Abstract
Purpose:
Stargardt disease (STGD) is the most prevalent juvenile macular dystrophy, and it has been associated with mutations in the ABCRgene, encoding a photoreceptor-specific transport protein. In this study, we determined the mutation spectrum in the ABCRgene in a group of Italian STGD patients.
Methods:
The DNA samples of 71 Italian patients (from 62 independent pedigrees), affected with autosomal recessive STGD, were analysed for mutations in all 50 exons of the ABCRgene by the DHPLC approach (with optimization of the DHPLC conditions for mutation analysis) and direct sequencing techniques.
Results:
In our group of STGD patients, 71 mutations were identified in 68 patients with a detection rate of 95.7%. Forty-three mutations had been already reported in the literature, whereas 28 mutations had not been previously described and were not detected in 150 unaffected control individuals of Italian origin. Missense mutations represented the most frequent finding (59.2%); G1961E was the most common mutation and it was associated with phenotypes in various degrees of severity.
Conclusions:
Some novel mutations in the ABCRgene were reported in a group of Italian STGD patients confirming the extensive allelic heterogeneity of this gene—probably related to the vast number of exons that favours rearrangements in the DNA sequence.
Similar content being viewed by others
Introduction
Stargardt disease (STGD), the most prevalent inherited juvenile macular dystrophy, is a progressive juvenile-to-young-adult onset macular degeneration characterized by severe reduction of central visual acuity and normal peripheral vision.1, 2 The onset of the disease occurs usually around 10 years of age, and the first symptom is a reduction of central visual acuity. Rare late clinical pictures, appearing even after 50 years of age, have also been described.3
STGD is distinguished by a diffuse accumulation of toxic metabolites (lipofuscins) within the retinal pigment epithelium (RPE) with consequent disomogeneity and focal hypertrophy of the same RPE, and subsequent photoreceptors atrophy.4
Fundoscopy usually manifests a macular atrophy, often associated with typical fishtail white-yellowish spots spread at the posterior pole, and sometimes at retinal midperiphery (flecks). In the past, the presence of flecks was considered a well-marked disease (‘fundus flavimaculatus’), which could be associated or not with atrophic maculopathy. Currently, macular atrophy and fundus flavimaculatus (and their possible association) are considered variants of the basically same disease.3
Fluorangiography often reveals a homogeneous dark aspect of the choroid (‘dark or silent choroid’), determined by the masking effect of lipofuscin storage in RPE on the underlying choroidal fluorescence. ERG abnormalities can be recorded in advanced stages of the disease.
Stargardt disease is predominantly inherited as an autosomal recessive trait; however, autosomal dominant forms have been described. It has been associated with alterations in the gene encoding the photoreceptor-specific ATP-binding cassette (ABC) transporter (ABCR). This gene (OMIM no. 601691) is localized in chromosome 1p22, and it codes for a 2.273 amino-acid protein expressed in the rims of rod and cone outer segment disks.5 As with other ABC transporters, ABCR consists of a consensus ATP-binding region of approximately 90–110 amino acids, which includes two Walker motifs (A and B regions), a linker or dodecapeptide region, which lies between these Walker motifs (also known as the C region) and some additional regions of homology upstream and downstream from the Walker A and B motifs. Although A, B, and C regions are well conserved across all known organisms, they are usually associated with less conserved transmembrane (TM) domains consisting of six TM helices, which confer substrate specificity.6, 7
ABCR is a transport protein located in the rim of photoreceptor discs and involved in the transport of all-trans-retinal through the disc membrane, and then from the disc lumen to the photoreceptor cytoplasm. ABCR dysfunction reveals an accumulation of all-trans-retinal in the photoreceptors discs and in the RPE. All-trans-retinal is then converted into a substance called A2-E, a major component of lipofuscin, which determines a toxic effect leading to the disruption of the RPE and the overlying photoreceptors.8
Several series of mutation analyses have confirmed that homozygous and compound heterozygous mutations in ABCR are responsible for recessive STGD.9, 10, 11, 12, 13
ABCR has also been singled out as a possible cause of other diseases with similar clinical macular abnormalities. Gene mutations have been observed in families manifesting cone-rod dystrophy,14 retinitis pigmentosa,15 and age-related macular degeneration (AMD).16
All studies investigating ABCR in eye diseases report a broad mutation spectrum and high allelic heterogeneity. This phenomenon might be due to the long gene sequence (50 exons) and to ethnic variability.
ABCR mutations in STGD have been investigated in several different ethnic groups. Italian STGD patients had been analysed for ABCR mutations in three earlier studies. The first study considered 11 families coming from southern Italy,10 and the second studied 36 families originating from various regions of northern, central, and southern Italy.11 In addition, another study on an Italian sample considered only patients with biallelic disease mutations for a genotype–phenotype correlation.17
In this study, the mutation spectrum of the ABCR gene was determined in another group of Italian patients affected with autosomal recessive STGD. Our series consisted of 62 families, originating for the most part from the central Italy. Consequently, it can be said that our sequence represents a large and homogeneous sampling.
Materials and methods
Clinical evaluation
Sixty-two Italian families, some members of which were affected by autosomal recessive STGD, were recruited through the Hereditary Retinal Degenerations Referral Center of the Eye Clinic, University of Florence.
Criteria for the STGD phenotype included the following: (1) juvenile-to-adult symptom onset; (2) bilateral central vision loss; (3) macular dystrophy and/or atrophy (beaten bronze appearance or large patch of atrophy); (4) normal calibre of retinal vessels; (5) absence of pigmented bone spicules; and (6) normal electroretinogram.
The fluorangiographic phenomenon of ‘dark choroid’ and the presence of yellow-white flecks were not considered among the obligatory inclusion criteria, even if they could be appreciated in most of the patients in our series.
Seventy-one patients with a clinical diagnosis of STGD were included in the study (40 males and 31 females). The mean age was 36.6 years (±15.8 years); (range: 10–75 years); visual acuity ranged from 1/30 to 8/10, with an average value of 2.31/10 (±1.9/10). In 48 patients, fundoscopy confirmed the presence of flecks at the posterior pole, whereas in 40 patients, the phenomenon of dark choroid could be observed during the fluorangiographic examination.
DNA extraction and PCR amplification
After obtaining the written informed consent and a complete family history, 10 ml of peripheral blood taken from the antecubital vein using EDTA-containing vials were collected. DNA was extracted from 200 l of peripheral blood with Biorobot EZ1 (Qiagen GmbH, Hilden, Germany).
Coding regions, intron/exon boundaries, and 5′ and 3′ regions of ABCR were amplified in 50 reactions. The PCR amplification was performed using the Core System-Robotic Station (Beckman Coulter, CA, USA). Cycling parameters for each reaction were optimized for all the exons.
The PCR amplification of 50 exons and flanking intronic regions of the ABCR gene was performed using 50–100 ng of genomic DNA. The primers used were those recommended in Rivera et al.,9 and are exhibited in Table 1.
Amplification was performed in 50 mmol/l KCl, 10 mmol/l Tris-HCl, pH 8.3, 5 mmol/l MgCl2, 200 μmol/l dNTPs, and 0.5 μmol/l for each primer set. AmpliTAq DNA polymerase (1 U; Ampli TAq Gold, Applied Biosystems, Foster City, CA, USA) was added for each 25 μl reaction. PCR was performed by employing a multiblock MWG PCR System. Cycling parameters for the reactions were optimized for each exon.
Mutational analysis
Sequence variations were detected by denaturing high-performance liquid chromatography (DHPLC) using the WAVE™ DNA Fragment Analysis System equipped with a DNAsep column (Transgenomics, San Jose, CA, USA).18, 19 The conditions for DHPLC were developed on the basis of exon-specific melting profiles predicted by NAVIGATOR™ Software. PCR products were examined for heteroduplexes by subjecting 5 μl of each PCR product to a denaturation step process (5 min at 95°C), followed by a renaturing step (30 min at 37°C). The PCR products were then separated through a 5% linear acetonitrile gradient. Commercially available WAVE Optimized™ buffers (A, B, and D) and Syringe Solution (Transgenomics) were used to provide highly reproducible retention times. Samples showing heteroduplex by DHPLC were finally sequenced on an automated sequencing system (ABI Prism 3100 genetic Analyser) using Big Dye Terminator chemistry (Applied Biosystems). PCR products were purified according to QIAquick PCR Purification Kit (Quiagen GmbH). Finally, data obtained from the Sequence Analysis Software (Applied Biosystems) were aligned with the wild-type ABCR gene sequence (GenBank database; http://www.ebi.ac.uk/). According to the EMQN Best Practice Guidelines, a sequence mismatch was considered as a disease-causing mutation only if it is absent in 150 healthy controls,18, 19, 20 associated with amino-acidic change, confirmed by a new independent PCR, and, whenever possible, by restriction enzyme digestion. As a final point, the degree of evolutionary conservation of the affected residue, directly related to its importance in the functional protein structure, was assessed by interspecies amino-acid alignment analysis.
Results
Seventy-one Italian patients with a diagnosis of STGD (from 62 independent pedigrees) were clinically examined. DNA samples of the affected individuals were analysed for mutations in all 50 exons of the ABCR gene by DHPLC approach and by direct sequencing techniques. Seventy-one mutations were identified in 68 patients with a detection rate of 95.7%. Forty-three mutations had already been reported in the literature,5, 10, 11, 12, 13, 14, 17, 18, 19, 20, 21, 22, 23, 24 whereas 28 mutations had not been and, further, were not detected in 150 unaffected control individuals (300 chromosomes) of Italian origin.18, 19, 20 The mutations identified in our series are reported in Table 2.
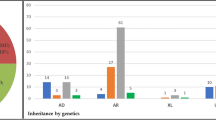
Forty-two mutations (59.2%) were missense mutations, 10 (14.1%) were nonsense mutations, 9 (12.6%) were splice mutations, and 10 (14.1%) were frameshift mutations.
The majority of patients (42/71, 59.1%) were compound heterozygotes for two missense mutations or one nonsense and one missense mutations, and 12 patients (16.9%) were simple heterozygotes. Only three patients were found to be homozygous for ABCR variants (324-327insT, V1433I, and A1598D). Potential complex alleles were identified in 11 patients (15.5%). Unfortunately, because of a lack of parental DNA, the exact genotype was not determined in nine cases.
G1961E was the most common mutated allele among our STGD patients of Italian origin. It was found, always in heterozygosis, in 40.8% of our series (29/71; and then in 20.4% of our STGD alleles). The next most common mutated allele was the splicing mutation IVS40+5G → A, reported, always in heterozygosis, in 8.4% (6/71) of our series (and then in 4.2% of our STGD alleles). In our series, the detected mutations occurred with equal frequency in predicted conserved regions and in non-conserved regions.
Thirty different alterations were present in >1% of the control alleles and were classified as polymorphisms (Table 3).
Discussion
We have optimized DHPLC conditions for mutation analysis of all 50 exons of the ABCR gene in a study group of Italian STGD patients.
In 95.7% of STGD patients (68/71), we reported some mutations of the ABCR gene. This detection rate is in conformity with Fumagalli et al11 (94.4%), and it is somewhat higher than Simonelli et al10 (73%).
This might be due to mild technological differences in mutation analysis, to the strict clinical inclusion criteria, and/or to the lack of a functional analysis to select disease-causing mutations.
In our series, we detected 71 mutations. Missense mutations made up the majority (59.2%), followed by nonsense (14.1%) and frameshift (14.1%) mutations. Splicing mutations represented 12.6%. These data are in agreement with the results of earlier investigations in the Italian population and with other studies in a sizeable series of patients.9, 12, 25
We identified 28 novel ABCR mutations, confirming and further highlighting the high heterogeneity of the ABCR gene in STGD. The frequent report of novel mutations is probably related to the enormous number of exons in the ABCR gene, which favours rearrangement in the DNA sequence.
The majority of patients (59.1%) were compound heterozygotes. Only three patients were found to be homozygous for variants. A single disease allele was found in 16.9% of our series. No disease allele was reported in 4.3% of our patients. Potential complex alleles were identified in 11 patients (15.5%). Possible unidentified mutations might be located in parts of the gene that had not been screened; alternatively, our investigation technique could have failed to detect certain variations. The possible influence of modifier genes in the clinical expression of the ABCR gene variants must be considered.
Concurring with earlier studies,9, 11, 13, 26 ABCR mutant alleles are distributed throughout the entire coding sequence, and no mutational hotspots seem to exist.
In our series, mainly consisting of patients coming from central Italy, G1961E was the most common mutant allele, in congruence with other studies performed in distinct dissimilar European populations.9, 20 Nevertheless, the frequency of G1961E mutation (20.4% of our STGD alleles) was higher than in the other Italian studies where this mutation was detected in 11.110 and 9.7% 11 of the screened alleles.
In earlier reports, G1961E was considered a mutation with a low pathogenetic influence,10, 13 but in our series, it may be associated with STGD phenotypes of a varying severity. Therefore, it can be speculated that its clinical expression depends on the mutation severity on the fellow allele, as suggested by earlier genotype/phenotype studies.17, 21
Still, although the A1038V mutation is commonly reported in the literature,9, 13, 27 in our series, it was detected in only two patients (1.4% of the patients, 0.7% of the alleles) within the L541P-A1038V complex allele. Moreover, in the Italian studies, this mutation was reported in 4.110 and 5.5%11 of the alleles. These data suggest a possible regional distribution of specific mutations.
In our series, the reported mutations occurred with equal frequency in predicted conserved regions and in non-conserved regions. These data underscore the importance of screening the entire coding sequence of the ABCR to search for mutant alleles and not merely to seek out that portion predicted to encode conserved domains.
Affected members of the same family occasionally showed variable phenotypes (various age of onset, different visual loss severity, presence of flecks, or dark choroid), in agreement with some earlier reports of reduced penetrance and variable clinical expressivity of the ABCR mutations in STGD.27, 28, 29, 30, 31 The variable expressivity of ABCR mutations might be due to the influence of environmental factors or unknown modificator genes. This suggests that molecular genetic results must be interpreted with caution especially in the context of genetic counselling for family planning.
In our series, the homozygous independent genomes (three unrelated patients) continuously showed a rapidly progressive clinical course, even if with a variable age of onset of the disease (8, 31 and 38 years). The presence of flecks and the phenomenon of dark choroid could be appreciated in all three patients.
In conclusion, 28 novel ABCR mutations were identified in our series of 71 Italian patients with diagnoses of STGD. A concentrated knowledge of the ABCR mutation spectrum, and further information about genotype/phenotype correlations are essential to understand the physiopathology of STGD and to evaluate the chances for patients to be referred to future possible therapeutic options.
References
Fishman GA . Fundus flavimaculatus : a clinical classification. Arch Ophthalmol 1976; 94: 2061–2067.
Gass JDM . Heredodystrophic Disorders Affecting the Pigment Epithelium and Retina. In: Gass JDM (ed). Stereocopic Atlas of Macular Disease. Diagnosis and Treatment. Mosby. St.Louis: London-Phyladelphia-Sidney-Toronto, 1997, pp 303–435.
Rozet JM, Gerber S, Ducroq D, Hamel C, Dufier JL, Kaplan J . Les dystrophies maculaires héréditaires. J Fr Ophtalmol 2005; 28 (1): 113–124.
Birnbach CD, Jarvelainen N, Possim DE, Milam AH . Histopathology and immunochemistry of the neurosensory retina in fundus flavimaculatus. Ophthalmology 1994; 101: 1211–1219.
Allikmets R, Singh N, Shroyer NF, Hutchinson A, Chidambaram A, Gerrard B et al. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat Genet 1997; 15: 236–245.
Stefkova J, Poledine R, Hubacek JA . ATP-binding cassette (ABC) transporters in human metabolism and disease. Physiol Res 2004; 53: 235–243.
Kaminski WE, Piehler A, Wenzel JJ . ABC a-subfamily transporters: structure, function and disease. Biochim Biophys Acta 2006; 1762: 510–524.
Cideciyan AV, Aleman TS, Swider M, Schwartz SB, Steinberg JD, Brucker AJ et al. Mutations in ABCA4 result in accumulation of lipofuscin before slowing of the retinoid cycle: a reappraisal of the human disease sequence. Hum Mol Genet 2004; 13 (5): 525–534.
Rivera A, White K, Stohr H, Steiner K, Hemmrich N, Grimm T et al. A comprehensive survey of sequence variation in the ABCA4 (ABCR) gene in Stargardt disease and age-related macular degeneration. Am J Hum Genet 2000; 67: 800–813.
Simonelli F, Testa F, De Crecchio G, Rinaldi E, Hutchinson A, Atkinson A et al. New ABCR mutations and clinical phenotype in Italian patients with Stargardt disease. Invest Ophthalmol Vis Sci 2000; 41: 892–897.
Fumagalli A, Ferrari M, Soriani N, Gessi A, Foglieni B, Martina E et al. Mutational scanning of the ABCR gene with double-gradient denaturing-gradient gel electrophoresis (DG-DGGE) in Italian Stargardt disease patients. Hum Genet 2001; 109: 326–338.
September AV, Vorsler AA, Ramesar RS, Greenberg LJ . Mutation spectrum and founder chromosomes for the ABCA4 gene in South African patients with Stargardt disease. Invest Ophthalmol Vis Sci 2004; 45 (6): 1705–1711.
Hargitai J, Zernant J, Somfai GM, Vamos R, Farkas A, Salacz G et al. Correlation of clinical and genetic findings in Hungarian patients with Stargardt disease. Invest Ophtahlmol Vis Sci 2005; 46: 4402–4408.
Briggs CE, Rucinski D, Rosenfeld PJ, Hirose T, Berson EL, Dryja TP . Mutations in ABCR (ABCA4) in patients with Stargardt macular degeneration or cone-rod degeneration. Invest Ophthalmol Vis Sci 2001; 42 (10): 2229–2236.
Cremers FPM, Van de Pol DJR, Van Driel M, Den Hollander AI, Van Haren FJJ, Knoers NVAM et al. Autosomal recessive retinitis pigmentosa and cone-rod dystrophy caused by splice site mutations in the Stargardt's disease gene ABCR. Hum Mol Genet 1998; 7 (3): 355–362.
Allikmets R, Shroyer NF, Singh N, Seddon JM, Lewis RA, Bernstein PS et al. Mutation of the Stargardt disease gene (ABCR) in age-related macular degeneration. Science 1997; 277: 1805–1807.
Simonelli F, Testa F, Zernant J, Nesti A, Rossi S, Allikmets R et al. Genotype–phenotype correlation in families with Stargardt disease. Ophthalm Res 2005; 37: 159–167.
Fukui T, Yamamoto S, Nakano K, Tsujikawa M, Morimura H, Nishida K et al. ABCA4 gene mutations in Japanese patients with Stargardt disease and retinitis pigmentosa. Invest Ophthalmol Vis Sci 2002; 43: 2819–2824.
Ozgul R, Durukan H, Tutan A, Oner C, Ogus A, Faber DB . Molecular analysis of the ABCA4 gene in Turkish patients with Stargardt disease and retinitis pigmentosa. Hum Mutat 2004; 23 (5): 523.
Paloma E, Martínez-Mir A, Vilageliu L, Gonzàlez-Duarte R, Balcells S . Spectrum of ABCA4 (ABCR) gene mutations in Spanish patients with autosomal recessive macular dystrophies. Hum Mutat 2001; 17: 504–510.
Gerth C, Andrassi-Darida M, Bock M, Preising MN, Weber BHF, Lorenz B . Phenotypes of 16 Stargardt macular dystrophy/fundus flavimaculatus patients with known ABCA4 mutations and evaluation of genotype-phenotype correlation. Graefe's Arch Clin Exp Ophthalmol 2002; 240: 628–638.
Jaakson K, Zernant J, Kulm M, Hutchinson A, Tonisson N, Glavac D et al. Genotyping microarray (gene chip) for the ABCR (ABCA4) gene. Hum Mutat 2003; 22: 395–403.
Maugeri A, van Driel MA, van de Pol DJ, Klevering BJ, van Haren FJ, Tijmes N et al. The 2588G>C mutation in the ABCR gene is a mild frequent founder mutation in the Western European population and allows the classification of ABCR mutations in patients with Stargardt disease. Am J Hum Genet 1999; 64: 1024–1035.
Papaioannou M, Ocaka L, Bessant D, Lois N, Bird A, Payne A et al. An analysis of ABCR mutations in British patients with recessive retinal dystrophies. Invest Ophthalmol Vis Sci 2000; 41: 16–19.
Oldenburg J, Ivaskevicius V, Rost S, Fregin A, White K, Holinski-Feder E et al. Evaluation of DHPLC in the analysis of hemophilia A. J. Bioochem.Byophys 2001; 47: 39–51.
Xiao W, Oefner PJ . Denaturing high-performance liquid chromatography: a review. Hum Mut 2001; 17: 439–474.
Lewis RA, Shroyer NF, Singh N, Allikmets R, Hutchinson A, Li Y et al. Dean M genotype/phenotype analysis of a photoreceptor-specific ATP-binding cassette transporter gene, ABCR, in Stargardt disease. Am J Hum Genet 1999; 64: 422–434.
Webster AR, Heon E, Lotery AJ, Vandenburgh K, Casavant TL, Oh KT et al. An analysis of allelic variation in the ABCA4 gene. Invest Ophthalmol Vis Sci 2001; 42: 1179–1189.
Shroyer NF, Lewis RA, Lupski JR . Complex inheritance of ABCR mutations in Stargardt disease: linkage disequilibrium, complex alleles, and pseudodominance. Hum Genet 2000; 106: 244–248.
Yatsenko AN, Shroyer NF, Lewis RA, Lupski JR . Late-onset Stargardt disease is associated with missense mutations that map outside known functional regions of ABCR (ABCA4). Hum Genet 2001; 108: 346–355.
Sodi A, Bini A, Passerini I, Puccioni M, Torricelli F, Menchini U . Variable expressivity of ABCA4 gene mutations in an Italian family with Stargardt disease. Retin Cases Brief Rep.
Acknowledgements
This study was supported by a grant from Cassa di Risparmio di Firenze.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Passerini, I., Sodi, A., Giambene, B. et al. Novel mutations in of the ABCR gene in italian patients with Stargardt disease. Eye 24, 158–164 (2010). https://doi.org/10.1038/eye.2009.35
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.35
Keywords
This article is cited by
-
Genetic characteristics of 234 Italian patients with macular and cone/cone-rod dystrophy
Scientific Reports (2022)
-
Genetic landscape of 6089 inherited retinal dystrophies affected cases in Spain and their therapeutic and extended epidemiological implications
Scientific Reports (2021)
-
Genetic characterization of Stargardt clinical phenotype in South Indian patients using sanger and targeted sequencing
Eye and Vision (2020)
-
Searching the second hit in patients with inherited retinal dystrophies and monoallelic variants in ABCA4, USH2A and CEP290 by whole-gene targeted sequencing
Scientific Reports (2018)
-
Dietary profile of patients with Stargardt’s disease and Retinitis Pigmentosa: is there a role for a nutritional approach?
BMC Ophthalmology (2016)