop Relat Res 128:41–44
Yamada S, Zinke DE, Sanders D (1981) Pathophysiology of “tethered cord syndrome.” J Neurosurg 54:494–503
Yong RL, Habrock-Bach T, Vaughan M, Kestle JR, Steinbok P (2011) Symptomatic retethering of the spinal cord after section of a tight filum terminale. Neurosurgery 68:1594–1602
Author information
Authors and Affiliations
Contributions
HIS1 and HIS2 contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by HIS1, HIS2, and KHK. The first draft of the manuscript was written by HIS1 and HIS2 and reviewed by KCW and JYL. All authors read and approved the final manuscript (HIS1, Hyun Iee Shin; HIS2, Hyung-Ik Shin).
Corresponding author
Ethics declarations
Ethical standards
The study protocol was approved by the institutional review board (IRB no. 1812–054-993) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Neurosurgery
Hyun Iee Shin is the first author, and Kyu-Chang Wang, Ji Yeoun Lee, and Kyung Hyun Kim are co-authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shin, H.I., Wang, KC., Lee, J.Y. et al. Electrodiagnostic findings of retethering in children with spinal dysraphism. Acta Neurochir 165, 915–925 (2023). https://doi.org/10.1007/s00701-023-05539-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05539-0