Abstract
Kawasaki disease (KD) is an acute febrile systemic vasculitis, and the cause of KD is not well understood. It is likely due to multiple interactions between genes and environmental factors. The development of genetic association and genome-wide association studies (GWAS) has opened an avenue to better understanding the molecular mechanisms underlying KD. A novel ITPKC signaling pathway was recently found to be responsible for the susceptibility to KD. Furthermore, the GWAS demonstrated the functionally related susceptibility loci for KD in the Caucasian population. In the last decade, the identification of several genomic regions linked to the pathogenesis of KD has made a major breakthrough in understanding the genetics of KD. This review will focus on genetic polymorphisms associated with KD and describe some of the possible clinical implications and molecular mechanisms that can be used to explain how genetic variants regulate the pathogenesis in KD.
Similar content being viewed by others
Introduction
Kawasaki disease (KD)1 is an acute, febrile systemic vasculitis that was first described by Kawasaki et al2. In developed countries, it is the leading cause of acquired heart diseases in children, though its etiology remains unknown3, 4, 5. KD occurs worldwide, most commonly in Asian countries, and mainly affects children less than 5 years of age. Japan, Korea, and Taiwan region have the highest incidence of KD ranging from 69 to 213 cases per 100 000 children under 5 years of age6, 7, 8. The incidence of KD has been increasing globally in recent years. The most serious complications of KD are coronary artery lesions (CAL), including myocardial infarction, coronary artery fistula formation9, coronary artery dilatation/ectasia and coronary artery aneurysm10.
The clinical characteristics of KD patients include prolonged fever longer than five days, diffuse mucosal inflammation, bilateral non-purulent conjunctivitis, dysmorphous skin rashes, indurative angioedema over the hands and feet, and cervical lymphadenopathy. In addition to the diagnostic criteria, there is a broad range of non-specific clinical features, including irritability, uveitis, aseptic meningitis, cough, vomiting, diarrhea, abdominal pain, gallbladder hydrops, urethritis, arthralgia, arthritis, hypoalbuminemia5, liver function impairment and heart failure4, 11.
Although the clinical features of KD are recognizable, the immuno-pathogenetic mechanism of this disease is still unclear, particularly the causative agent for CAL formation. Transforming growth factor-beta (TGF-β) is a candidate gene for KD pathogenesis because TGF-β-mediated T-cell activation and cardiovascular remodeling are regarded as important features of KD. Indeed, genetic polymorphisms of the TGF-β pathway, including TGFB2, TGFBR2, and SMAD3, are associated with susceptibility to KD and development of CAL in the European and US populations12. In the Asian population, we reported that monocytosis, eosinophilia, and eosinophil-related Th2 immune response (especially, plasma level of IL-5) are associated with CAL formation and/or initial intravenous immunoglobulin (IVIG) treatment response13, 14, 15, 16. Immune-related genes, such as CTLA-4, CASP3 and ITPKC, have also been suggested to influence the susceptibility to and the clinical status of KD14, 15, 17, 18, 19, 20, 21.
The efficacy of IVIG administered during the acute phase of KD to reduce the prevalence of coronary artery abnormalities has been well established22. However, the mechanism of action of IVIG is still elusive. IVIG appears to have a generalized anti-inflammatory effect. Possible mechanisms of IVIG include the modulation of cytokine production, neutralization of bacterial super-antigens, suppression of antibody synthesis and inflammatory markers (CD40L, nitric oxide and iNOS expression)23, 24, and provision of anti-idiotypic antibodies9, 13, 16.
The role of genetic polymorphisms in immune-related genes in the susceptibility to Kawasaki disease
The higher incidence of KD in Asia, in conjunction with a higher incidence of the disease in Asian descendants compared with other ethnic populations in the United States and Europe, suggests that a genetic predisposition might play an important role in the susceptibility to this disease3, 4, 7, 10, 25, 26, 27. There is also evidence that the incidence of KD is higher among siblings than in the general population28. Additionally, KD has a higher incidence rate among males than in females5, 19. Further evidence supports the hypothesis that genetic factors contribute to the susceptibility to KD17. For example, a number of genes have been reported to have significant associations with the susceptibility to KD in different populations. For instance, single nucleotide polymorphisms (SNPs) in the monocyte chemoattractant protein 1 (MCP-1)29, IL-1030, 31, 32, CD40L33, IL-426, CASP320, 34, IL-1835, IL-1B36, HLA-E37, C-C chemokine receptor 5 (CCR5)38, and inositol 1, 4, 5-trisphosphate 3-kinase C (ITPKC)21, 39 have been reported to be associated with the development of KD. In early 2011, Shimizu et al12 first reported that genetic polymorphisms of TGFB2, TGFBR2, and SMAD3 are associated with susceptibility to Kawasaki disease and the development of coronary artery lesions. Taken together, these findings suggest that multiple polymorphic alleles influence KD susceptibility and that different ethnic populations, which have distinct allelic expression patterns, and different sexes may have different susceptibilities to KD3. Interestingly, there are some genes associated with susceptibility to KD, but not CAL formation. We hypothesize that the genes responsible for susceptibility and CAL formation may be distinct20, 39, 40.
Association between the genetic polymorphisms and CAL formation in KD
All KD patients were treated with IVIG, 2 g/kg in a single infusion for 12 h, together with aspirin22. This therapy was within 10 d of illness and, if possible, within 7 d of illness. From a serial analysis of coronary artery lesions (n=341) in Chang Gung Memorial Hospital-Kaohsiung20, 35% of KD patients had dilatation during the acute phase, 17.2% had dilatation one month after disease onset, 10.2% still had dilatation at two months of follow-up, and 4% had persistent CAL for more than one year39.
The most commonly used definition of CAL (also known as coronary artery abnormality, CAA or CALs) is based on the Japanese Ministry of Health criteria: maximum absolute internal diameter >3 mm in children younger than 5 years of age or >4 mm in children 5 years and older, or a segment 1.5 times larger than an adjacent segment, or the presence of luminal irregularity41, 42, 43. If the body surface area is known, then coronary arteries are normalized to this surface area and expressed as standard deviation units from the mean (Z scores)44. Several studies have analyzed CAL using other methods, including the aorta route dimension12 and transient CAL (although the definition of “transient” varies among studies, from 30 d to 6–8 weeks after disease). Interestingly, some results have indicated that the genetic association was observed only with susceptibility, not with CAL formation. However, other studies have revealed inconsistent results (Table 1)45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57. These results indicate that the genes responsible for susceptibility and CAL formation may be different between populations7, 32, 37, 38, 58, 59, 60. Recently, several candidate genes have been proposed for the susceptibility to KD or the formation of CAL in different populations. Although there is evidence to support a role for each candidate gene in the susceptibility to KD and/or development of CAL, there is also evidence that cannot be easily fitted into any (Table 2). Most studies addressing this question are plagued with inconsistencies. First, the sample size varies dramatically across studies. Hence, a small sample size may not have sufficient power to detect minor genetic effects. Second, it is becoming clear that there are different genetic backgrounds within populations that due to variations in allele frequencies or heterogeneity of the phenotype, may also influence the results. Third, the incidence of KD in Asia is much higher than in other places. Thus, the role of environmental factors or infectious agents in the development of KD should also be considered.
Genetic polymorphisms of the ITPKC signaling pathway in patients with Kawasaki disease
A major advancement in the genetic study of KD was provided by the discovery of ITPKC. ITPKC is an important molecule in the regulation of T cell activation, and it may function as a calcium channel modulator21. In 2008, Onouchi and colleagues first identified the functional polymorphism of ITPKC (rs28493229) that is significantly associated with the susceptibility to KD and coronary artery lesions in both Japanese and US children21, 61. Using cell-based functional studies, Onouchi et al further indicated that the risk allele (C allele) of ITPKC reduces the splicing efficiency of the ITPKC mRNA that, in turn, may contribute to the hyperactivation of Ca2+-dependent NFAT pathways in T cells21. The identification of ITPKC has had an enormous effect on the field of genetic association studies of KD. These novel insights into genetic mechanism clearly provide a new understanding of the pathogenesis of KD. In contrast, the results obtained from the replication studies in the Taiwanese populations are strikingly controversial62, 63. A similar approach was taken by Chi et al62. These authors genotyped 385 KD patients and 1158 normal subjects. However, there were no significant differences in the genotype of rs28493229 between the controls and children with KD. The results from a study by Lin et al63 in another independent medical center in Taipei indicated that the C allele of rs28493229 is associated with KD susceptibility. Recently, new results using meta-analysis showed that the rs28493229 SNP of ITPKC is associated with the susceptibility to KD in the Taiwanese population39. Regarding to the controversial results obtained for ITPKC genetic association studies in the Taiwanese population, we attribute them to population migration, due to the increase in genetic diversity between cities in the south or north of Taiwan39.
ITPKC is involved in the Ca2+-dependent NFAT signaling pathways in T cells21. In the non-excitable cells, such as T cells and mast cells, one of the main pathways to increase the intracellular Ca2+ concentration is through store-operated calcium channels (SOC)64. The activation of store-operated calcium channels can be controlled by the expression level of IP3. IP3 binds to its receptor (IP3R) on the endoplasmic reticulum (also called the calcium store) causing the release of calcium from stores64. An empty store results in the activation of both store-operated calcium channels and Ca2+-dependent signaling pathways, including inflammatory reactions65, 66 and apoptosis64. Onouchi et al reported that a G to A substitution in the 5′-untranslated region of CASP3 (rs72689236) is associated with susceptibility to Kawasaki disease in Japanese and in Americans of European descent34. The CASP3 (rs72689236) is replicated in the KD patients in the Taiwanese population. Kuo et al provided further evidence that the A allele of rs72689236 is very likely to be a risk allele in the development of aneurysms in patients with KD20.
Another important molecule in the ITPKC signaling pathway is ORAI1 (also known as CRACM1). ORAI1 was identified by Feske et al in 200667. Modified linkage analysis completed on data generated by single-nucleotide polymorphism arrays and an RNA interference screen led to an important finding. A single missense mutation in ORAI1 was found in patients with severe combined immune deficiency (SCID) syndrome67. Furthermore, this mutation in ORAI1 has been shown to cause dysfunctions in Ca2+ release-activated Ca2+ (CRAC) channels and impairs the immune system67. In 2011, a genetic polymorphism of ORAI1 was reported to be associated with the risk and recurrence of calcium nephrolithiasis68. In the study of Kawasaki disease, no significant association between genotype and allele frequency of the five ORAI1 tSNPs was found. Additionally, there is no association between ORAI1 polymorphisms and CAL formation or IVIG treatment responses69. However, this lack of association does not rule out the possibility that other genes in the ITPKC signaling pathways might contribute to the susceptibility or clinical status (CAL or IVIG treatment responses) of KD (Figure 1). For example, a mutation in STIM1, a key molecule in the regulation of SOC, has also been reported to be associated with an immunodeficiency syndrome70. Therefore, identification of genetic polymorphisms for STIM1 and other genes related to the ITPKC pathway by direct DNA sequencing in a larger population may be helpful to better understand the pathogenesis of KD.
Genome-wide association study (GWAS) in Kawasaki disease
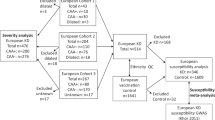
In 2009, Burgner et al firstly performed a genome-wide association study (GWAS) on 119 Caucasian KD cases and 135 matched controls. Forty SNPs and six haplotypes were confirmed in an independent cohort of KD families71. This insightful work led to the identification of a SNP within the N-acetylated alpha-linked acidic dipeptidase-like 2 gene (NAALADL2; rs17531088), which was significantly associated with the susceptibility to KD. Although the function of NAALADL2 remains unclear, mutations in the gene may be involved in the development of Cornelia de Lange syndrome72. In 2010, another GWAS was conducted by Kim et al in a Korean population. A total of 786 subjects (186 KD patients and 600 controls) were recruited. A locus in the 1p31 region was identified as a susceptibility locus for KD. Furthermore, the PELI1 gene locus in the 2p13.3 region was confirmed to associate with the development of CAL in KD patients73. GWAS results from a Taiwanese population suggest another three novel susceptibility loci for KD74. However, the susceptibility loci reported by Kim et al in the Korean population cannot be replicated in a Taiwanese or Caucasian population. Hence, the results of the GWAS from independent groups support the hypothesis that susceptibility loci for KD and CAL formation can be distinct between different ethnic populations.
Conclusion
Several major advances have been made in understanding the genetic effects of the susceptibility and clinical status of KD over the past decade. Very recently, genome-wide association has led two groups to identify novel susceptibility loci as being important for KD in the Asian population. Although the exact genes in the loci are still unclear at present, these loci could provide a new direction for future studies. Now that the sequencing of the human genome is complete and advanced genotyping tools are readily available to help identify candidate genes, we can expect to see more insightful researches begin to elucidate the genes responsible for KD susceptibility.
References
Kawasaki T . Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi 1967; 16: 178–222.
Kawasaki T, Kosaki F, Okawa S, Shigematsu I, Yanagawa H . A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics 1974; 54: 271–6.
Wang CL, Wu YT, Liu CA, Kuo HC, Yang KD . Kawasaki disease: infection, immunity and genetics. Pediatr Infect Dis J 2005; 24: 998–1004.
Burns JC, Glode MP . Kawasaki syndrome. Lancet 2004; 364: 533–44.
Kuo HC, Liang CD, Wang CL, Yu HR, Hwang KP, Yang KD . Serum albumin level predicts initial intravenous immunoglobulin treatment failure in Kawasaki disease. Acta Paediatr 2010; 99: 1578–83.
Park YW, Han JW, Park IS, Kim CH, Cha SH, Ma JS, et al. Kawasaki disease in Korea, 2003–2005. Pediatr Infect Dis J 2007; 26: 821–3.
Huang WC, Huang LM, Chang IS, Chang LY, Chiang BL, Chen PJ, et al. Epidemiologic features of Kawasaki disease in Taiwan, 2003–2006. Pediatrics 2009; 123: e401–5.
Nakamura Y, Yashiro M, Uehara R, Oki I, Kayaba K, Yanagawa H . Increasing incidence of Kawasaki disease in Japan: nationwide survey. Pediatr Int 2008; 50: 287–90.
Liang CD, Kuo HC, Yang KD, Wang CL, Ko SF . Coronary artery fistula associated with Kawasaki disease. Am Heart J 2009; 157: 584–8.
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2004; 110: 2747–71.
Liu YC, Hou CP, Kuo CM, Liang CD, Kuo HC . Atypical kawasaki disease: literature review and clinical nursing. Hu Li Za Zhi 2010; 57: 104–10.
Shimizu C, Jain S, Davila S, Hibberd ML, Lin KO, Molkara D, et al. Transforming growth factor-beta signaling pathway in patients with Kawasaki disease. Circ Cardiovasc Genet 2011; 4: 16–25.
Kuo HC, Wang CL, Liang CD, Yu HR, Chen HH, Wang L, et al. Persistent monocytosis after intravenous immunoglobulin therapy correlated with the development of coronary artery lesions in patients with Kawasaki disease. J Microbiol Immunol Infect 2007; 40: 395–400.
Kuo HC, Wang CL, Liang CD, Yu HR, Huang CF, Wang L, et al. Association of lower eosinophil-related T helper 2 (Th2) cytokines with coronary artery lesions in Kawasaki disease. Pediatr Allergy Immunol 2009; 20: 266–72.
Kuo HC, Wang CL, Wang L, Yu HR, Yang KD . Patient characteristics and intravenous immunoglobulin product may affect eosinophils in Kawasaki disease. Pediatr Allergy Immunol 2008; 19: 184–5.
Kuo HC, Yang KD, Liang CD, Bong CN, Yu HR, Wang L, et al. The relationship of eosinophilia to intravenous immunoglobulin treatment failure in Kawasaki disease. Pediatr Allergy Immunol 2007; 18: 354–9.
Yu HR, Kuo HC, Sheen JM, Wang L, Lin IC, Wang CL, et al. A unique plasma proteomic profiling with imbalanced fibrinogen cascade in patients with Kawasaki disease. Pediatr Allergy Immunol 2009; 20: 699–707.
Kuo HC, Liang CD, Yu HR, Wang CL, Lin IC, Liu CA, et al. CTLA-4, position 49 A/G polymorphism associated with coronary artery lesions in Kawasaki disease. J Clin Immunol 2011; 31: 240–4.
Yu HR, Kuo HC, Huang EY, Liang CD, Hwang KP, Lin IC, et al. Plasma clusterin levels in predicting the occurrence of coronary artery lesions in patients with Kawasaki disease. Pediatr Cardiol 2010; 31: 1151–6.
Kuo HC, Yu HR, Juo SH, Yang KD, Wang YS, Liang CD, et al. CASP3 gene single-nucleotide polymorphism (rs72689236) and Kawasaki disease in Taiwanese children. J Hum Genet 2011; 56: 161–5.
Onouchi Y, Gunji T, Burns JC, Shimizu C, Newburger JW, Yashiro M, et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat Genet 2008; 40: 35–42.
Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med 1991; 324: 1633–9.
Wang CL, Wu YT, Liu CA, Lin MW, Lee CJ, Huang LT, et al. Expression of CD40 ligand on CD4+ T-cells and platelets correlated to the coronary artery lesion and disease progress in Kawasaki disease. Pediatrics 2003; 111: E140–7.
Wang CL, Wu YT, Lee CJ, Liu HC, Huang LT, Yang KD . Decreased nitric oxide production after intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr 2002; 141: 560–5.
Nakamura Y, Yashiro M, Uehara R, Oki I, Watanabe M, Yanagawa H . Epidemiologic features of Kawasaki disease in Japan: results from the nationwide survey in 2005–2006. J Epidemiol 2008; 18: 167–72.
Burns JC, Shimizu C, Shike H, Newburger JW, Sundel RP, Baker AL, et al. Family-based association analysis implicates IL-4 in susceptibility to Kawasaki disease. Genes Immun 2005; 6: 438–44.
Yanagawa H, Nakamura Y, Yashiro M, Oki I, Hirata S, Zhang T, et al. Incidence survey of Kawasaki disease in 1997 and 1998 in Japan. Pediatrics 2001; 107: E33.
Dergun M, Kao A, Hauger SB, Newburger JW, Burns JC . Familial occurrence of Kawasaki syndrome in North America. Arch Pediatr Adolesc Med 2005; 159: 876–81.
Jibiki T, Terai M, Shima M, Ogawa A, Hamada H, Kanazawa M, et al. Monocyte chemoattractant protein 1 gene regulatory region polymorphism and serum levels of monocyte chemoattractant protein 1 in Japanese patients with Kawasaki disease. Arthritis Rheum 2001; 44: 2211–2.
Weng KP, Hsieh KS, Hwang YT, Huang SH, Lai TJ, Yuh YS, et al. IL-10 polymorphisms are associated with coronary artery lesions in acute stage of Kawasaki disease. Circ J 2010; 74: 983–9.
Hsieh KS, Lai TJ, Hwang YT, Lin MW, Weng KP, Chiu YT, et al. IL-10 promoter genetic polymorphisms and risk of Kawasaki disease in Taiwan. Dis Markers 2011; 30: 51–9.
Hsueh KC, Lin YJ, Chang JS, Wan L, Tsai YH, Tsai CH, et al. Association of interleukin-10 A-592C polymorphism in Taiwanese children with Kawasaki disease. J Korean Med Sci 2009; 24: 438–42.
Onouchi Y, Onoue S, Tamari M, Wakui K, Fukushima Y, Yashiro M, et al. CD40 ligand gene and Kawasaki disease. Eur J Hum Genet 2004; 12: 1062–8.
Onouchi Y, Ozaki K, Buns JC, Shimizu C, Hamada H, Honda T, et al. Common variants in CASP3 confer susceptibility to Kawasaki disease. Hum Mol Genet 2010; 19: 2898–906.
Chen SY, Wan L, Huang YC, Sheu JJ, Lan YC, Lai CH, et al. Interleukin-18 gene 105A/C genetic polymorphism is associated with the susceptibility of Kawasaki disease. J Clin Lab Anal 2009; 23: 71–6.
Weng KP, Hsieh KS, Ho TY, Huang SH, Lai CR, Chiu YT, et al. IL-1B polymorphism in association with initial intravenous immunoglobulin treatment failure in Taiwanese children with Kawasaki disease. Circ J 2010; 74: 544–51.
Lin YJ, Wan L, Wu JY, Sheu JJ, Lin CW, Lan YC, et al. HLA-E gene polymorphism associated with susceptibility to Kawasaki disease and formation of coronary artery aneurysms. Arthritis Rheum 2009; 60: 604–10.
Jhang WK, Kang MJ, Jin HS, Yu J, Kim BJ, Kim BS, et al. The CCR5 (-2135C/T) polymorphism may be associated with the development of Kawasaki disease in Korean children. J Clin Immunol 2009; 29: 22–8.
Kuo HC, Yang KD, Juo SH, Liang CD, Chen WC, Wang YS, et al. ITPKC single nucleotide polymorphism associated with the Kawasaki disease in a Taiwanese population. PLoS One 2011; 6: e17370.
Kuo HC, Wu CC, Yang TH, Yu HR, Liang CD, Chen YJ, et al. Non-Langerhans cell histiocytosis in a child with Kawasaki disease. BMJ Case Reports 2009; doi:10.1136/bcr.11.2008.1227.
Akagi T, Rose V, Benson LN, Newman A, Freedom RM . Outcome of coronary artery aneurysms after Kawasaki disease. J Pediatr 1992; 121: 689–94.
Shulman ST, De Inocencio J, Hirsch R . Kawasaki disease. Pediatr Clin North Am 1995; 42: 1205–22.
Wu MT, Hsieh KS, Lin CC, Yang CF, Pan HB . Images in cardiovascular medicine. Evaluation of coronary artery aneurysms in Kawasaki disease by multislice computed tomographic coronary angiography. Circulation 2004; 110: e339.
Newburger JW, Sleeper LA, McCrindle BW, Minich LL, Gersony W, Vetter VL, et al. Randomized trial of pulsed corticosteroid therapy for primary treatment of Kawasaki disease. N Engl J Med 2007; 356: 663–75.
Fukazawa R, Sonobe T, Hamamoto K, Hamaoka K, Sakata K, Asano T, et al. Possible synergic effect of angiotensin-I converting enzyme gene insertion/deletion polymorphism and angiotensin-II type-1 receptor 1166A/C gene polymorphism on ischemic heart disease in patients with Kawasaki disease. Pediatr Res 2004; 56: 597–601.
Kariyazono H, Ohno T, Khajoee V, Ihara K, Kusuhara K, Kinukawa N, et al. Association of vascular endothelial growth factor (VEGF) and VEGF receptor gene polymorphisms with coronary artery lesions of Kawasaki disease. Pediatr Res 2004; 56: 953–9.
Nishimura S, Zaitsu M, Hara M, Yokota G, Watanabe M, Ueda Y, et al. A polymorphism in the promoter of the CD14 gene (CD14/-159) is associated with the development of coronary artery lesions in patients with Kawasaki disease. J Pediatr 2003; 143: 357–62.
Hsueh KC, Lin YJ, Chang JS, Wan L, Tsai YH, Tsai CH, et al. Association of vascular endothelial growth factor C-634 G polymorphism in taiwanese children with Kawasaki disease. Pediatr Cardiol 2008; 29: 292–6.
Quasney MW, Bronstein DE, Cantor RM, Zhang Q, Stroupe C, Shike H, et al. Increased frequency of alleles associated with elevated tumor necrosis factor-alpha levels in children with Kawasaki disease. Pediatr Res 2001; 49: 686–90.
Cheung YF, Ho MH, Ip WK, Fok SF, Yung TC, Lau YL . Modulating effects of mannose binding lectin genotype on arterial stiffness in children after Kawasaki disease. Pediatr Res 2004; 56: 591–6.
Hsueh KC, Lin YJ, Chang JS, Wan L, Tsai YH, Tsai CH, et al. Influence of interleukin 18 promoter polymorphisms in susceptibility to Kawasaki disease in Taiwan. J Rheumatol 2008; 35: 1408–13.
Park JA, Shin KS, Kim YW . Polymorphism of matrix metalloproteinase-3 promoter gene as a risk factor for coronary artery lesions in Kawasaki disease. J Korean Med Sci 2005; 20: 607–11.
Ikeda K, Ihara K, Yamaguchi K, Muneuchi J, Ohno T, Mizuno Y, et al. Genetic analysis of MMP gene polymorphisms in patients with Kawasaki disease. Pediatr Res 2008; 63: 182–5.
Wu SF, Chang JS, Peng CT, Shi YR, Tsai FJ . Polymorphism of angiotensin-1 converting enzyme gene and Kawasaki disease. Pediatr Cardiol 2004; 25: 529–33.
Shim YH, Kim HS, Sohn S, Hong YM . Insertion/deletion polymorphism of angiotensin converting enzyme gene in Kawasaki disease. J Korean Med Sci 2006; 21: 208–11.
Furuno K, Takada H, Yamamoto K, Ikeda K, Ohno T, Khajoee V, et al. Tissue inhibitor of metalloproteinase 2 and coronary artery lesions in Kawasaki disease. J Pediatr 2007; 151: 155–60.
Simonini G, Corinaldesi E, Massai C, Falcini F, Fanti F, De Martino M, et al. Macrophage migration inhibitory factor -173 polymorphism and risk of coronary alterations in children with Kawasaki disease. Clin Exp Rheumatol 2009; 27: 1026–30.
Jin HS, Kim HB, Kim BS, Lee JK, Seo EJ, Yoo HW, et al. The IL-10 (-627 A/C) promoter polymorphism may be associated with coronary aneurysms and low serum albumin in Korean children with Kawasaki disease. Pediatr Res 2007; 61: 584–7.
Cheung YF, Huang GY, Chen SB, Liu XQ, Xi L, Liang XC, et al. Inflammatory gene polymorphisms and susceptibility to Kawasaki disease and its arterial sequelae. Pediatrics 2008; 122: e608–14.
Ban JY, Yoon KL, Kim SK, Kang S, Chung JH . Promoter polymorphism (rs3755724, -55C/T) of tissue inhibitor of metalloproteinase 4 (TIMP4) as a risk factor for Kawasaki disease with coronary artery lesions in a Korean population. Pediatr Cardiol 2009; 30: 331–5.
Hata A, Onouchi Y . Susceptibility genes for Kawasaki disease: toward implementation of personalized medicine. J Hum Genet 2009; 54: 67–73.
Chi H, Huang FY, Chen MR, Chiu NC, Lee HC, Lin SP, et al. ITPKC gene SNP rs28493229 and Kawasaki disease in Taiwanese children. Hum Mol Genet 2010; 19: 1147–51.
Lin MT, Wang JK, Yeh JI, Sun LC, Chen PL, Wu JF, et al. Clinical implication of the C allele of the ITPKC gene SNP rs28493229 in Kawasaki disease: association with disease susceptibility and BCG scar reactivation. Pediatr Infect Dis J 2011; 30: 148–52.
Parekh AB, Putney JW Jr . Store-operated calcium channels. Physiol Rev 2005; 85: 757–810.
Chang WC, Nelson C, Parekh AB . Ca2+ influx through CRAC channels activates cytosolic phospholipase A2, leukotriene C4 secretion, and expression of c-fos through ERK-dependent and -independent pathways in mast cells. FASEB J 2006; 20: 2381–3.
Chang WC, Parekh AB . Close functional coupling between Ca2+ release-activated Ca2+ channels, arachidonic acid release, and leukotriene C4 secretion. J Biol Chem 2004; 279: 29994–9.
Feske S, Gwack Y, Prakriya M, Srikanth S, Puppel SH, Tanasa B, et al. A mutation in Orai1 causes immune deficiency by abrogating CRAC channel function. Nature 2006; 441: 179–85.
Chou YH, Juo SH, Chiu YC, Liu ME, Chen WC, Chang CC, et al. A polymorphism of the ORAI1 gene is associated with the risk and recurrence of calcium nephrolithiasis. J Urol 2011; 185: 1742–6.
Kuo HC, Lin YJ, Juo SH, Hsu YW, Chen WC, Yang KD, et al. Lack of association between ORAI1/CRACM1 gene polymorphisms and Kawasaki disease in the Taiwanese children. J Clin Immunol 2011. 10.1007/s10875-011-9524–8.
Picard C, McCarl CA, Papolos A, Khalil S, Luthy K, Hivroz C, et al. STIM1 mutation associated with a syndrome of immunodeficiency and autoimmunity. N Engl J Med 2009; 360: 1971–80.
Burgner D, Davila S, Breunis WB, Ng SB, Li Y, Bonnard C, et al. A genome-wide association study identifies novel and functionally related susceptibility Loci for Kawasaki disease. PLoS Genet 2009; 5: e1000319.
Tonkin ET, Smith M, Eichhorn P, Jones S, Imamwerdi B, Lindsay S, et al. A giant novel gene undergoing extensive alternative splicing is severed by a Cornelia de Lange-associated translocation breakpoint at 3q26.3. Hum Genet 2004; 115: 139–48.
Kim JJ, Hong YM, Sohn S, Jang GY, Ha KS, Yun SW, et al. A genome-wide association analysis reveals 1p31 and 2p13.3 as susceptibility loci for Kawasaki disease. Hum Genet 2011; 129: 487–95.
Tsai FJ, Lee YC, Chang JS, Huang LM, Huang FY, Chiu NC, et al. Identification of novel susceptibility Loci for Kawasaki disease in a Han Chinese population by a genome-wide association study. PLoS One 2011; 6: e16853.
Taniuchi S, Masuda M, Teraguchi M, Ikemoto Y, Komiyama Y, Takahashi H, et al. Polymorphism of Fc gamma RIIa may affect the efficacy of gamma-globulin therapy in Kawasaki disease. J Clin Immunol 2005; 25: 309–13.
Biezeveld M, Geissler J, Merkus M, Kuipers IM, Ottenkamp J, Kuijpers T . The involvement of Fc gamma receptor gene polymorphisms in Kawasaki disease. Clin Exp Immunol 2007; 147: 106–11.
Huang FY, Chang TY, Chen MR, Chiu NC, Chi H, Lee HC, et al. Genetic polymorphisms in the CD40 ligand gene and Kawasaki disease. J Clin Immunol 2008; 28: 405–10.
Acknowledgements
This study was partly supported by funding from an Excellence for Cancer Research Center grant, Department of Health, Executive Yuan, Taiwan, China (No DOH100-TD-C-111-002), and a grant (NSC 100-2320-B-037-002) from the National Science Council, Taiwan, China, to Wei–chiao CHANG. A grant (NSC 98-2314-B-182A-004-MY3) from the National Science Council of Taiwan and a grant (NSC 100-2314-B-182A-048 -MY3) from Chang Gung Memorial Hospital, Taiwan, China (CMRPG891441 and CMRPG891241) also helped to support this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuo, Hc., Chang, Wc. Genetic polymorphisms in Kawasaki disease. Acta Pharmacol Sin 32, 1193–1198 (2011). https://doi.org/10.1038/aps.2011.93
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.93
Keywords
This article is cited by
-
Whole-exome sequencing analysis identifies novel variants associated with Kawasaki disease susceptibility
Pediatric Rheumatology (2023)
-
Inositol-Triphosphate 3-Kinase C and DNA Methylation Involvement in NLRP3 Inflammasome Activation in Kawasaki Disease
Indian Journal of Pediatrics (2023)
-
Kawasaki disease in siblings in close temporal proximity to each other—what are the implications?
Clinical Rheumatology (2021)
-
Discovery and structural optimization of 1-phenyl-3-(1-phenylethyl)urea derivatives as novel inhibitors of CRAC channel
Acta Pharmacologica Sinica (2015)
-
Common carotid artery intima-media thickness is useful for diagnosis of the acute stage of Kawasaki disease
BMC Pediatrics (2014)