Abstract
Multiple myeloma (MM) is a heterogeneous plasma cell disorder characterized by genetic abnormalities, including chromosomal translocations, deletions, duplications and genetic mutations. Translocations involving the immunoglobulin heavy chain region at chromosome 14q32 are observed in approximately 40% of patients with MM. Translocation of oncogenes into this region may lead to their increased expression, contributing to disease initiation, disease progression and therapeutic resistance. The t(4;14) translocation is associated with upregulation of the fibroblast growth factor receptor 3 (FGFR3) and the myeloma SET domain protein. Patients with t(4;14) demonstrate an overall poor prognosis that is only partially mitigated by the use of the novel agents bortezomib and lenalidomide; as such, an unmet medical need remains for patients with this aberration. Preclinical studies of inhibitors of FGFR3 have shown promise in t(4;14) MM, and these studies have led to the initiation of clinical trials. Data from these trials will help to determine the clinical utility of FGFR3 inhibitors for patients with t(4;14) MM and may pave the way for personalized medicine in patients with this incurable disease.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is an incurable hematological disorder in which malignant plasma cells accumulate in the bone marrow and is primarily distinguished from other premalignant plasma cell disorders, such as monoclonal gammopathy of unknown significance or smoldering MM, by the presence of end-organ damage as defined by the CRAB criteria: hypercalcemia, renal impairment, anemia and bone disease.1 Although MM is characterized by a range of genetic aberrations leading to heterogeneity in the patient population, the specific mechanisms leading to the development of plasma cell disorders and progression to symptomatic MM have not been fully elucidated. Treatment options for patients with MM have improved significantly within the past decade, resulting in improved response rates and survival;2 however, a disparity remains for patients with poor prognostic factors, including t(4;14). As has been shown for other hematological malignancies,3 it is hoped that patients with MM may similarly benefit from personalized treatment strategies that target molecular mechanisms contributing to their underlying disease.
Molecular genetics of MM
MM is characterized by significant molecular heterogeneity and comprises two broad subtypes of disease that may reflect different underlying oncogenetic pathways of evolution—one characterized by chromosomal gains (hyperdiploidy) and the other by structural changes (nonhyperdiploidy), most commonly involving translocations of the IGH gene, located at 14q32.4, 5, 6 These translocations lead to the juxtaposition with and subsequent dysregulation of putative oncogenes by immunoglobulin heavy chain (IgH) control elements and have been demonstrated to affect approximately 40% of patients with MM.7 The former and more frequently recognized abnormalities are defined by recurrent chromosome gains that usually do not have coexistent 14q32 translocations.8, 9, 10
These initial genetic insults are invariably followed by further karyotypic instability that may result in further deletions and secondary translocations and/or mutations.10 Characterization of various genetic abnormalities among patients with MM and their impact on prognosis has led to a disease-risk classification system and suggested treatment recommendations.7
IgH translocations in MM
The IgH locus at 14q32 is transcriptionally active in B cells, and the translocation of putative oncogenes to this region and their subsequent dysregulated expression is considered a seminal event in the pathogenesis of most B-cell malignancies, including MM.11 Chromosomal translocations at 14q32 have been implicated as early genetic lesions in the pathogenesis of some cases of MM because of their presence in 35–50% of patients with monoclonal gammopathy of unknown significance and smoldering MM,10 although some variants may represent progression/secondary translocations. There are several known translocations of 14q32 with nonrandom partners, including the more commonly observed t(4;14) and t(11;14) translocations (30% of patients with MM) and the less common (⩽5% of patients) t(14;16), t(6;14), t(8;14) and t(14;20) translocations (Table 1).11, 12, 13, 14, 15, 16, 17 These translocations are associated with upregulation of oncogenes—including D-type cyclins (cyclin D1, D2 and D3), MAF family members (MafA, MafB and c-Maf), c-MYC, the myeloma SET domain protein (MMSET) and the fibroblast growth factor receptor 3 (FGFR3)—and have been shown to influence patient prognosis (Table 1).7, 18 Dysregulation of these genes and others not specifically related to 14q32 translocations results in specific gene-expression signatures that correlate with disease biology and prognosis.5, 19
Other genetic abnormalities in MM
In addition to 14q32 translocations, hyperdiploidy is a common genetic abnormality in patients with MM and is typically characterized by trisomy of odd-numbered chromosomes (3, 5, 7, 9, 11, 15 and 19),20 although the molecular basis for this is currently unknown. As a group, patients with hyperdiploidy have been recognized as having a better prognosis than the nonhyperdiploid group.4, 20
Both hyperdiploid and IgH translocation genetic events are unified by the downstream upregulation of cyclins D1, D2 and/or D3, which is then followed by further karyotypic instability. Secondary chromosomal abnormalities, including deletions, amplifications and additional translocations, may also adversely affect outcomes.7 Deletions of chromosome 17p13 (the chromosomal change associated with the poorest prognosis21) and 13q14 have been observed in up to 10% and 50%, respectively, of patients with MM, and both are associated with a poor prognosis.7, 22 Another important secondary event correlating with disease progression is amplification of the long arm of chromosome 1 (1q21). The amplification of 1q21 is absent in patients with monoclonal gammopathy of unknown significance but is observed in 43% of patients with newly diagnosed MM and 72% of patients with relapsed MM23 and is associated with a poor prognosis, particularly in the context of other high-risk abnormalities, such as t(4;14) translocation.23 Somatic activating mutations of several oncogenes have also been observed in MM, including FGFR3, NRAS and KRAS, and have been correlated with clinical outcome.10
Despite the breadth of knowledge on the role of these chromosomal aberrations in the prognosis of patients with MM, there are currently no therapies that specifically target genes or the pathways influenced by these genetic abnormalities. Data from studies evaluating bortezomib and lenalidomide have demonstrated that regimens with these novel agents are probably more effective than more conventional therapeutic approaches in patients with high-risk cytogenetic factors, but patients treated with these agents develop resistance, and alternative, more effective treatment strategies are urgently needed.24, 25 The t(4;14) translocation is one of the most prevalent IgH translocations in MM, may be associated with ectopic expression of FGFR318 and is associated with a poor prognosis.10 This review will focus on the role of the t(4;14) translocation, the influence of this translocation on FGFR3 expression and treatment strategies for patients whose tumors harbor this chromosomal aberration.
The t(4;14) translocation and FGFR in MM
Molecular characterization of the t(4;14) translocation
At the time of the discovery of the t(4;14)(p16.3;q32.2) translocation, the role of translocations involving the IgH locus at chromosome 14q32 in B-cell malignancies was well characterized. The karyotypically silent t(4;14) translocation, undetectable by conventional cytogenetic analysis, was identified independently by two groups utilizing southern blot analysis of cell line and patient samples.18, 26 The break points on chromosome 4 occurred in a region mapping to the FGFR3 gene, which is 50–100 kb telomeric to the 4p16 break points, and dysregulation of this gene was noted in several of the samples analyzed.18, 26
Subsequent to the initial observations, Chesi et al.27 reported that another gene, MMSET, was also affected by the t(4;14) translocation; the 4p16 break point occurs telomeric to and within the 5′ introns of MMSET, resulting in IgH/MMSET hybrid transcripts and MMSET overexpression from endogenous promoters on 4p16 (Figure 1). From these studies, it was hypothesized that dysregulation of both FGFR3 and MMSET contributes to neoplastic transformation in MM with t(4;14). The t(4:14) translocation was the first example of an IgH translocation that simultaneously dysregulated two genes with oncogenic potential: FGFR3 on der(14) and MMSET on der(4).27
The t(4;14) translocation is observed in approximately 15–20% of patients with MM14, 27 and is detected by interphase fluorescence in situ hybridization or reverse transcriptase PCR.10 A majority of patients whose tumors harbor the t(4;14) translocation also demonstrate deletion of chromosome 13q.12, 28 Because of this strong association, it has been hypothesized that deletion of chromosome 13q precedes the t(4;14) translocation in the pathogenesis of MM.28 Indeed, these genetic aberrations have been detected in patients with monoclonal gammopathy of unknown significance and smoldering MM, as well as symptomatic MM, and it has recently been demonstrated that the percentage of plasma cells that harbor the t(4;14) translocation or 13q deletion significantly increases with progression of disease, thus suggesting that the clonal expansion of cells harboring such aberrations may drive disease progression.29
The roles of FGFR3 and MMSET proteins in the pathogenesis of MM remain elusive. Overexpression of FGFR3 protein occurs in only approximately 70% of patients with the t(4;14) translocation; however, MMSET is overexpressed in all cases.30, 31 The MMSET gene product is a histone methyltransferase; its function in both normal cells and MM tumors has only recently been investigated. Martinez-Garcia et al.32 reported that in an MM cell-line system with the t(4:14) translocation, MMSET expression resulted in methylation of histone 3 at lysine 36 along with changes in chromatin structure. Pei et al.33 identified MMSET as a histone methyltransferase with activity toward H4K420 when transfected into human embryonic kidney cells. In this model, MMSET regulated the recruitment of p53-binding protein (53BP1) to sites of DNA damage. Together, these studies suggest a role for MMSET in regulating DNA repair and overall gene expression, which may be dysregulated in t(4;14) MM cells. Furthermore, MMSET immunoreactivity has been detected in samples from a variety of tumor types, suggesting it may be more broadly involved in oncogenesis.34
Overexpression of both FGFR3 and MMSET has been implicated in the specific changes in gene expression observed in plasma cells as a result of the t(4;14) translocation. Although microarray analysis of patient samples with the t(4;14) translocation not unexpectedly identified FGFR3 and MMSET as the top two overexpressed genes, the translocation also resulted in a specific genetic signature characterized by perturbations in the expression of several other genes.19 Overexpressed genes included the Wnt receptors FZD2 and FZD8 and the oncogene PBX1.19 Although the cadherin family member desmoglein 2 was also overexpressed, N-cadherin and cadherin 7 were underexpressed as was the adhesion molecule ICAM4.19 Of note, the t(4;14) translocation was associated with overexpression of MMSET in all patient samples analyzed, whereas overexpression of FGFR3 was observed in only 75% of cases.19, 30 A small proportion of patients with the t(4;14) translocation also have FGFR3-activating mutations, including A1157G, A1987G, A761G and G1138A; however, overall these mutations are rare, with a frequency of approximately 5% among t(4;14) patients.35, 36, 37
There may be additional mechanisms by which FGFR3 is dysregulated in MM that are independent of t(4;14) translocation. Although rare, amplification of the FGFR3 gene has been observed in MM cell lines and patients.38, 39 Based on these data, FGFR3 may have a broader role in MM disease biology beyond its juxtaposition and subsequent overexpression following translocation to the IgH region. Furthermore, gene-expression analysis of FGFR3 in addition to fluorescence in situ hybridization analysis for t(4;14) will be necessary to account for patients who may express FGFR3 independent of translocation or, conversely, who lack overexpression of FGFR3 in the presence of t(4;14).
Biology of FGFR3
FGFR3 is one of four members of the FGFR family of transmembrane tyrosine kinase receptors that are involved in the intracellular signaling pathways. FGFR activation has been shown to have a critical role in both embryogenesis and adults with a pleiotropic range of sequelae, including cell proliferation and survival, migration, differentiation and growth arrest.40 Signaling is mediated by 1 of the 18 FGF ligands, and ligand-receptor specificity is controlled by differential cellular expression of the receptors, secretion of cell-surface proteins that modulate the interaction and alternative splicing of the receptors.40, 41 FGF ligands cause dimerization of FGFRs, which leads to activation and phosphorylation of the intracellular tyrosine kinase domain. That, in turn, leads to activation of the several key pathways implicated in oncogenic signaling, including the mitogen-activated protein kinase (RAS-RAF-MAPK), phosphatidylinositol 3-kinase (PI3K-AKT-mTOR), phospholipase Cγ (PLCγ), protein kinase C (PKC) and signal transducer and activator of transcription (STAT) pathways (Figure 2).40 Because of the role that FGFR3 has in these critical pathways, it is clear how genetic alterations of the receptor may have oncogenic potential. Genetic alterations of the FGFR family are observed in several cancers besides MM; these include FGFR1 amplification in breast cancer (10%), FGFR2 mutation in endometrial cancer (12%) and FGFR3 mutation in bladder cancer (50–60% invasive and 10–15% noninvasive).42, 43, 44, 45
The FGFR and downstream pathways. Signaling pathways activated by FGF ligand binding to FGFR include the mitogen-activated protein kinase (RAS-RAF-MAPK), phosphatidylinositol 3-kinase (PI3K-AKT-mTOR), phospholipase Cγ (PLCγ), protein kinase C (PKC), and signal transducer and activator of transcription (STAT) pathways. DAG, diacylglycerol; FGF, fibroblast growth factor; FGFR, fibroblast growth factor receptor; JAK, Janus kinase.
The intergenic t(4;14) translocation places the FGFR3 gene under the control of the active IGH promoter and may result in an increase in ligand-dependent and ligand-independent signaling.37, 46 This aberrant signaling can lead to activation of the downstream pathways that drive disease progression. It was demonstrated that overexpression of FGFR3 in the bone marrow of mice led to the development of tumors, and antibody-based targeting of FGFR3 in vitro has been demonstrated to be cytotoxic in MM cells with the t(4;14) translocation.47, 48 These data support the contribution of aberrant FGFR3-expression translocation in the disease pathology of t(4;14) MM.
Clinical impact of the t(4;14) translocation in MM
Overall, patients with MM treated with conventional therapies experience a median survival of 3–4 years, and among patients who undergo autologous stem cell transplantation, the median survival is around 5–7 years.49 Higher stage of disease, as determined by the International Staging System (ISS), which uses the β-2 microglobulin and serum albumin, is associated with shorter overall survival (OS).50 Currently, the ISS does not incorporate cytogenetics in staging of disease; however, a large body of evidence has demonstrated that cytogenetics influences outcomes in patients with MM. Several studies have shown the t(4;14) translocation as well as the MAF translocations t(14;16) and t(14;20), usually detected by fluorescence in situ hybridization rather than metaphase cytogenetics, are associated with an overall poor prognosis for patients with MM.10, 13, 19, 28, 51, 52 Deletion of 17p13, which leads to inactivation of p53, is associated with an extremely poor prognosis that has been shown to be independent of the t(4;14) translocation.53 Deletion of chromosome 13 (when detected by fluorescence in situ hybridization as opposed to metaphase cytogenetics) was also thought to be associated with a poor prognosis but is commonly found in patients with t(4;14), t(14;16) and t(14;20);10, 13, 19 as such, it is now considered that its apparent prognostic impact may actually be related to the presence of coexisting genetic changes.22
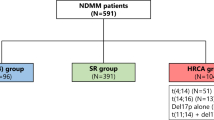
On the basis of the data linking certain genetic abnormalities with outcomes, several groups have now published prognostic stratification guidelines incorporating cytogenetic factors to determine disease risk. Stewart et al.7 describe a consensus definition that classifies high-risk patients (25% of patients with MM) as having any of t(4;14), t(14, 16), t(14;20), deletion of 17q13, deletion of chromosome 13 by metaphase cytogenetics, aneuploidy or a plasma cell labeling index of >3.0. The remaining ‘good-risk’ patients lack these high-risk features but may exhibit hyperdiploidy or translocations, including t(11;14) or t(6;14). Stewart and colleagues suggest that a high-risk diagnostic panel be performed on all patients newly diagnosed with MM to make informed choices regarding therapeutic options, notably to identify the poor-risk group in whom current therapies are inadequate and the use of investigational agents should be considered. The role of cytogenetics has also been analyzed in the context of the ISS. A study by Neben et al.49 demonstrated significant differences in progression-free survival (PFS) and OS among patients classified as low, intermediate or high risk. Patients were classified as low risk if they had they had ISS stage I MM without the presence of deletion of 17p13 or t(4;14). Intermediate-risk patients included ISS stage I patients with deletion of 17p13 or t(4;14) and ISS stage II/III patients without these poor prognostic cytogenetic markers. High-risk patients included ISS stage II/III patients with deletion of 17p13 or t(4;14).49 Both these studies have clear implications for the implementation of risk-adapted treatment strategies. Such risk-adaptive strategies could include novel combinations, including chemotherapeutic agents (melphalan and doxorubicin), novel agents (bortezomib, lenalidomide and thalidomide) or investigational agents such as second-generation proteasome inhibitors and immunomodulatory agents, deacetylase inhibitors or inhibitors of the FGFR3 receptor.
Treatment strategies and outcomes for patients with t(4;14) MM
Patients with t(4;14) MM have a poor prognosis in comparison with the MM population as a whole; however, factors including stage of disease (newly diagnosed and relapsed/refractory) or type of therapy may lead to differences in patient outcomes (Table 2). In a recent study of patients with t(4;14) and ISS stage II/III symptomatic MM, high response rates (93%) were observed following high-dose therapy, but this did not translate into prolonged PFS or OS.54 Patients with t(4;14) MM demonstrate a shorter duration of remission51, 55 and more aggressive relapses characterized by renal failure, cytopenia and extramedullary disease.7, 54 It was concluded that the poor prognosis conferred by the t(4;14) translocation was related to shortened PFS after achieving an initial disease response to high-dose chemotherapy combined with subsequent failure of salvage therapy, suggesting resistance to alkylating agent-based treatment approaches (Table 2).54, 55 Therefore, the treatment of patients with MM bearing the t(4;14) translocation represents a substantial challenge.
Implications for the clinical impact of risk-adapted treatment strategies are not entirely clear. Although the introduction of novel agents has led to improved outcomes in patients with MM, particularly patients with relapsed/refractory disease,2 the beneficial impact on outcomes in patients with t(4;14) MM remains uncertain (Table 2). However, in several studies investigating novel agents, available data suggest that the poor prognosis conferred by t(4;14) (as well as by other poor-risk cytogenetic abnormalities) may be partially overcome by the newer agents, particularly bortezomib.13, 21, 24, 25, 51, 56, 57, 58
Bortezomib in the treatment of t(4;14) MM
In the phase III Velcade as Initial Standard Therapy in Multiple Myeloma: Assessment with Melphalan and Prednisone (VISTA) trial evaluating melphalan and prednisone alone or in combination with bortezomib in patients with newly diagnosed MM, the impact of high-risk cytogenetics, as defined by the presence of a t(4;14) or t(14;16) translocation or a 17p deletion, was analyzed.25 Among patients who received bortezomib-containing therapy, response rate, PFS and OS were similar in high-risk and the standard cytogenetic profile groups.25 Another study, albeit with only 65 patients, showed that when relapsed/refractory MM was treated with single-agent bortezomib, there were no statistical differences in terms of outcome between patients with t(4;14) MM in comparison with the entire population.57 The Total Therapy 3 trial evaluated the addition of bortezomib to the chemotherapy regimen defined in the previous Total Therapy 2 trial, which consisted of thalidomide and dexamethasone along with 4-day continuous infusions of cisplatin, doxorubicin, cyclophosphamide and etoposide in patients with newly diagnosed MM.59 Pineda-Roman et al.58 demonstrated that in a subgroup of high-risk patients defined by gene-expression profiling to have elevated FGFR3 and MMSET levels, patients in the Total Therapy 3 study demonstrated significantly better outcomes for OS, event-free survival and complete response duration compared with patients in the Total Therapy 2 trial (Table 2), suggesting that the incorporation of bortezomib into multiagent approaches for this subset of patients at diagnosis confers a survival advantage.
Consistent with these reports, a recent study by Avet-Loiseau et al.21 of 507 patients with newly diagnosed MM found that bortezomib and dexamethasone improved the outcome of patients with t(4;14) compared with patients treated with vincristine, doxorubicin and dexamethasone; however, the presence of t(4;14) remained an adverse prognostic factor for both event-free survival and OS. Patients with the t(4;14) translocation had a reduced OS and an increased rate of relapse at a median follow-up of 24 months (41% versus 31% without t(4;14) translocation; P=0.0178). The authors hypothesized that the difference in results among the various trials may be related to differences in patient numbers or duration of therapy, that is, perhaps only the long-term administration of bortezomib as a ‘maintenance’ therapy is able to abrogate the poor prognosis of t(4;14).21 Additional prospective studies are needed to more clearly define the role of bortezomib in the treatment of patients with t(4:14) MM.
Lenalidomide in the treatment of t(4;14) MM
Lenalidomide may also improve outcomes in patients with t(4;14) MM; however, the evidence for this is less compelling. A retrospective analysis by Reece et al.24 of patients with relapsed/refractory MM treated with lenalidomide or lenalidomide plus dexamethasone concluded that the time to progression and OS was equivalent between patients with the t(4;14) translocation and the entire population (Table 2). Furthermore, this was supported by a matched-pair analysis to account for imbalances in patient characteristics.24 However, these conclusions are in contrast with a larger, more recent study by Avet-Loiseau et al.56 in which patients also received lenalidomide plus dexamethasone. In this study, both PFS and OS were lower among patients with the t(4;14) translocation when compared with those without the translocation. This study was also limited by the retrospective nature of the analysis, and the authors attributed the differences in the results to variations among the patient populations, again highlighting the need for prospective studies.
Implementing risk-adapted treatment strategies for t(4;14) MM
The treatment of patients with high-risk cytogenetic factors remains an area of unmet medical need. Although the development of novel agents has resulted in improved outcomes in these patients, there is a clear need for further improvement. Risk-adapted treatment strategies would be applicable for patients who present with high-risk factors and are exemplified by the Mayo Stratification for Myeloma and Risk-Adapted Therapy guidelines for the treatment of patients with MM, in which patients with t(4;14) translocations, elevated β-2 microglobulin and anemia are considered to have intermediate- or high-risk disease. A bortezomib-containing regimen is recommended for these patients.60
Future directions in the treatment of MM with t(4;14) translocations
Bortezomib and, to a lesser extent, lenalidomide have demonstrated improved outcomes in patients with high-risk cytogenetic abnormalities, including t(4;14), when compared with conventional therapy, but other novel treatment approaches or modalities may prove to be more effective. Of note, a recent analysis of patients who received allogeneic stem cell transplant with melphalan–fludarabine-based conditioning demonstrated statistically similar rates of event-free survival and OS between patients with t(4;14) translocations and the entire patient population.61 This was in contrast with del(17p), which retained its negative prognostic value. As discussed earlier, bortezomib-based therapies have improved outcomes in patients with this translocation, and bortezomib may overcome resistance mediated by overexpression of FGFR3. A study in patients with relapsed MM who received bortezomib salvage therapy demonstrated equivalent time to progression and OS among patients with FGFR3-positive tumors as confirmed by immunohistochemistry compared with patients with tumors lacking FGFR3 expression.62 Agents that can interfere with or mitigate the effects of FGFR3 signaling are therefore of interest as a novel approach for the treatment of t(4;14) MM.
Small-molecule tyrosine kinase inhibitors of FGFR3
There are several inhibitors of FGFR3 at various stages of clinical development for the treatment of MM. Both small-molecule inhibitors and monoclonal antibody-based approaches induce cell-growth arrest and apoptosis in MM cell lines bearing the t(4;14) translocation.48, 63, 64, 65, 66, 67, 68 Studies with the FGFR-specific tyrosine kinase inhibitor SU5402 showed that it inhibited cell growth and led to apoptosis in MM cells at micromolar concentrations. Of note, although the MM cell line KMS11, which harbors an activating mutation of FGFR3, was exquisitely sensitive to SU5402, the K620 cell line, which does not express FGFR3, demonstrated resistance.63 Furthermore, cell lines with t(4;14) and a concomitant mutation of NRAS, upstream of ERK 1/2, were also resistant to SU5402.63 Similar results were also observed in a study evaluating the highly specific FGFR tyrosine kinase inhibitor PD173074.65 This compound also demonstrated antimyeloma activity against FGFR3-expressing cell lines and prolonged the survival of mice in a KMS11 xenograft model.65 In contrast, the multitargeted tyrosine kinase inhibitor PKC412, which is currently undergoing evaluation for the treatment of FLT3-positive acute myeloid leukemia, demonstrated significant activity against both FGFR3- and RAS-mutated myeloma cells.69
Dovitinib (TKI-258 and CHIR-258) is a potent multitargeted tyrosine kinase inhibitor with nanomolar activity against the vascular endothelial growth factor receptors 1–3, platelet endothelial growth factor receptors α and β and FGFR1 and FGFR3.64, 70 Similar to the results observed with SU5402 and PD173074, dovitinib demonstrated antimyeloma activity in t(4;14) FGFR3-expressing cell lines and in both mouse xenograft and orthotopic models of MM.64, 67 As described for SU5402, cells with NRAS mutations were resistant to TKI-258, thus demonstrating a similar profile for these agents.65 A recent study with another FGFR3 inhibitor, BIBF 1000, demonstrated that dexamethasone could sensitize NRAS-mutant cell lines to FGFR3 inhibition.68 Based on these early studies of dovitinib and early clinical results seen in other tumors, a phase II study of dovitinib in patients with relapsed or refractory MM is ongoing (NCT01058434).71 The results of this trial will help to determine if tyrosine kinase inhibitors that target FGFR3 demonstrate efficacy in patients with MM.
Monoclonal antibody inhibitors of FGFR3
Monoclonal antibody-based approaches have also been investigated. The fully human monoclonal antibody PRO-001 inhibits ligand binding to FGFR3 on t(4;14) MM cells. Preclinical studies have shown that PRO-001 inhibits FGFR3 signaling, leading to inhibition of cell growth and apoptosis in FGFR3 MM cells.66 However, in contrast with the tyrosine kinase inhibitors, the KMS11 MM cell line, which bears the FGFR3 Y377C-activating mutation, was resistant to PRO-011.66 Another FGFR3-specific monoclonal antibody under evaluation, R3Mab, inhibits ligand binding as well as causes changes to receptor confirmation.48 Furthermore, R3Mab was able to inhibit cell growth in an in vivo xenograft model of the FGFR3-mutant cell line KMS11 through antibody-dependent cellular cytotoxicity.48
Conclusions
Treatment options for patients with MM have improved considerably over the past decade, resulting in survival rates that surpass 10 years for some patients. These advances have also led to improved outcomes for those with high-risk cytogenetic abnormalities, such as t(4;14), when compared with conventional therapeutic approaches, although these improvements are less substantial for high-risk than for lower-risk patients. Clinical data suggest that bortezomib and, to a lesser extent, lenalidomide may partially overcome the poor prognosis conferred by the t(4;14) translocation, although there are discrepancies among the various studies, and prospective analyses are clearly needed to determine the true impact of these agents on patients with this abnormality.21, 24, 56, 57
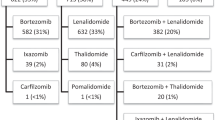
MM is a heterogeneous disease; however, treatment options outside of clinical trials are currently limited to combinations of bortezomib, thalidomide and its analogs (IMiDs, thalidomide and lenalidomide), chemotherapy and steroids (dexamethasone, prednisone) with stem cell transplantation in eligible patients. Although these agents are effective in the treatment of a majority of patients with MM, a clear unmet need remains for high-risk patients. The Mayo Stratification for Myeloma and Risk-Adapted Therapy guidelines have provided an example of a personalized therapeutic approach for the treatment of MM; however, among the different risk groups, there remains a considerable degree of heterogeneity.60 Molecular-based targeted therapeutic approaches, analogous to those used in the treatment of other diseases, such as breast cancer, may help to identify patient subsets that derive benefit from novel investigational agents and lead to the development of personalized therapeutic approaches.
The use of FGFR3 inhibitors for patients with t(4;14) MM represents a potential targeted and personalized approach. Based on the preclinical data, these therapies may benefit a subset of patients with the t(4;14) translocation, particularly those with increased expression of FGFR3 and absence of NRAS mutations.63, 64, 65, 67 Further research is needed to determine the ideal therapeutic combination partners (for example, bortezomib, IMiDs, chemotherapy and steroids), but early evidence suggests that this class of agents synergizes with bortezomib and dexamethasone.68 Based on the available data, FGFR3 inhibitors should be investigated in clinical trials for patients with t(4;14) translocations, both as monotherapy and in combination with standard-of-care agents used in the treatment of MM. Carefully designed clinical trials that incorporate biomarker analyses will be needed to ultimately determine the ideal patient population that will derive benefit from this novel approach.
References
Katzel JA, Hari P, Vesole DH . Multiple myeloma: charging toward a bright future. CA Cancer J Clin 2007; 57: 301–318.
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Deininger MW, Druker BJ . Specific targeted therapy of chronic myelogenous leukemia with imatinib. Pharmacol Rev 2003; 55: 401–423.
Bergsagel PL, Kuehl WM, Zhan F, Sawyer J, Barlogie B, Shaughnessy J . Cyclin D dysregulation: an early and unifying pathogenic event in multiple myeloma. Blood 2005; 106: 296–303.
Decaux O, Lode L, Magrangeas F, Charbonnel C, Gouraud W, Jezequel P et al. Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiploid signatures in low-risk patients: a study of the Intergroupe Francophone du Myelome. J Clin Oncol 2008; 26: 4798–4805.
Fonseca R, Bergsagel PL, Drach J, Shaughnessy J, Gutierrez N, Stewart AK et al. International Myeloma Working Group molecular classification of multiple myeloma: spotlight review. Leukemia 2009; 23: 2210–2221.
Stewart AK, Bergsagel PL, Greipp PR, Dispenzieri A, Gertz MA, Hayman SR et al. A practical guide to defining high-risk myeloma for clinical trials, patient counseling and choice of therapy. Leukemia 2007; 21: 529–534.
Chng WJ, Van Wier SA, Ahmann GJ, Winkler JM, Jalal SM, Bergsagel PL et al. A validated FISH trisomy index demonstrates the hyperdiploid and nonhyperdiploid dichotomy in MGUS. Blood 2005; 106: 2156–2161.
Chng WJ, Winkler JM, Greipp PR, Jalal SM, Bergsagel PL, Chesi M et al. Ploidy status rarely changes in myeloma patients at disease progression. Leuk Res 2006; 30: 266–271.
Fonseca R, Barlogie B, Bataille R, Bastard C, Bergsagel PL, Chesi M et al. Genetics and cytogenetics of multiple myeloma: a workshop report. Cancer Res 2004; 64: 1546–1558.
Nahi H, Sutlu T, Jansson M, Alici E, Gahrton G . Clinical impact of chromosomal aberrations in multiple myeloma. J Intern Med 2011; 269: 137–147.
Avet-Loiseau H, Facon T, Grosbois B, Magrangeas F, Rapp MJ, Harousseau JL et al. Oncogenesis of multiple myeloma: 14q32 and 13q chromosomal abnormalities are not randomly distributed, but correlate with natural history, immunological features, and clinical presentation. Blood 2002; 99: 2185–2191.
Gertz MA, Lacy MQ, Dispenzieri A, Greipp PR, Litzow MR, Henderson KJ et al. Clinical implications of t(11;14)(q13;q32), t(4;14)(p16.3;q32), and -17p13 in myeloma patients treated with high-dose therapy. Blood 2005; 106: 2837–2840.
Moreau P, Facon T, Leleu X, Morineau N, Huyghe P, Harousseau JL et al. Recurrent 14q32 translocations determine the prognosis of multiple myeloma, especially in patients receiving intensive chemotherapy. Blood 2002; 100: 1579–1583.
Shaughnessy J, Gabrea A, Qi Y, Brents L, Zhan F, Tian E et al. Cyclin D3 at 6p21 is dysregulated by recurrent chromosomal translocations to immunoglobulin loci in multiple myeloma. Blood 2001; 98: 217–223.
Boersma-Vreugdenhil GR, Kuipers J, Van Stralen E, Peeters T, Michaux L, Hagemeijer A et al. The recurrent translocation t(14;20)(q32;q12) in multiple myeloma results in aberrant expression of MAFB: a molecular and genetic analysis of the chromosomal breakpoint. Br J Haematol 2004; 126: 355–363.
Avet-Loiseau H, Gerson F, Magrangeas F, Minvielle S, Harousseau J, Bataille R . Rearrangements of the c-myc oncogene are present in 15% of primary human multiple myeloma tumors. Blood 2001; 98: 3082–3086.
Chesi M, Nardini E, Brents LA, Schrock E, Ried T, Kuehl WM et al. Frequent translocation t(4;14)(p16.3;q32.3) in multiple myeloma is associated with increased expression and activating mutations of fibroblast growth factor receptor 3. Nat Genet 1997; 16: 260–264.
Zhan F, Huang Y, Colla S, Stewart JP, Hanamura I, Gupta S et al. The molecular classification of multiple myeloma. Blood 2006; 108: 2020–2028.
Chng WJ, Kumar S, VanWier S, Ahmann G, Price-Troska T, Henderson K et al. Molecular dissection of hyperdiploid multiple myeloma by gene expression profiling. Cancer Res 2007; 67: 2982–2989.
Avet-Loiseau H, Leleu X, Roussel M, Moreau P, Guerin-Charbonnel C, Caillot D et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol 2010; 28: 4630–4634.
Avet-Loiseau H, Attal M, Moreau P, Charbonnel C, Garban F, Hulin C et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myelome. Blood 2007; 109: 3489–3495.
Hanamura I, Stewart JP, Huang Y, Zhan F, Santra M, Sawyer JR et al. Frequent gain of chromosome band 1q21 in plasma-cell dyscrasias detected by fluorescence in situ hybridization: incidence increases from MGUS to relapsed myeloma and is related to prognosis and disease progression following tandem stem-cell transplantation. Blood 2006; 108: 1724–1732.
Reece D, Song KW, Fu T, Roland B, Chang H, Horsman DE et al. Influence of cytogenetics in patients with relapsed or refractory multiple myeloma treated with lenalidomide plus dexamethasone: adverse effect of deletion 17p13. Blood 2009; 114: 522–525.
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med 2008; 359: 906–917.
Richelda R, Ronchetti D, Baldini L, Cro L, Viggiano L, Marzella R et al. A novel chromosomal translocation t(4; 14)(p16.3; q32) in multiple myeloma involves the fibroblast growth-factor receptor 3 gene. Blood 1997; 90: 4062–4070.
Chesi M, Nardini E, Lim RS, Smith KD, Kuehl WM, Bergsagel PL . The t(4;14) translocation in myeloma dysregulates both FGFR3 and a novel gene, MMSET, resulting in IgH/MMSET hybrid transcripts. Blood 1998; 92: 3025–3034.
Fonseca R, Oken MM, Greipp PR, Eastern Cooperative Oncology Group Myeloma Group. The t(4;14)(p16.3;q32) is strongly associated with chromosome 13 abnormalities in both multiple myeloma and monoclonal gammopathy of undetermined significance. Blood 2001; 98: 1271–1272.
Lopez-Corral L, Gutierrez NC, Vidriales MB, Mateos MV, Rasillo A, Garcia-Sanz R et al. The progression from MGUS to smoldering myeloma and eventually to multiple myeloma involves a clonal expansion of genetically abnormal plasma cells. Clin Cancer Res 2011; 17: 1692–1700.
Santra M, Zhan F, Tian E, Barlogie B, Shaughnessy J . A subset of multiple myeloma harboring the t(4;14)(p16;q32) translocation lacks FGFR3 expression but maintains an IGH/MMSET fusion transcript. Blood 2003; 101: 2374–2376.
Keats JJ, Maxwell CA, Taylor BJ, Hendzel MJ, Chesi M, Bergsagel PL et al. Overexpression of transcripts originating from the MMSET locus characterizes all t(4;14)(p16;q32)-positive multiple myeloma patients. Blood 2005; 105: 4060–4069.
Martinez-Garcia E, Popovic R, Min DJ, Sweet SM, Thomas PM, Zamdborg L et al. The MMSET histone methyl transferase switches global histone methylation and alters gene expression in t(4;14) multiple myeloma cells. Blood 2011; 117: 211–220.
Pei H, Zhang L, Luo K, Qin Y, Chesi M, Fei F et al. MMSET regulates histone H4K20 methylation and 53BP1 accumulation at DNA damage sites. Nature 2011; 470: 124–128.
Hudlebusch HR, Santoni-Rugiu E, Simon R, Ralfkiaer E, Rossing HH, Johansen JV et al. The histone methyltransferase and putative oncoprotein MMSET is overexpressed in a large variety of human tumors. Clin Cancer Res 2011; 17: 2919–2933.
Intini D, Baldini L, Fabris S, Lombardi L, Ciceri G, Maiolo AT et al. Analysis of FGFR3 gene mutations in multiple myeloma patients with t(4;14). Br J Haematol 2001; 114: 362–364.
Ronchetti D, Greco A, Compasso S, Colombo G, Dell'Era P, Otsuki T et al. Deregulated FGFR3 mutants in multiple myeloma cell lines with t(4;14): comparative analysis of Y373C, K650E and the novel G384D mutations. Oncogene 2001; 20: 3553–3562.
Onwuazor ON, Wen XY, Wang DY, Zhuang L, Masih-Khan E, Claudio J et al. Mutation, SNP, and isoform analysis of fibroblast growth factor receptor 3 (FGFR3) in 150 newly diagnosed multiple myeloma patients. Blood 2003; 102: 772–773.
Vatsveen TK, Brenne AT, Dai HY, Waage A, Sundan A, Borset M . FGFR3 is expressed and is important for survival in INA-6, a human myeloma cell line without a t(4;14). Eur J Haematol 2009; 83: 471–476.
Quintero-Rivera F, El-Sabbagh Badr R, Rao PN . FGFR3 amplification in the absence of IGH@-FGFR3 fusion t(4;14) in myeloma. Cancer Genet Cytogenet 2009; 195: 92–93.
Turner N, Grose R . Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer 2010; 10: 116–129.
Zhang X, Ibrahimi OA, Olsen SK, Umemori H, Mohammadi M, Ornitz DM . Receptor specificity of the fibroblast growth factor family. J Biol Chem 2006; 281: 15694–15700.
Courjal F, Cuny M, Simony-Lafontaine J, Louason G, Speiser P, Zeillinger R et al. Mapping of DNA amplifications at 15 chromosomal localizations in 1875 breast tumors: definition of phenotypic groups. Cancer Res 1997; 57: 4360–4367.
Dutt A, Salvesen HB, Chen TH, Ramos AH, Onofrio RC, Hatton C et al. Drug-sensitive FGFR2 mutations in endometrial carcinoma. Proc Natl Acad Sci USA 2008; 105: 8713–8717.
Cappellen D, De Oliveira C, Ricol D, de Medina S, Bourdin J, Sastre-Garau X et al. Frequent activating mutations of FGFR3 in human bladder and cervix carcinomas. Nat Genet 1999; 23: 18–20.
Munro NP, Knowles MA . Fibroblast growth factors and their receptors in transitional cell carcinoma. J Urol 2003; 169: 675–682.
Otsuki T, Yamada O, Yata K, Sakaguchi H, Kurebayashi J, Nakazawa N et al. Expression of fibroblast growth factor and FGF-receptor family genes in human myeloma cells, including lines possessing t(4;14)(q16.3;q32. 3) and FGFR3 translocation. Int J Oncol 1999; 15: 1205–1212.
Li Z, Zhu YX, Plowright EE, Bergsagel PL, Chesi M, Patterson B et al. The myeloma-associated oncogene fibroblast growth factor receptor 3 is transforming in hematopoietic cells. Blood 2001; 97: 2413–2419.
Qing J, Du X, Chen Y, Chan P, Li H, Wu P et al. Antibody-based targeting of FGFR3 in bladder carcinoma and t(4;14)-positive multiple myeloma in mice. J Clin Invest 2009; 119: 1216–1229.
Neben K, Jauch A, Bertsch U, Heiss C, Hielscher T, Seckinger A et al. Combining information regarding chromosomal aberrations t(4;14) and del(17p13) with the International Staging System classification allows stratification of myeloma patients undergoing autologous stem cell transplantation. Haematologica 2010; 95: 1150–1157.
Greipp PR, San Miguel J, Durie BG, Crowley JJ, Barlogie B, Blade J et al. International staging system for multiple myeloma. J Clin Oncol 2005; 23: 3412–3420.
Chang H, Sloan S, Li D, Zhuang L, Yi QL, Chen CI et al. The t(4;14) is associated with poor prognosis in myeloma patients undergoing autologous stem cell transplant. Br J Haematol 2004; 125: 64–68.
Fonseca R, Oken MM, Harrington D, Bailey RJ, Van Wier SA, Henderson KJ et al. Deletions of chromosome 13 in multiple myeloma identified by interphase FISH usually denote large deletions of the q arm or monosomy. Leukemia 2001; 15: 981–986.
Loiseau HA, Attal M, Moreau P, Charbonnel C, Garban F, Harousseau J et al. A comprehensive analysis of cytogenetic abnormalities in myeloma: Results of the FISH analysis of 1000 patients enrolled in the IFM99 trials. Blood 2005; 106: 622.
Karlin L, Soulier J, Chandesris O, Choquet S, Belhadj K, Macro M et al. Clinical and biological features of t(4;14) multiple myeloma: a prospective study. Leuk Lymphoma 2011; 52: 238–246.
Jaksic W, Trudel S, Chang H, Trieu Y, Qi X, Mikhael J et al. Clinical outcomes in t(4;14) multiple myeloma: a chemotherapy-sensitive disease characterized by rapid relapse and alkylating agent resistance. J Clin Oncol 2005; 23: 7069–7073.
Avet-Loiseau H, Soulier J, Fermand JP, Yakoub-Agha I, Attal M, Hulin C et al. Impact of high-risk cytogenetics and prior therapy on outcomes in patients with advanced relapsed or refractory multiple myeloma treated with lenalidomide plus dexamethasone. Leukemia 2010; 24: 623–628.
Chang H, Trieu Y, Qi X, Xu W, Stewart KA, Reece D . Bortezomib therapy response is independent of cytogenetic abnormalities in relapsed/refractory multiple myeloma. Leuk Res 2007; 31: 779–782.
Pineda-Roman M, Zangari M, Haessler J, Anaissie E, Tricot G, van Rhee F et al. Sustained complete remissions in multiple myeloma linked to bortezomib in total therapy 3: comparison with total therapy 2. Br J Haematol 2008; 140: 625–634.
Barlogie B, Anaissie E, van Rhee F, Haessler J, Hollmig K, Pineda-Roman M et al. Incorporating bortezomib into upfront treatment for multiple myeloma: early results of total therapy 3. Br J Haematol 2007; 138: 176–185.
Kumar SK, Mikhael JR, Buadi FK, Dingli D, Dispenzieri A, Fonseca R et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines. Mayo Clin Proc 2009; 84: 1095–1110.
Schilling G, Hansen T, Shimoni A, Zabelina T, Perez-Simon JA, Gutierrez NC et al. Impact of genetic abnormalities on survival after allogeneic hematopoietic stem cell transplantation in multiple myeloma. Leukemia 2008; 22: 1250–1255.
Dawson MA, Opat SS, Taouk Y, Donovan M, Zammit M, Monaghan K et al. Clinical and immunohistochemical features associated with a response to bortezomib in patients with multiple myeloma. Clin Cancer Res 2009; 15: 714–722.
Paterson JL, Li Z, Wen XY, Masih-Khan E, Chang H, Pollett JB et al. Preclinical studies of fibroblast growth factor receptor 3 as a therapeutic target in multiple myeloma. Br J Haematol 2004; 124: 595–603.
Trudel S, Li ZH, Wei E, Wiesmann M, Chang H, Chen C et al. CHIR-258, a novel, multitargeted tyrosine kinase inhibitor for the potential treatment of t(4;14) multiple myeloma. Blood 2005; 105: 2941–2948.
Trudel S, Ely S, Farooqi Y, Affer M, Robbiani DF, Chesi M et al. Inhibition of fibroblast growth factor receptor 3 induces differentiation and apoptosis in t(4;14) myeloma. Blood 2004; 103: 3521–3528.
Trudel S, Stewart AK, Rom E, Wei E, Li ZH, Kotzer S et al. The inhibitory anti-FGFR3 antibody, PRO-001, is cytotoxic to t(4;14) multiple myeloma cells. Blood 2006; 107: 4039–4046.
Xin X, Abrams TJ, Hollenbach PW, Rendahl KG, Tang Y, Oei YA et al. CHIR-258 is efficacious in a newly developed fibroblast growth factor receptor 3-expressing orthotopic multiple myeloma model in mice. Clin Cancer Res 2006; 12: 4908–4915.
Bisping G, Wenning D, Kropff M, Gustavus D, Müller-Tidow C, Stelljes M et al. Bortezomib, dexamethasone, and fibroblast growth factor receptor 3–specific tyrosine kinase inhibitor in t(4;14) myeloma. Clin Cancer Res 2009; 15: 520–531.
Sharkey J, Khong T, Spencer A . PKC412 demonstrates JNK-dependent activity against human multiple myeloma cells. Blood 2007; 109: 1712–1719.
Lee SH, Lopes de Menezes D, Vora J, Harris A, Ye H, Nordahl L et al. In vivo target modulation and biological activity of CHIR-258, a multitargeted growth factor receptor kinase inhibitor, in colon cancer models. Clin Cancer Res 2005; 11: 3633–3641.
Sarker D, Molife R, Evans TR, Hardie M, Marriott C, Butzberger-Zimmerli P et al. A phase I pharmacokinetic and pharmacodynamic study of TKI258, an oral, multitargeted receptor tyrosine kinase inhibitor in patients with advanced solid tumors. Clin Cancer Res 2008; 14: 2075–2081.
Acknowledgements
Financial support for medical editorial assistance was provided by Novartis Pharmaceuticals. We thank William Fazzone, Leah Bernstein and Nicole Parker, ArticulateScience, for their medical editorial assistance with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Spencer has participated in scientific advisory boards and received compensation from Novartis, Janssen, Celgene and Merck Sharp & Dohme. He also has participated in speakers bureaus for Novartis. Dr Kalff declares no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kalff, A., Spencer, A. The t(4;14) translocation and FGFR3 overexpression in multiple myeloma: prognostic implications and current clinical strategies. Blood Cancer Journal 2, e89 (2012). https://doi.org/10.1038/bcj.2012.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2012.37
Keywords
This article is cited by
-
Molecular characterization stratifies VQ myeloma cells into two clusters with distinct risk signatures and drug responses
Oncogene (2023)
-
Multiple myeloma, a quintessential malignant disease of aging: a geroscience perspective on pathogenesis and treatment
GeroScience (2023)
-
High-risk disease in newly diagnosed multiple myeloma: beyond the R-ISS and IMWG definitions
Blood Cancer Journal (2022)
-
Ponatinib sensitizes myeloma cells to MEK inhibition in the high-risk VQ model
Scientific Reports (2022)
-
Exploiting gene dependency to inform drug development for multiple myeloma
Scientific Reports (2022)