Abstract
This study describes the results of an online social support intervention, called “Thrive with Me” (TWM), to improve antiretroviral therapy (ART) adherence. HIV-positive gay or bisexually-identified men self-reporting imperfect ART adherence in the past month were randomized to receive usual care (n = 57) or the eight-week TWM intervention (n = 67). Self-reported ART outcome measures (0–100 % in the past month) were collected at baseline, post-intervention, and 1-month follow-up. Follow-up assessment completion rate was 90 %. Participants rated (1–7 scale) the intervention high in information and system quality and overall satisfaction (Means ≥ 5.0). The intervention showed modest effects for the overall sample. However, among current drug-using participants, the TWM (vs. Control) group reported significantly higher overall ART adherence (90.1 vs. 57.5 % at follow-up; difference = 31.1, p = 0.02) and ART taken correctly with food (81.6 vs. 55.7 % at follow-up; difference = 47.9, p = 0.01). The TWM intervention appeared feasible to implement, acceptable to users, and demonstrated greatest benefits for current drug users.
Similar content being viewed by others
Introduction
Despite evidence of the effectiveness of combination antiretroviral therapy (ART) to substantially slow the progression of HIV disease and reduce onward transmission [1, 2], it is estimated that in the United States (US) approximately 50,000 people become infected with HIV each year [3]; over 20,000 persons living with HIV (PLWH) died in the US in 2010 [4]. Progression of HIV disease and premature deaths among PLWH have been attributed foremost to insufficient engagement in medical care and adherence to HIV treatment regimens [5, 6]. Interventions to improve ART adherence have proliferated in the past decade [7, 8]. Until recently, most ART adherence interventions occurred face-to-face, often in point-of-HIV-care settings (e.g., clinics [9]). However, technology-delivered intervention approaches have gained attention and support [10], particularly for their ability to transcend geographic distance between patients and care providers and lower implementation costs compared to conventional adherence interventions [10, 11].
A review of interventions for PLWH published between 2011 and 2012 that were partially or solely delivered using technology revealed nine ART adherence interventions: three mobile phone counseling interventions, five text (SMS) messaging interventions, and one intervention delivered on a desktop computer (which, along with interventions delivered on laptop computers, are referred to here as “computerized” interventions) [12]. In the computerized intervention, Fisher and his colleagues randomized nearly 600 PLWH living in the US to an interactive computerized intervention grounded in the Information, Motivation, and Behavioral Skills (IMB) model, called LifeWindows, or to the standard-of-care intervention [13]. The LifeWindows intervention consisted of 20 modules from which participants could choose—depending on their individual needs or preferences—to complete during a standard clinic visit over an 18-month period. Although intent-to-treat findings were null, further analysis showed that participants randomized to the LifeWindows intervention who completed at least six sessions and were continuously prescribed medications (i.e., participants who remained “on protocol”) had significantly higher 3-day self-reported ART adherence compared to participants in the control condition. Despite evidence that computerized interventions demonstrate short-term efficacy across multiple health domains [14] and are potentially as effective as face-to-face interventions for reducing sexual risk [15], no other computerized intervention to improve ART adherence, to our knowledge, has been reported in the literature. Thus, more research is needed to understand the extent to which this approach is beneficial for improving treatment outcomes for PLWH [12].
Group education/counseling and peer support are recommended methods to improve ART adherence [9]; however, computerized ART adherence interventions have not harnessed the potential benefits of social interaction between PLWH. Population-based studies of US adults show that 65 % of all Internet-using adults access social networking sites, representing 50 % of the total US adult population [16]. Furthermore, 18 % of US Internet-using adults have gone online in search of others with similar health concerns, with such searches higher among persons living with one or more chronic health conditions (23 %) [17]. A recent study of online social networking website and feature use among 312 PLWH recruited primarily via the Internet showed that a majority of participants taking ART reported using online social networking websites or features [18]. The most common online social networking website was Facebook (61.7 %), followed by Poz.com forums (28.0 %), My Space (21.2 %), and the Body.com forums (10.6 %). Few differences in online social networking use were detected between PLWH with higher (≥95 %) and lower (<95 %) adherence. Participants in the study described their ideal online social networking health website as one that was social, provided relevant HIV information, and provided an emotionally supportive virtual space. However, participants also had concerns about privacy in such contexts and were concerned that some online social spaces provide an opportunity for hostile or negative users who would make the experience less appealing.
Based on the need for more research on computerized interventions for PLWH [12] and the potential for interventions that use social interactive technologies to engage PLWH, the “Thrive with Me” (TWM) intervention was developed and pilot tested in a randomized controlled trial among men who have sex with men (MSM). The primary aims of this study are to: (1) Assess the feasibility of retaining HIV-positive MSM in the TWM intervention; (2) Assess the acceptability and use of the TWM intervention among HIV-positive MSM; and (3) Determine the preliminary efficacy of the TWM intervention to improve ART adherence outcomes compared to an usual care (i.e., no-treatment) control condition.
In addition to these primary aims, we conducted exploratory analyses of intervention acceptability and efficacy of the TWM intervention among current drug-using MSM based on recent findings that current drug use (excluding marijuana) exerted moderation effects on the association between IMB factors and ART adherence (Horvath, Smolenski, and Amico, unpublished manuscript). Specifically, ART information directly influenced ART adherence for current drug users, rather than influencing adherence indirectly through behavioral skills; however, ART information influenced adherence via behavioral skills (as predicted by the IMB model) for non-drug using participants. As the TWM intervention was based on the IMB model, we also examined intervention acceptability and efficacy among current drug users to determine whether they would benefit from this novel approach.
Methods
Procedures and Participants
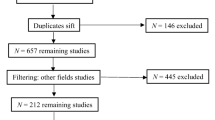
A randomized controlled trial of the TWM intervention was conducted between February and April 2011 (Fig. 1). An a prior goal was set to enroll 120 participants into the TWM study in order to achieve 80 % completion of the final assessment (i.e., at least 50 participants per arm). Participants were recruited mostly through a variety of online venues: 42 % of participants from a prior online survey [18] were contacted via e-mail and rescreened for inclusion in the current study; 21 % were recruited using online banner ads on HIV-related websites (e.g., Poz.com; AIDSMeds.com); 11 % were recruited using online banner ads placed on websites that target the gay/bisexual MSM community; and 1 % via Facebook. Nearly one-quarter (24 %) of the sample came through other sources, such as word-of-mouth or hearing about the study at their clinic. Regardless of how men were informed of the study, all participants were required to complete an online screening survey to determine eligibility for the study.
Self-reported eligibility criteria were: (1) HIV-positive test result; (2) male gender; (3) gay or bisexual sexual orientation; (4) 18 years of age or older; (5) US resident; (6) less than 100 % ART adherence in the past 30 days; (7) availability to participate in the study in the subsequent 16 weeks; and (8) reported being somewhat to very interested (on a 1–4 point scale) in “participating in a health and wellness website in which you would be interacting with other people living with HIV.” We limited enrollment to HIV-positive MSM to promote group cohesion among participants.
Because this was an online social support intervention study in which participants were expected to interact with one another, it was ideal for participants to enter the intervention simultaneously. Therefore, a two-part enrollment process was used to facilitate simultaneous enrollment. First, 145 persons were given a brief description of the purpose of the study and screened for eligibility. Eligible men were informed that they would receive an e-mail in 3–4 weeks (the timeframe the research team estimated that it would take to successfully screen members the participant pool) to finalize the enrollment process. More men were screened for eligibility (n = 145) than was needed to reach the enrollment goal (n = 120) since we anticipated that not all men would return to complete the enrollment process. As anticipated, the screening period was completed in 3 weeks. The participant pool was randomized to the TWM intervention or control group by using a random number generator to assign each case a unique 9-digit number, sorting numbers from low to high, and assigning the first 78 to the TWM intervention and the last 67 to the control condition. More men were randomized to the TWM intervention group given the research team’s prior experience that greater drop-out occurs during the study period among treatment-assigned group members than among the control group [19]. The second phase of the enrollment process was initiated when men in the participant pool were sent the e-mail reminder to complete the consent and enrollment process, resulting in 123 enrolled participants. Importantly, participants were only given information describing the study arm to which they were randomized as to blind them to the requirements and activities of the other arm. Once participants completed the consent and enrolled in the study, they were given immediate access to the baseline survey.
During the intervention period, those randomized to the null control condition were not asked to participate in any activities; however, they were sent one interim e-mail message reminding them of the upcoming follow-up survey. Men randomized to the TWM intervention arm were given access to the intervention for 8 weeks. These intervention participants were first instructed in how to establish their online profile, and given a brief written description of how to use the website. Participants’ use of selected intervention components (including logging into the website, writing or responding to posts, updating their medication adherence graph, viewing articles, links, and videos; see description below) were automatically recorded during the study period to gauge intervention use. Participants received one “Thrive Point” for each day they interacted with the intervention; those who received 5 or more “Thrive Points” in a week were entered into a weekly raffle of $25. To encourage participation and discussion, study staff posted a weekly question to the group (called the “Question of the Week”) asking participants to share their opinion on various aspects of living with HIV. Because the aim was to assess how participants would naturally engage with the TWM intervention, participants were not required to interact with any component of the intervention. The TWM intervention was monitored daily by study staff to identify any concerns (e.g., hostile interactions; suicidal ideation; ART or HIV-related misinformation) and to respond to participants’ questions or concerns about the intervention.
Following the eight-week intervention period, TWM intervention (but not control) participants completed the “post-intervention” survey to assess their perceived information and system quality of, as well as overall satisfaction with, the intervention. One month later, all participants completed the “follow-up” survey to assess adherence outcomes. Remuneration amounts for each of the surveys was as follows: Baseline: $20; Post-intervention: $25; Follow-up: $35. In addition, a $10 bonus was paid to participants who completed all assessments. All study procedures were approved by the University of Minnesota Institutional Review Board.
Intervention Description
The TWM intervention had three main components. First, the TWM homepage consisted of an interface for participants to asynchronously interact with one other by posting messages and replying to other participants’ messages (Fig. 2). Once written, any message could immediately be viewed by all participants without first subjected to review by study staff. The homepage also contained a summary of the participant’s online profile, a graph of the number of “Thrive Points” earned in the present week, and links to other website content.
Second, a medication adherence page (Fig. 3) allowed participants to input (or update) their current antiretroviral medications, and indicate the dosing and frequency of administration. Participants were encouraged to update their adherence level daily, and were shown a private graph of their weekly adherence level. In addition, participants were given the option to receive e-mail or SMS text-based reminders to take their medications as scheduled. Those who opted for this service could update their medication adherence graph by responding to a text asking them to indicate their adherence to each dose.
The third major component of the intervention was intervention content addressing issues about living with HIV (Fig. 4). Intervention content took one of 3 forms: (a) video segments provided by the Positive Project (http://www.thepositiveproject.org/#) were chosen based on a prior analysis of topics HIV-positive MSM would find most interesting [18]; (b) brief articles about HIV-related topics and medication adherence written by study staff; and (c) links to other HIV-related websites and webpages.
Measures
Demographic Characteristics
Demographic characteristics included age (in years); how long participants had been living with HIV (in years); education (years of school); race (White, Black, Multi-racial); ethnicity (Hispanic identity); residency (from rural residency to central core of a large city); current employment status (part-time, full-time, disabled, unemployed, retired); and whether the participant was currently in school (Table 1).
Psychosocial Characteristics
Internet knowledge was assessed using the iKnow scale, which is a 14-item measure of one’s knowledge of Internet-related terms and how to perform Internet-related tasks [20]. Among 300 undergraduate and graduate-level students, Chronbach’s alpha for the iKnow measure was 0.94 (M = 54.30) [20]. In this sample of HIV-positive MSM, Chronbach’s alpha was 0.89. Depression was measured with the 10-item Center for Epidemiologic Studies—Depression Scale (CES-D) [21], a widely used measure of depression in research studies (α = 0.89 for this sample). A cut-off score of 10 or higher (range 0–30) was used to categorize men as having significant depressive symptoms [22]. The Perceived Stress Scale was used as a measure of the extent to which life situations are perceived as stressful and has been shown to have good internal validity (α = 0.84–0.86) among samples of college-aged students (Ms = 23.18–23.67) and cigarette smokers (M = 25.0) [23]. Chronbach’s alpha for the Perceived Stress Scale for this sample of PLWH was 0.91. The Life Chaos Scale is a 6-item measure of whether someone has a stable and predictable lifestyle and has been shown to be psychometrically adequate among PLWH in a prior study (M = 17.7; α = 0.67) [24]. Chronbach’s alpha for the Life Chaos Scale among this sample of PLWH was 0.68. The HIV Stigma scale developed by Emlet [25] was used to measure subjective perceptions of stigma by PLWH. A prior study showed that the scale was particularly useful for older PLWH (M = 23.02 for 50+ year olds vs. 25.18 for 20–39 year olds) [25]; Chronbach’s alpha for this sample on the HIV Stigma Scale was 0.91.
The alcohol use disorders identification test (AUDIT) [26] was used to determine whether participants were at risk for alcohol dependency or hazardous alcohol consumption. Prior research showed that 92 % of persons who were diagnosed as having harmful or hazardous alcohol use scored 8 or more on the AUDIT (the cut-off score for harmful and hazardous alcohol use) [26]. In addition, participants were asked to indicate the number of times they had used any of the following 10 illicit drugs in the past 30 days: codeine purchased on the street, powder cocaine, crack cocaine, amphetamines, methamphetamines, GHB, ketamine, ecstasy, heroin, or cocaine and heroin mixed together.
Intervention Acceptability
Items used to assess intervention acceptability are shown in Table 2. Factors from the Information Systems Success Model (ISSM) proposed by DeLone and McLean [27, 28] were adapted to assess users’ perception of the information quality, system quality, perceived usefulness and overall satisfaction with the TWM intervention. Information quality refers to users’ perceptions of the quality of the information contained on the TWM website. System quality refers to users’ perceptions of how easily the TWM website was to navigate and the technical responsiveness of the TWM intervention. Perceived usefulness reflects how the TWM intervention was perceived to impact participants’ health behaviors.
ART Medication Use and Adherence
Participants were asked to self-report the number of different HIV medications they were prescribed, and how many daily doses of their HIV medications they were prescribed. ART regimen complexity was assessed by grouping participants into four categories (from least complex to most complex): (a) one medication once a day; (b) two or more medications once a day; (c) one or two medications twice a day; or (d) three to four medications two or more times a day.
Based on best practices for measuring self-reported ART adherence [29] and a study showing strong associations between similar self-report measures and more objective ART adherence measures [30], three primary self-reported adherence outcomes were assessed for the purpose of this study: (a) The percentage of time ART was correctly taken as prescribed in the past 30 days; (b) The percentage of time ART was taken within 2 h of the scheduled dose in the past 30 days; and (c) The percentage of time ART was taken correctly with food in the past 30 days. For each item, participants responded using a pull-down menu with response options that ranged from 0 to 100 in 1 point increments.
Analysis Plan
Intervention feasibility is described at the percentage of participants recruited and retained at each assessment point [31]. Demographic and psychosocial characteristics, intervention acceptability and satisfaction items, intervention component utilization, and baseline and follow-up ART adherence outcomes were summarized using descriptive statistics (i.e., frequencies, percentages, means, and standard deviations), and analyzed with the appropriate nonparametric (Fisher’s exact or Chi square) or parametric (Students t test or analysis of variance) statistic.
Adherence outcomes were examined in two ways. First, pre-to-post intervention ART adherence improvement was calculated by subtracting baseline adherence scores from follow-up adherence scores for each ART adherence outcome (i.e., calculating a “difference score”) [32, 33]. Mean difference scores between the TWM intervention participants and control participants for each of the three ART adherence item were examined with Student’s t test. Second, participants’ follow-up assessment ART adherence score was dichotomized as either below 90 % ART adherence or 90 % or higher ART adherence, and analyzed using non-parametric tests (i.e., Fisher’s exact or Chi square). All adherence outcomes were assessed for the overall sample, for men who did not report using any of the 10 illicit drugs (described above) in the past 30 days, and among men who reported using one or more of the 10 illicit drugs in the past 30 days.
All available participant data were included in the analyses as originally randomized irrespective of the level of intervention engagement or completion. Since overall survey completion at each time point was high, participants with missing data were excluded from analysis. Cohen’s d was calculated to assess the magnitude of the treatment effect on ART adherence items. Statistical significance was set at p < 0.05.
Results
Study Retention and Demographic Characteristics
Of the 145 men who met inclusion criteria and expressed interest in the study, 123 consented and were randomized to either the intervention (n = 66) or control (n = 57) arm (Fig. 1). After the eight-week intervention period, 57 men in the intervention arm completed the post-intervention assessment (86.4 % retention). Most men in the intervention (87.9 %) and control (93.0 %) arm completed the follow-up assessment, for an overall retention rate of 90.2 %.
Baseline demographic characteristics for the total sample, and by treatment and control arm, are presented in Table 1. On average, participants were 43 years of age, White, had been living with HIV for 13 years, and had completed some college. Men were recruited from 30 US states and the District of Columbia (not shown). A large proportion of men reported depressive symptoms, and similarly high levels of stigma and life chaos compared to other samples of PLWH [24, 25]. Men were relatively knowledgeable about Internet-related tasks, although participants randomized to the control condition were somewhat more likely to report higher Internet knowledge than those in the treatment arm (p = 0.05). Approximately one-quarter of men reported hazardous or dependent alcohol use, and 17.5 % (n = 20) of participants reported current drug use (excluding marijuana).
Chi square analysis showed that control arm participants reported more complex ART dosing regimens than those in the intervention group (p = 0.01); however, the complexity of dose regimen was not associated with baseline overall ART adherence score (F[3,121] = 0.71, p = 0.55) or overall ART difference score (F[3, 105] = 0.40, p = 0.75).
No significant differences in demographics, psychosocial, or adherence factors were found between participants who did (n = 110) and did not (n = 13) complete the follow-up survey.
TWM Intervention Use
Among the 66 men randomized to the TWM intervention arm, 61 (92.4 %) entered the intervention site at least once during the study period. Participants who entered into the TWM intervention site used 7,754 intervention components, including logging on to the intervention 1,825 times, posting to the intervention 1,181 times, updating their medication graph 3,935 times, viewing articles about living with HIV 106 times, viewing information about website rules and functions 204 times, viewing the question of the week and information about the chat discussions 337 times, viewing videos 99 times, and viewing links to other websites 67 times. Frequency of use of intervention components per individual ranged from 2 to 381 times. Altogether, 38 participants (58 % of the TWM intervention group) used 100 or more intervention components during the 8-week intervention period.
The most frequently read articles that addressed living with HIV were those that provided information on the relationship between medications and emotions, as well as an article on drug assistance programs. Videos with the highest number of hits were those about managing stress, coping with HIV and seeking social support, and opportunistic infections. In addition, 15 participants (24.6 %) opted to use the text messaging service, resulting in 2,100 text messages sent and received.
TWM Intervention Acceptability and Satisfaction
Mean intervention acceptability and satisfaction ratings for participants randomized to the intervention arm and who completed the post-intervention survey are shown in Table 2. For the total sample of intervention-assigned men, average ratings of 5 or higher were reported. Highest mean scores were reported for the perceived credibility of the TWM intervention (M = 6.2), how easy the TWM intervention was to comprehend (M = 6.1), and how quickly the text and graphics loaded (M = 6.1). Although still above 5, the lowest mean ratings were given on items that addressed the usefulness of the intervention in participant’s lives (Ms = 5.0–5.3).
When asked what was liked most about the intervention, men overwhelmingly indicated that it build a sense of community with other men living with HIV: “Opportunity to meet other POZ gay men.”; “The ability to talk about the issues that people with HIV deal with.”; “I think it is a great idea for those without a support network.”; and “It was interesting to see how others are handling their HIV.” In addition, many men appreciated receiving the medication reminders: “Medication reminder via text—the most compliant ever in taking meds”; “using the text feature. This feature allows for better adherence”. However, the average rating for “Using Thrive with Me is frustrating” was 5.2 (reverse coded), indicating that some men found the experience frustrating. Occasionally, technical glitches occurred during the course of the intervention, obstructing men from tracking their medications correctly and obtaining participation points. When asked about what they liked least about the intervention, the most common response was problems in these areas: “Sometimes the Thrive points did not calculate correctly”; and “Glitches with the med tracker.” Some participants also noted that they disliked negative comments from other group members: “the negative attitude of the majority of the participants”; “select member complaints about the site instead of constructive criticism.”
TWM Intervention Effects for the Overall Sample
The means and standard deviations of baseline and follow-up adherence outcomes are shown in Table 3. Analysis of mean ART difference scores showed that men in the intervention arm improved across each of the three adherence measures, while adherence scores for men in the control arm decreased over time (Fig. 5). There was not a significant difference in improvement for overall ART adherence for men in the intervention (M[difference score] = 0.54, SD = 25.2) compared to those in the control condition (M[difference score] = −3.2, SD = 24.5), t(107) = 0.79, p = 0.43, Cohen’s d = 0.15. However, there was a trend for greater improvement in taking ART within 2 h of the scheduled dose for men in the intervention arm (M[difference score] = 6.6; SD = 29.3) compared to men in the control arm (M[difference score] = −3.0; SD = 29.6), t(105) = 1.68, p = 0.095, Cohen’s d = 0.33. Furthermore, men in the intervention arm (M[difference score] = 8.3, SD = 32.6) reported significantly greater improvement in taking ART correctly with food compared to those in the control arm (M[difference score] = −3.7, SD = 27.2; t[105] = 2.06, p = 0.04, Cohen’s d = 0.40).
When participants were dichotomized as achieving 90 % ART adherence or not at the follow-up assessment (Table 4), a significant group difference was not found for the total sample in overall ART adherence (74.1 % for TWM vs. 71.2 % for Control), taking ART within 2 h of their scheduled dose (68.4 % for TWM vs. 53.9 % for Control), or for taking ART correctly with food (64.9 % for TWM vs. 61.5 % for Control).
TWM Acceptability Ratings and Intervention Effects for Current Drug Users
Just under one-fifth (17.5 %) of the sample (n = 20; intervention = 9, control = 11) reported using illicit drugs (excluding marijuana) in the past 30 days (Table 1). Current drug-using MSM randomized to the intervention arm reported similar intervention acceptability ratings as the overall sample and to non-drug using men (Table 2). In addition, current-drug using participants used an average of 147 intervention components (range 5–280) with 7 of the 9 current drug-using MSM randomized to the intervention group reporting using more than 100 intervention components during the 8-week intervention period. Intervention use of non-drug-using participants was similar to that of the overall sample (since most participants did not report current drug use).
Mean ART difference scores (Fig. 5) for current drug users showed that those in the intervention arm reported significantly higher overall ART adherence (Intervention: M[difference score] = 7.1, SD = 22.1; control: M[difference score] = −24.0, SD = 30.5; t[17] = 2.52, p = 0.02; Cohen’s d = 1.17) and ART taken correctly with food (Intervention: M[difference score] = 22.7, SD = 32.5; Control: M[difference score] = −25.2, SD = 37.6; t[17] = 2.95, p = 0.01; Cohen’s d = 1.36) than participants in the control condition. In addition, there was a trend for current drug users randomized to the intervention arm to report a higher percentage of ART taken within 2 h of scheduled dose compared to control group members (Intervention: M[difference score] = 11.9, SD = 37.8; Control: M[difference score] = −23.5, SD = 37.2; t[17] = 2.05, p = 0.06; Cohen’s d = 0.94).
The dichotomous analysis (Table 4) revealed that a higher proportion of drug-using men in the treatment arm maintained 90 % ART adherence at follow-up compared to those in the control arm for overall ART adherence (88.9 % for TWM vs. 30.0 % for Control, p = 0.01) and for taking ART within 2 h of the scheduled dose (77.8 % for TWM vs. 10.0 % for Control, p = 0.01). In contrast, ART adherence outcomes were not significantly different between treatment and control conditions for non-drug using men in any of the analyses (see Fig. 5 and Table 4).
Discussion
This is the first study, to our knowledge, to assess the feasibility, acceptability, and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. Three main findings were evident from this study of MSM. First, it was feasible to recruit and retain participants in the TWM study, with overall high retention rates. Overall retention in the TWM study was 90 %, with only a slight difference in retention between those randomized to the intervention (88 %) and control (93 %) arms. Second, users of the TWM intervention perceived it to be acceptable with respect to its overall information and system quality, perceived usefulness, and overall satisfaction. Third, the primary analyses using difference scores showed that the TWM intervention may have helped some users to refine their adherence behaviors, including taking their medications correctly with food and taking it within 2 h of their scheduled dose time. However, post-hoc analyses showed a dramatic improvement in adherence behaviors among a small group of participants who reported current drug use. These findings are discussed in greater detail below.
Examination of use patterns showed that participants assigned to the TWM intervention engaged with intervention components without a requirement that they do so. Of the men randomized to the TWM intervention arm and who entered the intervention at least once, almost two-thirds used the intervention components (among components that were tracked during the course of the study) 100 or more times. Given that the primary goal of the intervention was to improve ART adherence and foster support among group participants, it was encouraging that the most widely used features of the intervention were the medication adherence tracking graph and message posting on the intervention homepage. Participants also stated in their written evaluations of the TWM intervention that these were the most appreciated intervention components, which may have lead them to rate the intervention highly in terms of information and system quality, perceived usefulness, and overall satisfaction (Ms > 5 out a possible 7). Overall, it appears that the TWM intervention was successful in fostering peer support among many group members and in providing self-monitoring tools to support and strengthen ART adherence.
However, just as some men appreciated the support from TWM community members, other men found negative comments from some users discouraging. This is a particularly challenging aspect of online peer-to-peer support interventions, since expression of negative thoughts and feelings by group members may potentially adversely affect other group members and dampen their enthusiasm to participate in such interventions. These findings are consistent with those of a survey of PLWH that revealed that participants’ ideal online social networking health website was one that is social and supportive, although many feared that online peer exchange venues provided opportunities for users to express negativity [18]. Participants in the survey study recommended that online social networking spaces be monitored to address negative comments. As such, we attempted to provide a supportive space in the TWM intervention, while monitoring the website daily for potential hostile remarks between participants. Although less salient to participants than their appreciation of peer-to-peer support and the ART adherence self-monitoring tool, this approach to intervention monitoring may have contributed to participants’ overall satisfaction with the intervention.
The TWM intervention experienced several technical glitches during the intervention trial, of which the most common pertained to the medication adherence tracker and reminder system and the tracking of “Thrive Points.” Study staff attempted to address technical problems as they arose and to assure participants that actions were being taken to remedy problems that arose. Future technology-based intervention trials must allocate sufficient time and resources to the testing and identification of resolvable “glitches” before the intervention is officially launched, as well as to address new technical problems that may arise after the intervention is launched. Although usability testing was conducted during the development of the TWM intervention to identify technical problems, we did not anticipate technical issues that arose as a result of a higher number of users accessing the intervention. Thus, we recommend that testing should include a period in which multiple individuals simultaneously use the intervention for several days to weeks. Despite these technical problems, participants rated the intervention positively, suggesting that the technical problems did not exert a significant effect on users’ overall experience.
Results suggest that the TWM intervention was successful in helping some participants refine their adherence behaviors, although it did not appear to significantly influence overall self-reported ART adherence for the entire sample of MSM. Although disease progression is most predicted by sub-standard or non-adherence to ART [34], emerging evidence suggest that even occasional non-adherence may provide opportunity for viral replication that may underlie lower life expectancy among PLWH compared to the general population [35]. Therefore, interventions that show evidence for assisting participants in refining their adherence behaviors may be increasingly important to reduce morbidity and mortality among PLWH compared to the general population.
A post-hoc examination of current drug users in the TWM study showed significant group differences favoring the TWM intervention arm in overall ART adherence, as well as in refining ART adherence behaviors. Results favored the TWM intervention over the null-control condition regardless of whether the primary outcomes were assessed as difference scores or dichotomized. This set of findings points to a number of intriguing avenues for further study. For example, did drug-using MSM benefit more from the TWM intervention than their non-drug-using counterparts because they processed information (in the form of articles or videos) on the intervention website differently? Alternatively, it may have been that the non-drug-using participants provided high levels of support and suggestions for overcoming adherence barriers to drug-using participants, and therefore higher benefits were observed in drug users. A third alternative is that current drug using participants started with lower baseline ART adherence and had greater opportunity for improvement during the course of the intervention, which was somewhat supported by the results of this intervention (see Table 3).
This pilot study was limited by a number of factors. First, the TWM intervention was conducted under highly controlled conditions and it is unknown how the intervention would function or be used by the target population in less controlled (i.e., “real-world”) settings. However, given the early stage of investigation of this approach to intervention, such controls were necessary to determine if this approach would be feasible and acceptable to the target population. Second, because a two-part enrollment process was used to facilitate simultaneous enrollment into the intervention, men who were more motivated to participate in the study and engage with the intervention may have been enrolled than would be the case if a single-step enrollment process was used. However, the two-stage enrollment process did allow participants in the TWM intervention arm to enter into the intervention at approximately the same time and allowed us to restrict participants’ knowledge of the other study arm. The research team weighed the pros and cons of each approach and opted for the two-stage enrollment process, as it provided the greatest benefits. Third, self-report measures of adherence may not accurately reflect actual adherence levels and should be viewed with caution when interpreting the results of the study. Forth, a relatively small number of participants were recruited for the purpose of this pilot study, and an even smaller proportion of the overall sample reported current drug use. Thus, larger studies are needed to establish the efficacy of this approach with a wider sample of PLWH and among particular subgroups (e.g., drug users). Finally, the intervention period was relatively short compared to the length of prior ART interventions (2 vs. 5 months for the average ART adherence intervention period [36]); this intervention approach described here should be tested for a longer period of time.
Despite these limitations, this is the first study to demonstrate feasibility and acceptability of an online peer-to-peer social support ART adherence intervention among HIV-positive MSM. Moreover, the results showed preliminary efficacy of the intervention, particularly among drug-using MSM. These findings support continued efforts to pursue this innovative approach to address ART non-adherence among HIV-positive MSM, which remains a critical public health priority. Also, adapting this approach to other populations of PLWH (e.g., racial and ethnic minorities, youth, and women), as well as groups who would benefit from adherence-based interventions (e.g., persons taking pre-exposure prophylaxis [37]), is necessary to determine if similar results will be found among other priority populations.
References
The Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–9.
Cohen MS, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Prejean J, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6(8):e17502.
Centers for Disease Control and Prevention, HIV Surveillance Report: Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 2010, 2012.
Mills EJ, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3(11):e438.
Mugavero MJ, et al. Failure to establish HIV care: characterizing the “no show” phenomenon. Clin Infect Dis. 2007;45(1):127–30.
Simoni J, et al. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S23–35.
Simoni J, et al. Antiretroviral adherence interventions: a review of current literature and ongoing studies. Top HIV Med. 2003;11(6):185–98.
Thompson MA, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an international association of physicians in AIDS care panel. Ann Intern Med. 2012;156(11):817–33.
Saberi P, Johnson MO. Technology-based self-care methods of improving antiretroviral adherence: a systematic review. PLoS One. 2011;6(11):e27533.
Page TF, et al. A cost analysis of an internet-based medication adherence intervention for people living with HIV. J Acquir Immune Defic Syndr. 2012;60(1):1–4.
Pellowski JA, Kalichman SC. Recent advances (2011–2012) in technology-delivered interventions for people living with HIV. Curr HIV/AIDS Rep. 2012;9(4):326–34.
Fisher JD, et al. Computer-based intervention in HIV clinical care setting improves antiretroviral adherence: the LifeWindows project. AIDS Behav. 2011;15(8):1635–46.
Portnoy DB, et al. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47(1):3–16.
Noar SM, Black HG, Pierce LB. Efficacy of computer technology-based HIV prevention interventions: a meta-analysis. AIDS. 2009;23(1):107–15.
Madden M, Zickuhr K. 65 % of online adults use social networking sites. 2011. http://pewinternet.org/Reports/2011/Social-Networking-Sites.aspx, Pew Research Center: Washington DC.
Fox S. Peer-to-peer healthcare: many people-especially those living with chronic or rare diseases-use online connections to supplement professional medical advice. Washington DC: Pew Research Center’s Internet & American Life Project; 2011.
Horvath K, et al. Technology use and reasons to participate in social networking health websites among people living with HIV in the US. AIDS Behav. 2012;16(4):900–10.
Rosser BS, et al. Reducing HIV risk behavior of men who have sex with men through persuasive computing: results of the Men’s INTernet Study-II. AIDS. 2010;24(13):2099–107.
Potosky D. The internet knowledge (iKnow) measure. Comput Hum Behav. 2007;23(6):2760–77.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1992;1:385–401.
Zhang W, et al. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Wong MD, et al. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22(9):1286–91.
Emlet CA. Measuring stigma in older and younger adults with HIV/AIDS: an analysis of an HIV stigma scale and initial exploration of subscales. Res Soc Work Pract. 2005;15:291–300.
Saunders JB, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88(6):791–804.
DeLone WH, McLean ER. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst. 2003;19(4):9–30.
DeLone WH, McLean ER. Information systems success: the quest for the dependent variable. Inf Syst Res. 1992;3(1):60–95.
Simoni J, et al. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. AIDS. 2002;16(2):269–77.
Begg C, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA. 1996;276(8):637–9.
Dimitrov DM, Rumrill PD Jr. Pretest-posttest designs and measurement of change. Work. 2003;20(2):159–65.
Gottman JM, Rushe RH. The analysis of change: issues, fallacies, and new ideas. J Consult Clin Psychol. 1993;61(6):907–10.
Bangsberg DR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–3.
Pasternak AO, et al. Modest non-adherence to antiretroviral therapy promotes residual HIV-1 replication in the absence of virological rebound in plasma. J Infect Dis. 2012;206(9):1443–52.
Rivet Amico K, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a Research Synthesis of Trials, 1996 to 2004. J Acquir Immune Defic Syndr. 2006;41(3):285–97.
Anderson PL, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125.
Acknowledgments
We wish to thank the participants of this study for their time and effort. We also thank Tony Miles at the Positive Project for allowing us to use segments from their video archive for the purpose of this study. This study was funded by the National Institute of Mental Health (5R34MH083549).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horvath, K.J., Michael Oakes, J., Simon Rosser, B.R. et al. Feasibility, Acceptability and Preliminary Efficacy of an Online Peer-to-Peer Social Support ART Adherence Intervention. AIDS Behav 17, 2031–2044 (2013). https://doi.org/10.1007/s10461-013-0469-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0469-1