Abstract
OBJECTIVE:
To examine changes in eating behaviors and physical activity, as well as predictors of weight loss success, in obese adults who participated in a 2-year behavioral weight loss intervention conducted in a primary care setting.
DESIGN:
A longitudinal, randomized controlled, multisite trial.
SUBJECTS:
Three hundred ninety obese (body mass index, 30–50 kg m–2) adults, ⩾21 years, in the Philadelphia region.
METHODS:
Participants were assigned to one of three interventions: (1) Usual Care (quarterly primary care provider (PCP) visits that included education on diet and exercise); (2) Brief Lifestyle Counseling (quarterly PCP visits plus monthly lifestyle counseling (LC) sessions about behavioral weight control); or (3) Enhanced Brief LC (the previous intervention with a choice of meal replacements or weight loss medication).
RESULTS:
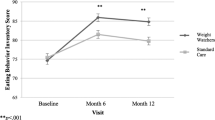
At month 24, participants in both Brief LC and Enhanced Brief LC reported significantly greater improvements in mean (±s.e.) dietary restraint than those in Usual Care (4.4±0.5, 4.8±0.5 and 2.8±0.5, respectively; both P-values⩽0.016). The percentage of calories from fat, along with fruit and vegetable consumption, did not differ significantly among the three groups. At month 24, both the Brief LC and Enhanced Brief LC groups reported significantly greater increases than usual care in energy expenditure (kcal per week) from moderately vigorous activity (+593.4±175.9, +415.4±179.6 and −70.4±185.5 kcal per week, respectively; both P-values⩽0.037). The strongest predictor of weight loss at month 6 (partial R2=33.4%, P<0.0001) and at month 24 (partial R2=19.3%, P<0.001) was food records completed during the first 6 months. Participants who achieved a 5% weight loss at month 6 had 4.7 times greater odds of maintaining a ⩾5% weight loss at month 24.
CONCLUSIONS:
A behavioral weight loss intervention delivered in a primary care setting can result in significant weight loss, with corresponding improvements in eating restraint and energy expenditure. Moreover, completion of food records, along with weight loss at month 6, is a strong predictor of long-term weight loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Tsai A, Wadden TA . Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009; 24: 1073–1079.
Leblanc ES, O'Connor E, Whitlock EP, Patnode CD, Kapka T . Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2012; 155: 434–447.
Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011; 365: 1959–1968.
Bennett GG, Warner ET, Glasgow RE, Askew S, Goldman J, Ritzwoller DP et al. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med 2012; 172: 565–574.
Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med 2011; 365: 1969–1979.
Derbas J, Vetter M, Volger S, Khan Z, Panigrahi E, Tsai AG et al. Improving weight management in primary care practice: a possible role for auxiliary health professionals collaborating with primary care physicians. Obes Weight Manag 2009; 5: 210–215.
Vetter ML, Wadden TA, Lavenberg J, Moore RH, Volger S, Perez JL et al. Relation of health-related quality of life to metabolic syndrome, obesity, depression and comorbid illnesses. Int J Obes 2011; 35: 1087–1094.
Volger S, Vetter ML, Dougherty M, Panigrahi E, Egner R, Webb V et al. Patients' preferred terms for describing their excess weight: discussing obesity in clinical practice. Obesity 2012; 20: 147–150.
Yeh H-C, Clark JM, Emmons KE, Moore RH, Bennett GG, Warner ET et al. Independent but coordinated trials: insights from the Practice-based Opportunities for Weight Reduction Trials Collaborative Research Group. Clin Trials 2010; 7: 322–332.
U.S. Department of Health and Human Services and the U.S. Department of Agriculture. Dietary Guidelines for Americans, 2005 6th edn. U.S. Government Printing Office: Washington, DC, USA, 2005.
Borushek A . The CalorieKing Calorie, Fat and Carbohydrate Counter 8 edn. Family Health: Conta Mesa, CA, USA, 2008.
National Heart Lung, and Blood Institute. Aim for a Healthy Weight. National Institutes of Health: Bethesda, MD, USA, August 2005. (NIH publication no. 05-5213.).
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Stunkard A, Messick S . Eating Inventory Manual. Psychological Corporation: San Antonio, TX, USA, 1988.
Stunkard AJ, Messick S . The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985; 29: 71–83.
Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V . Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Public Health Nutr 2004; 7: 1097–1105.
Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL et al. Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc 2002; 102: 1764–1772.
Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A . Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc 2007; 107: 760–767.
Thompson FE, Midthune D, Williams GC, Yaroch AL, Hurley TG, Resnicow K et al. Evaluation of a short dietary assessment instrument for percentage energy from fat in an intervention study. J Nutr 2008; 138: 193S–199S.
Paffenbarger RS, Wing AL, Hyde RT . Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 1978; 108: 161–175.
Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc 1997; 29: S1–205.
Sebastian RS, Wilkinson Enns C, Goldman JD MYPyramid Intakes and Snacking Patterns of U.S. Adults: What We Eat in America NHANES 2007-2008. In: Food Surveys Research Group Dietary Data Brief No. 5., 2011.
U.S. Department of Health and Human Services and the U.S. Department of Agriculture. Dietary Guidelines for Americans, 2010 7th edn. U.S. Government Printing Office: Washington, DC, USA, 2010.
Berkowitz RI, Wadden TA, Tershakovec AM, Cronquist JL . Behavior therapy and sibutramine for the treatment of adolescent obesity: a randomized controlled trial. JAMA 2003; 289: 1805–1812.
Helsel DL, Jakicic JM, Otto AD . Comparison of techniques for self-monitoring eating and exercise behaviors on weight loss in a correspondence-based intervention. J Am Diet Assoc 2007; 107: 1807–1810.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med 2005; 353: 2111–2120.
Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C . Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med 2001; 161: 218–227.
Burke LE, Wang J, Sevick MA . Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011; 111: 92–102.
Milsom VA, Middleton KM, Perri MG . Successful long-term weight loss maintenance in a rural population. Clin Interv Aging 2011; 6: 303–309.
Astrup A, Rossner S . Lessons from obesity management programmes: greater initial weight loss improves long-term maintenance. Obes Rev 2000; 1: 17–19.
Jeffery RW, Wing RR, Mayer RR . Are smaller weight losses or more achievable weight loss goals better in the long term for obese patients? J Consult Clin Psychol 1998; 66: 641–645.
Stubbs J, Whybrow S, Teixeira P, Blundell J, Lawton C, Westenhoefer J et al. Problems in identifying predictors and correlates of weight loss and maintenance: implications for weight control therapies based on behaviour change. Obes Rev 2011; 12: 688–708.
Fabricatore AN, Wadden TA, Moore RH, Butryn ML, Heymsfield SB, Nguyen AM . Predictors of attrition and weight loss success: results from a randomized controlled trial. Behav Res Ther 2009; 47: 685–691.
Wadden TA, Neiberg RH, Wing RR, Clark JM, Delahanty LM, Hill JO et al. Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity 2011; 19: 1987–1998.
Centers for Medicaid and Medicare Services. Decision memo for intensive behavioral therapy for obesity (CAG-00423N). Available at http://www.cms.gov/medicare-coverage-database/details/nca-decisionmemo.aspx?&NcaName=Intensive%20Behavioral%20Therapy%20for%20Obesity&bc=ACAAAAAAIAAA&NCAId=253. Accessed December 14, 2012.
Moyer VA . Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012; 7326: 0003–4819.
Acknowledgements
We thank Christopher Petro, PhD, for his assistance with data management, and Jeffrey Derbas, BS, Megan Dougherty, BS, Zahra Khan, BA, Joanna Perez, BA, Ilana Schriftman, BA and Dana Tioxon for their assistance with the execution of the research study. This research was supported by grants from the National Heart, Lung, and Blood Institute (U01-HL087072) and National Institute of Diabetes and Digestive and Kidney Diseases (K24-DK065018).
This article is published as part of a supplement, sponsored by the Center for Weight and Eating Disorders—University of Pennsylvania.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
TAW serves on the advisory boards of Novo Nordisk and Orexigen Therapeutics, which are developing weight loss medications, as well as the advisory boards of Alere and the Cardiometabolic Support Network, which provide behavioral weight loss programs. TAW has also served as a consultant for Boehringer Ingelheim, and has received grant support from the National Institutes of Health (NIH/NIDDK and NIH/NHLBI). DBS discloses relationships with the following companies: Allergan, BariMD, BaroNova, Enteromedics and Galderma. DBS has also received grant support from the National Institutes of Health (NIH). The remaining authors declare no conflict of interest.
Appendix
Appendix
POWER-UP Research Group: Investigators and Research Coordinators
Academic investigators at the Perelman School of Medicine at the University of Pennsylvania were Thomas A Wadden, PhD (principal investigator), David B Sarwer, PhD (co-principal investigator), Robert I Berkowitz, MD, Jesse Chittams, MS, Lisa Diewald, MS, RD, Shiriki Kumanyika, PhD, Renee Moore, PhD, Kathryn Schmitz, PhD, Adam G Tsai, MD, MSCE, Marion Vetter, MD and Sheri Volger, MS, RD.
Research coordinators at the University of Pennsylvania were Caroline H Moran, BA, Jeffrey Derbas, BS, Megan Dougherty, BS, Zahra Khan, BA, Jeffrey Lavenberg, MA, Eva Panigrahi, MA, Joanna Evans, BA, Ilana Schriftman, BA, Dana Tioxon, Victoria Webb, BA and Catherine Williams-Smith, BS.
POWER-UP Research Group: Participating Sites and Clinical Investigators
PennCare—Bala Cynwyd Medical Associates: Ronald Barg, MD, Nelima Kute, MD, David Lush, MD, Celeste Mruk, MD, Charles Orellana, MD and Gail Rudnitsky, MD (primary care providers); Angela Monroe (lifestyle coach); Lisa Anderson (practice administrator).
PennCare—Internal Medicine Associates of Delaware County: David E Eberly, MD, Albert H. Fink Jr MD, Kathleen Malone, CRNP, Peter B Nonack, MD, Daniel Soffer, MD, John N Thurman, MD and Marc J Wertheimer, MD (primary care providers); Barbara Jean Shovlin, Lanisha Johnson (lifestyle coaches); Jill Esrey (practice administrator).
PennCare—Internal Medicine Mayfair: Jeffrey Heit, MD, Barbara C Joebstl, MD and Oana Vlad, MD (primary care providers); Rose Schneider, Tammi Brandley (lifestyle coaches); Linda Jelinski (practice administrator).
Penn Presbyterian Medical Associates: Joel Griska, MD, Karen J Nichols, MD, Edward G Reis, MD, James W Shepard, MD and Doris Davis-Whitely, PA (primary care providers); Dana Tioxon (lifestyle coach); Charin Sturgis (practice administrator).
PennCare—University City Family Medicine: Katherine Fleming, CRNP, Dana B Greenblatt, MD, Lisa Schaffer, DO, Tamara Welch, MD and Melissa Rosato, MD (primary care providers); Eugonda Butts, Marta Ortiz, Marysa Nieves and Alethea White (lifestyle coach); Cassandra Bullard (practice administrator).
PennCare—West Chester Family Practice: Jennifer DiMedio, CRNP, Melanie Ice, DO, Brandt Loev, DO, John S Potts, DO and Christine Tressel, DO (primary care providers); Iris Perez, Penny Rancy and Dianne Rittenhouse (lifestyle coaches); Joanne Colligan (practice administrator).
Rights and permissions
About this article
Cite this article
Volger, S., Wadden, T., Sarwer, D. et al. Changes in eating, physical activity and related behaviors in a primary care-based weight loss intervention. Int J Obes 37 (Suppl 1), S12–S18 (2013). https://doi.org/10.1038/ijo.2013.91
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2013.91
Keywords
This article is cited by
-
Dietary intake during a pragmatic cluster-randomized weight loss trial in an underserved population in primary care
Nutrition Journal (2023)
-
Introduction to the POWER-UP supplement
International Journal of Obesity (2013)